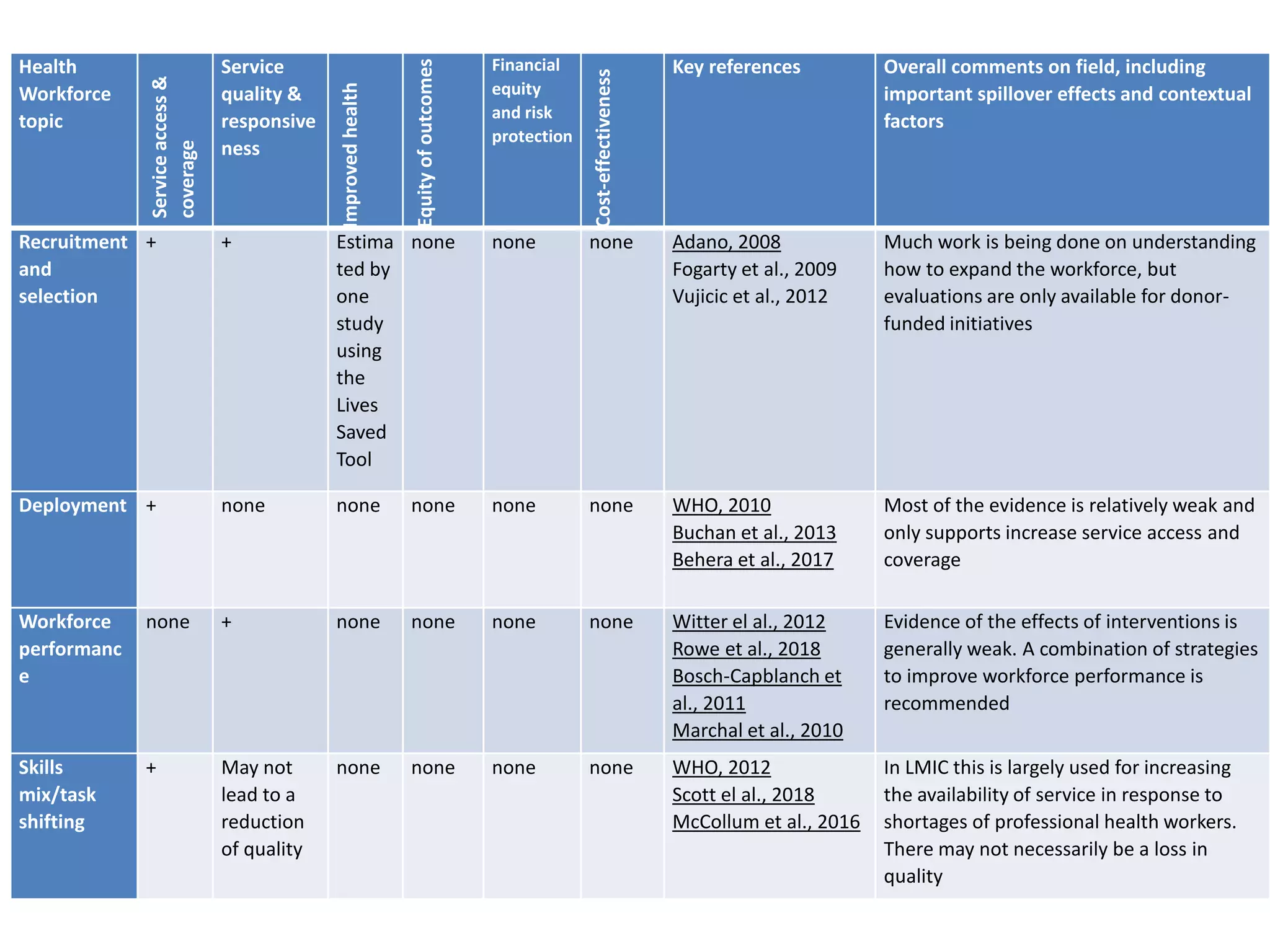
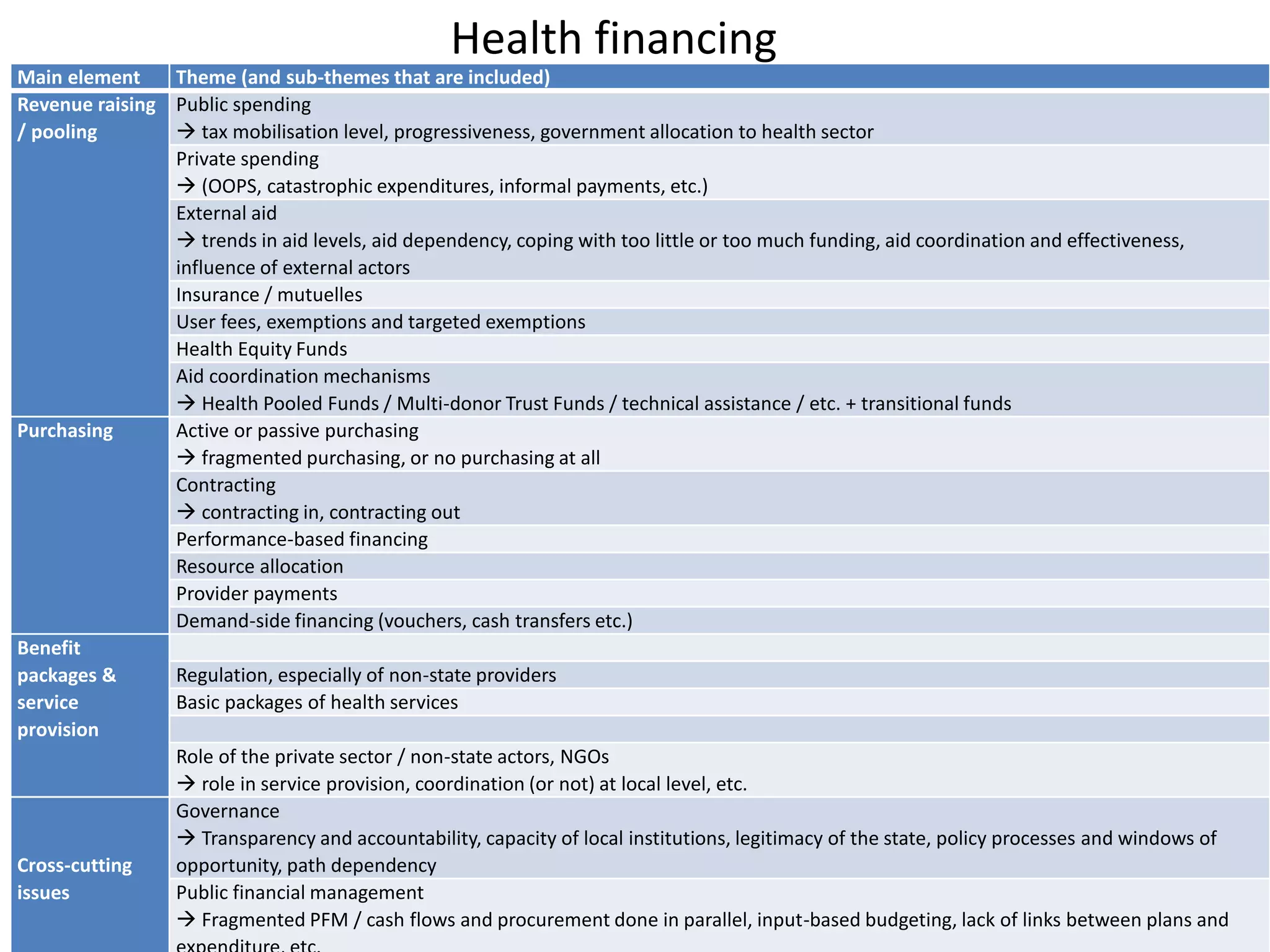
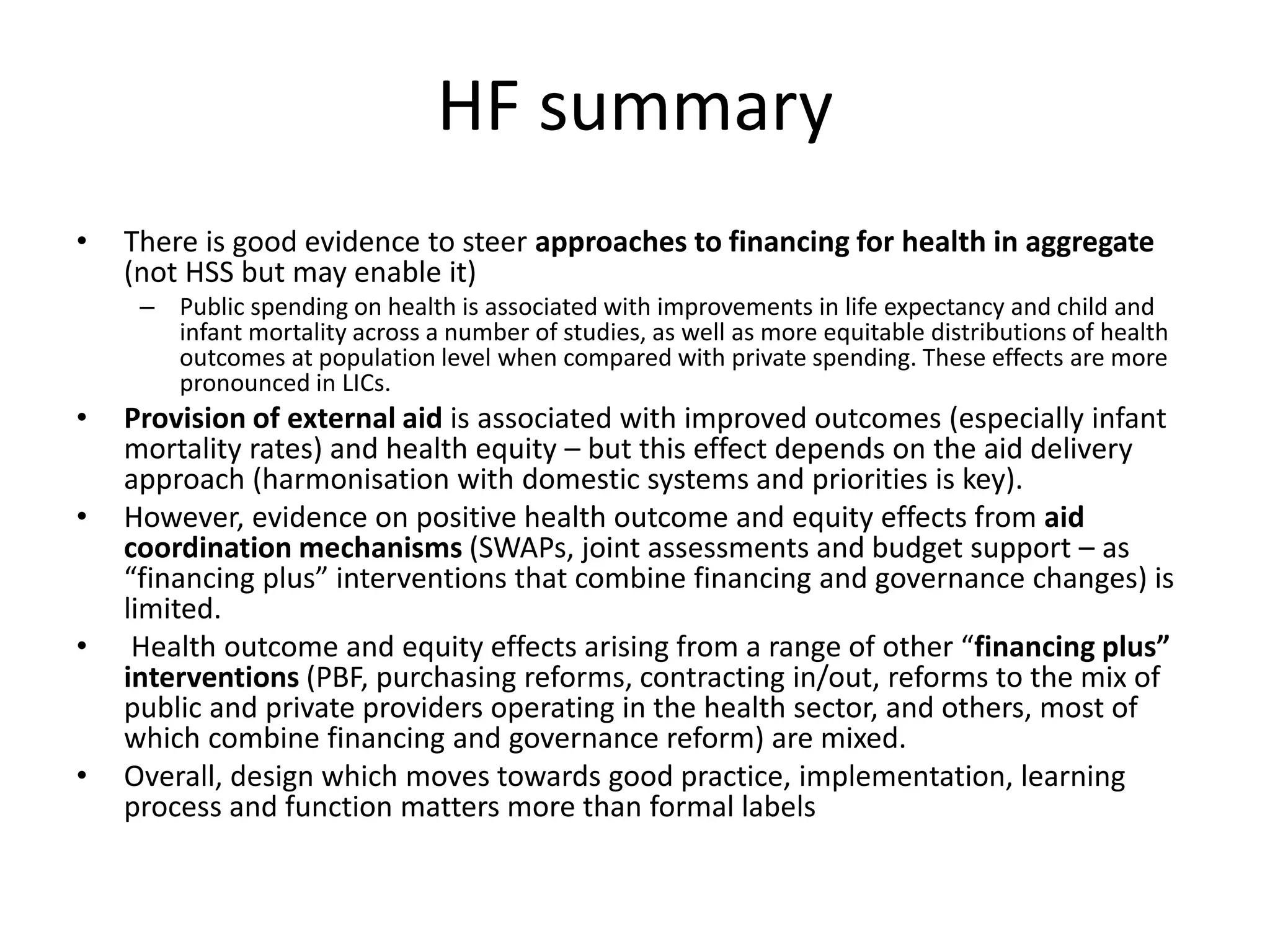
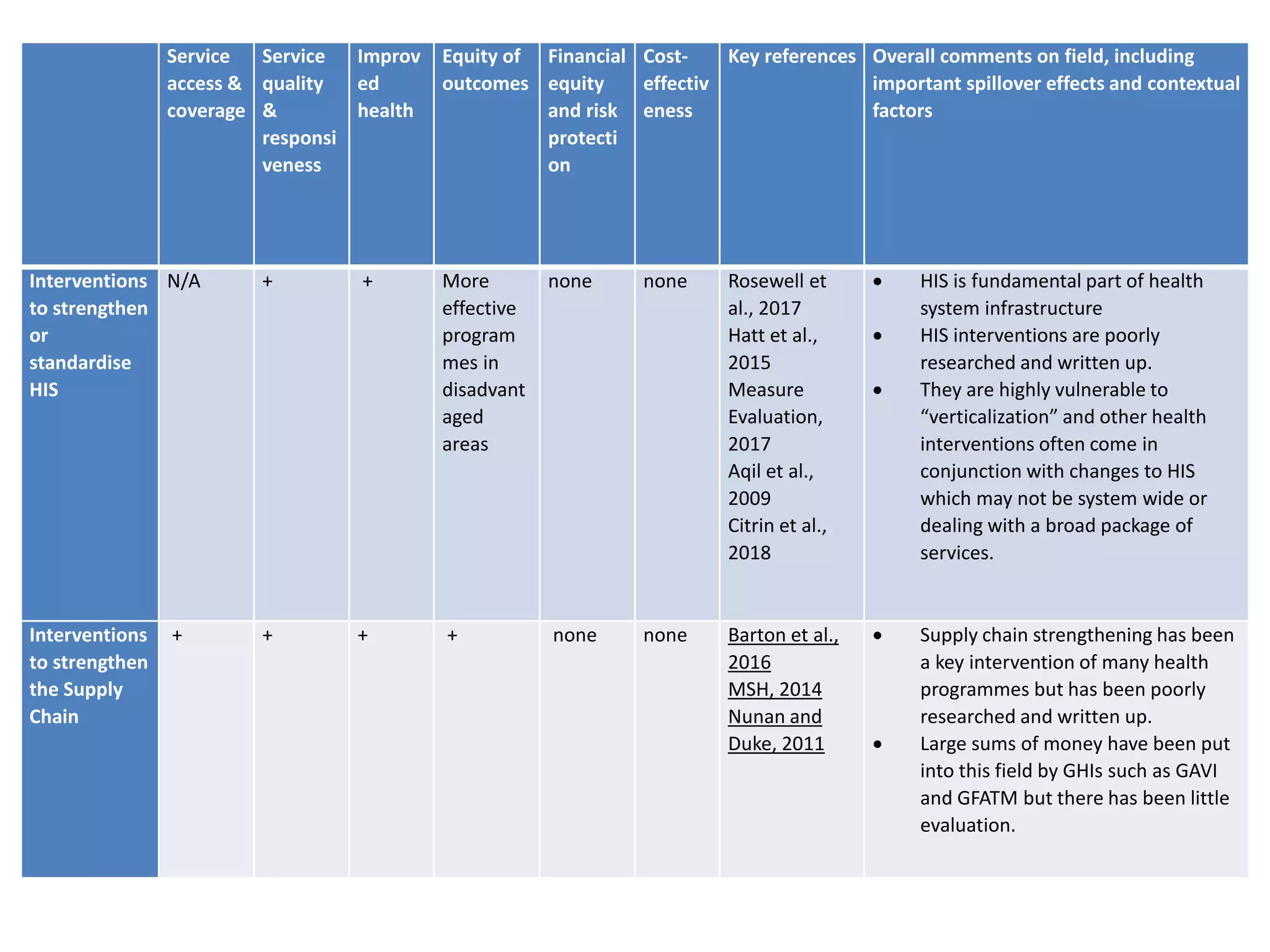
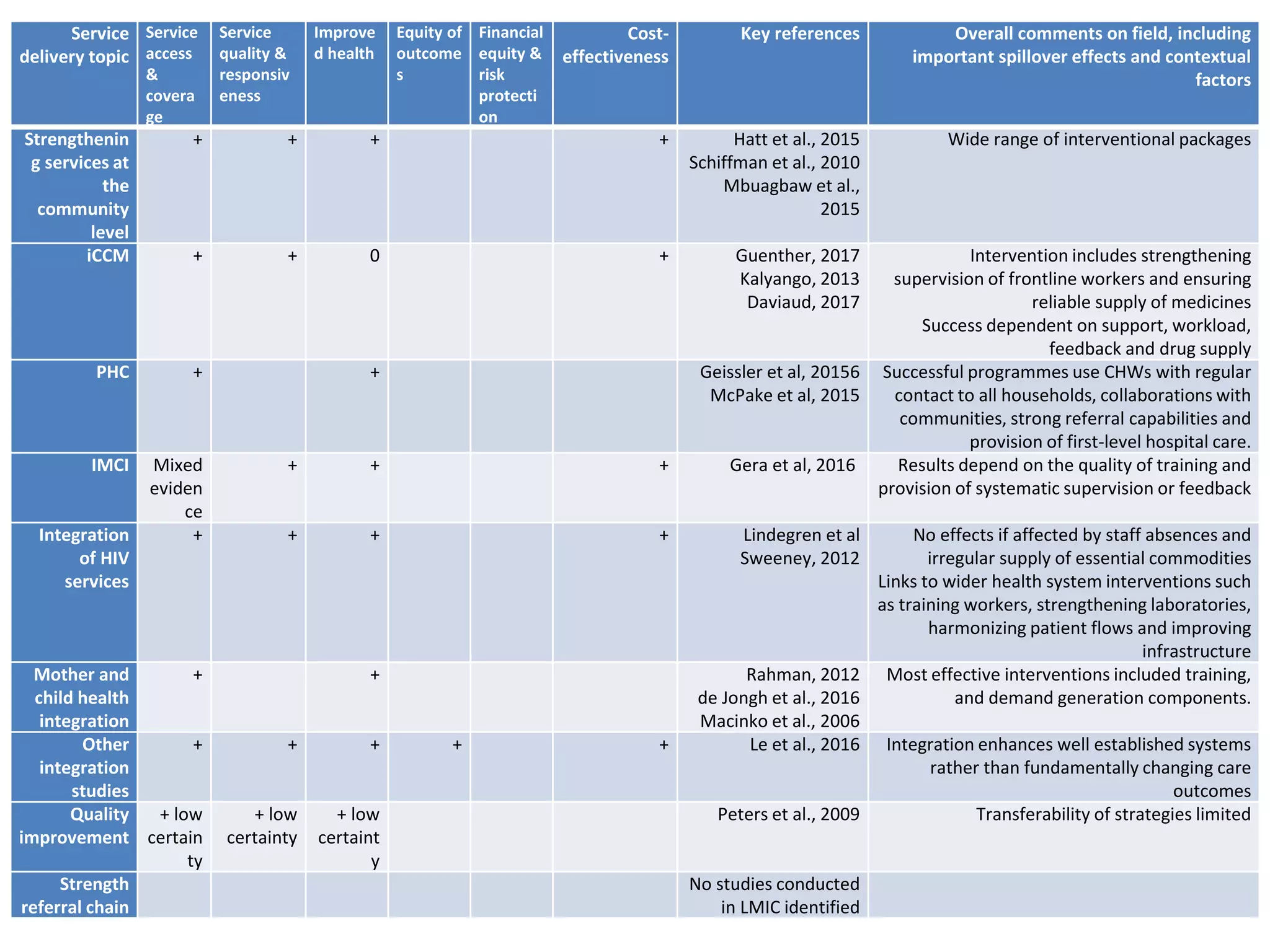
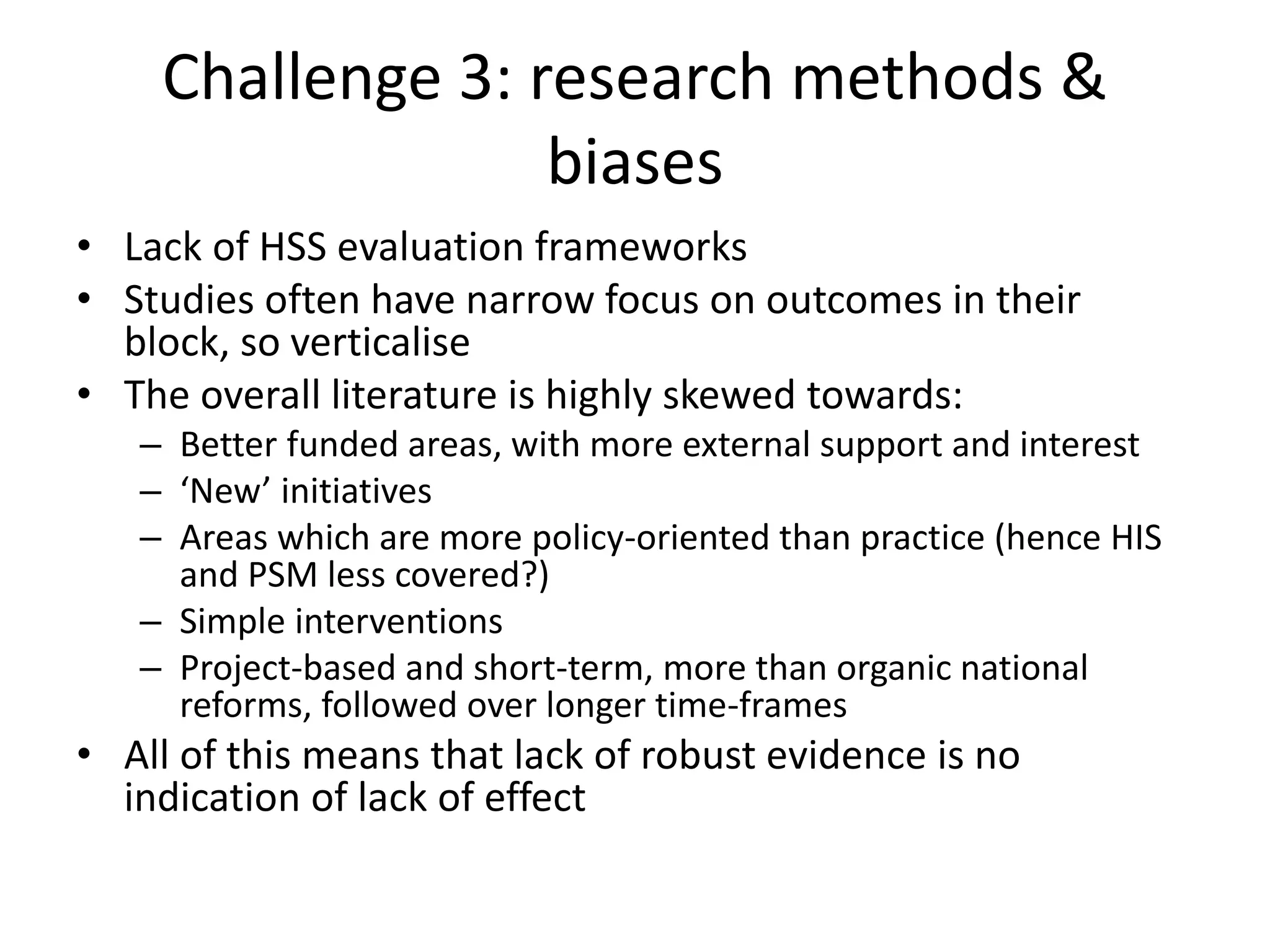
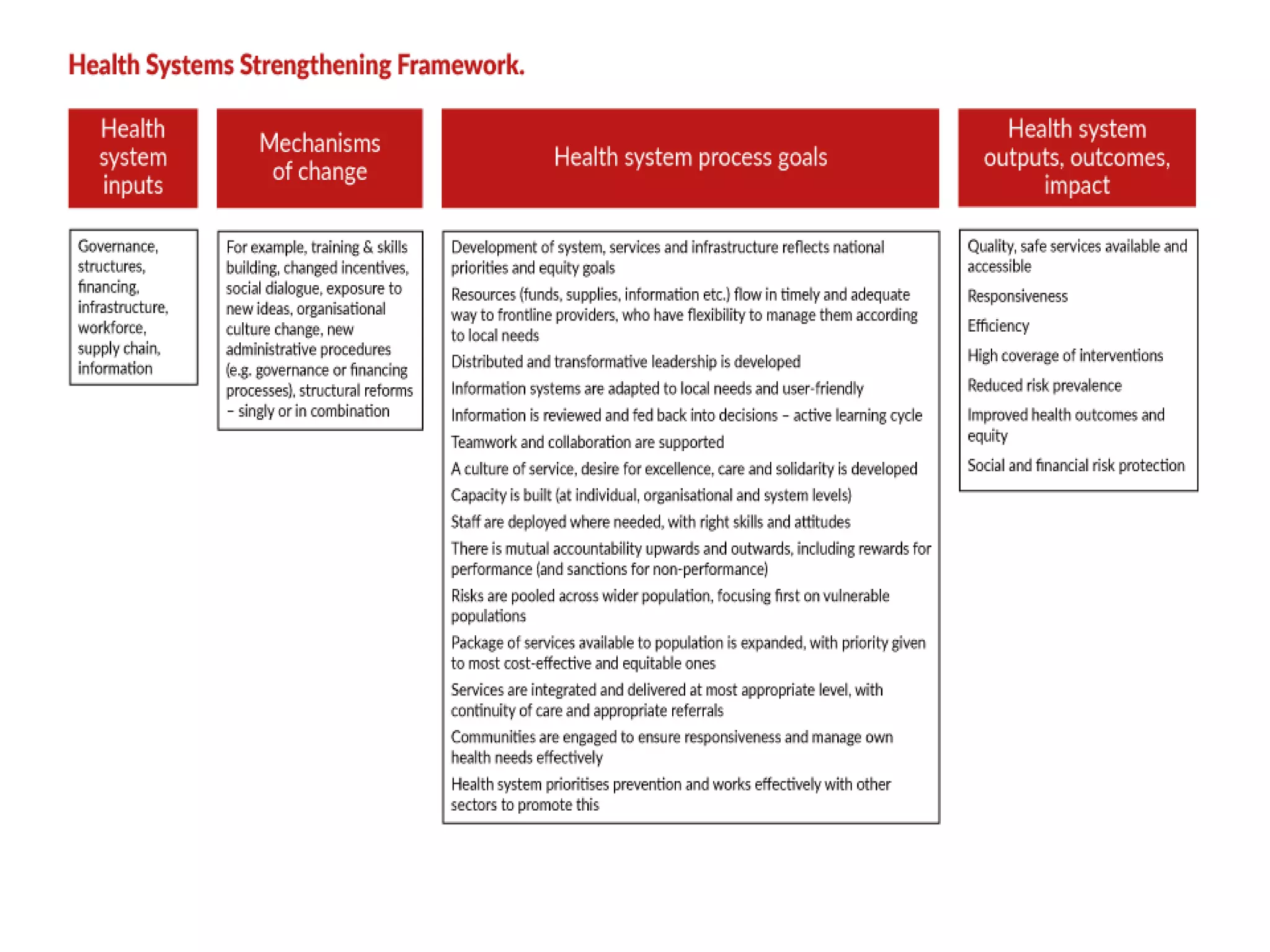
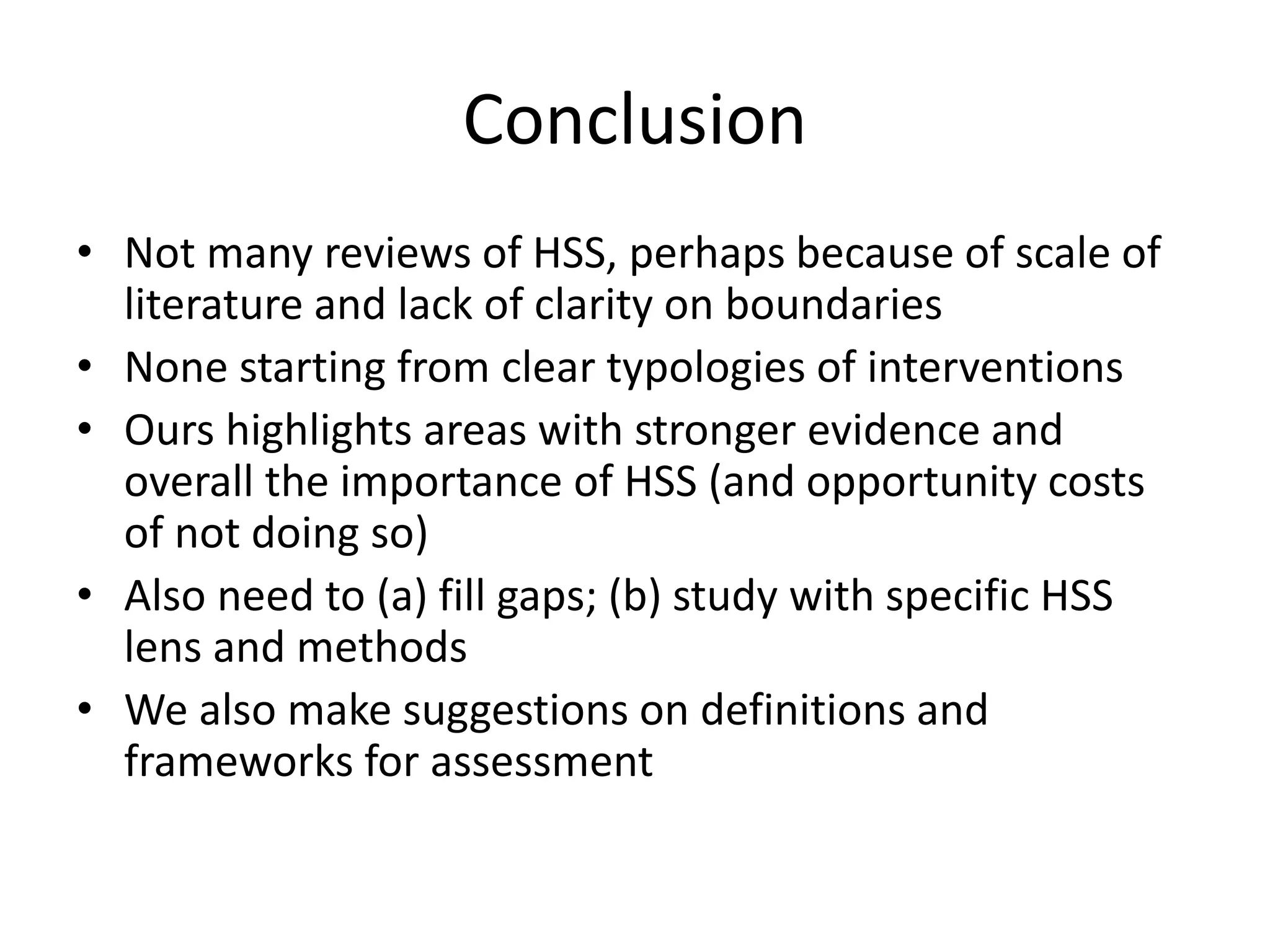
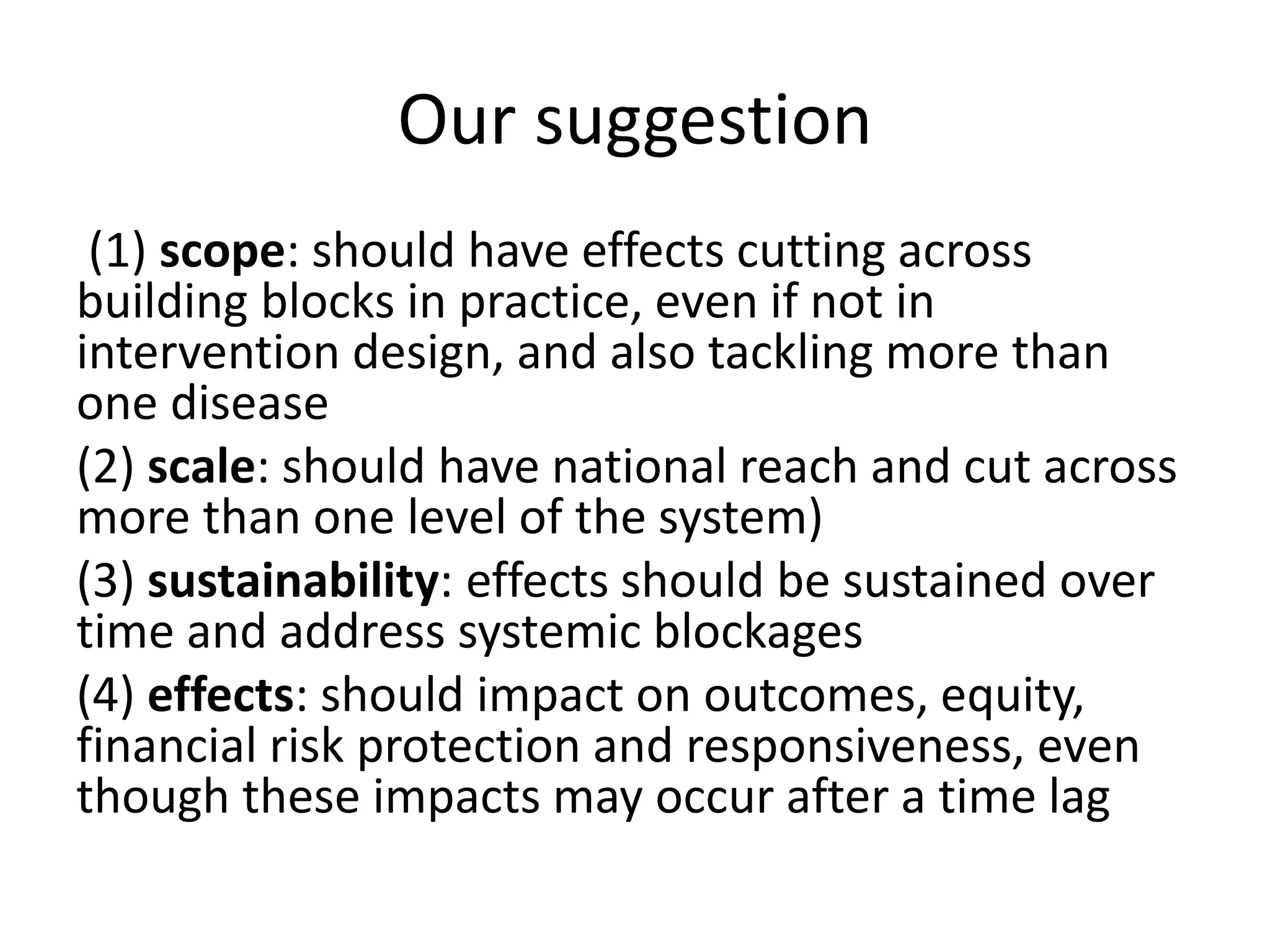
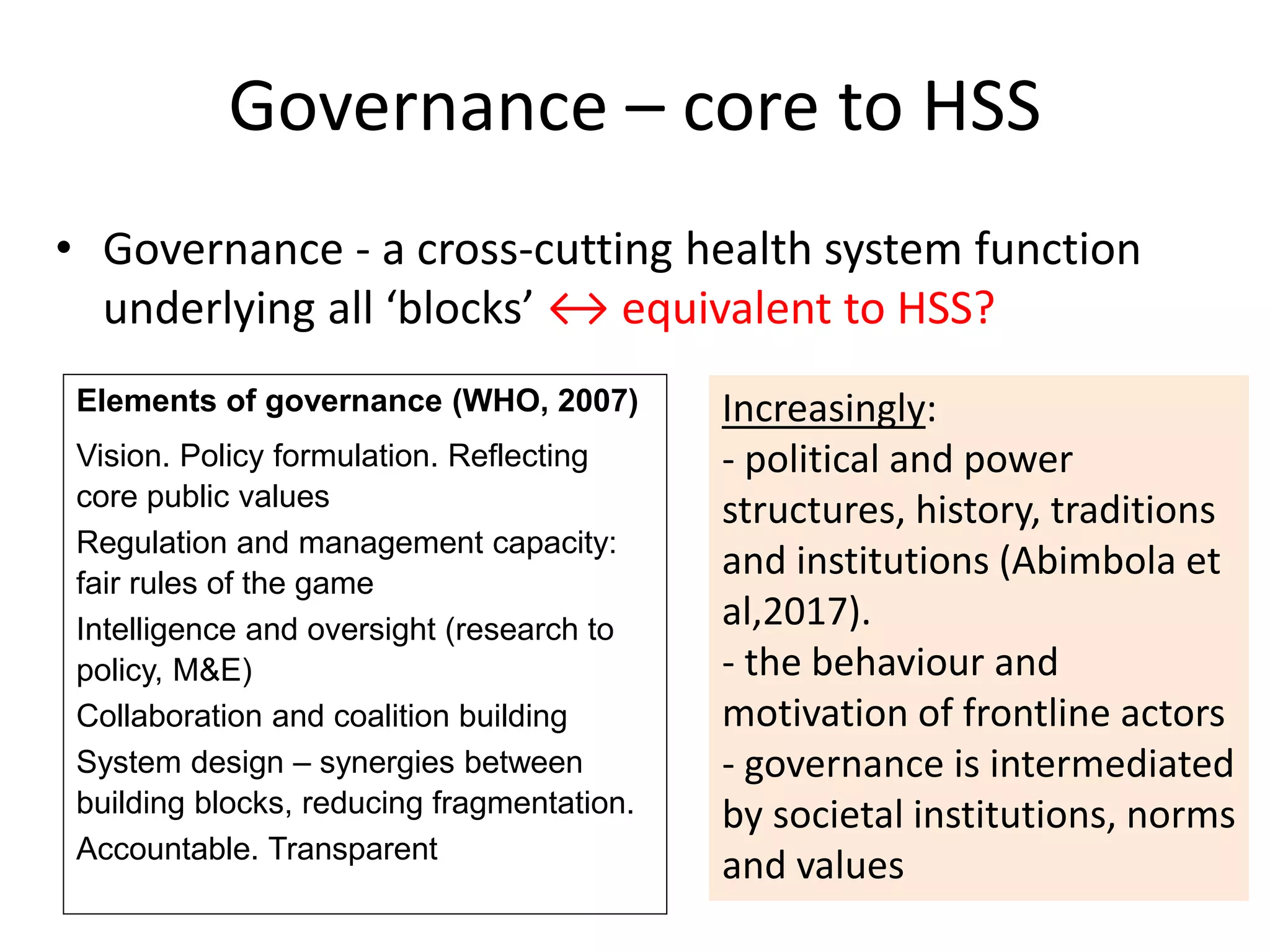
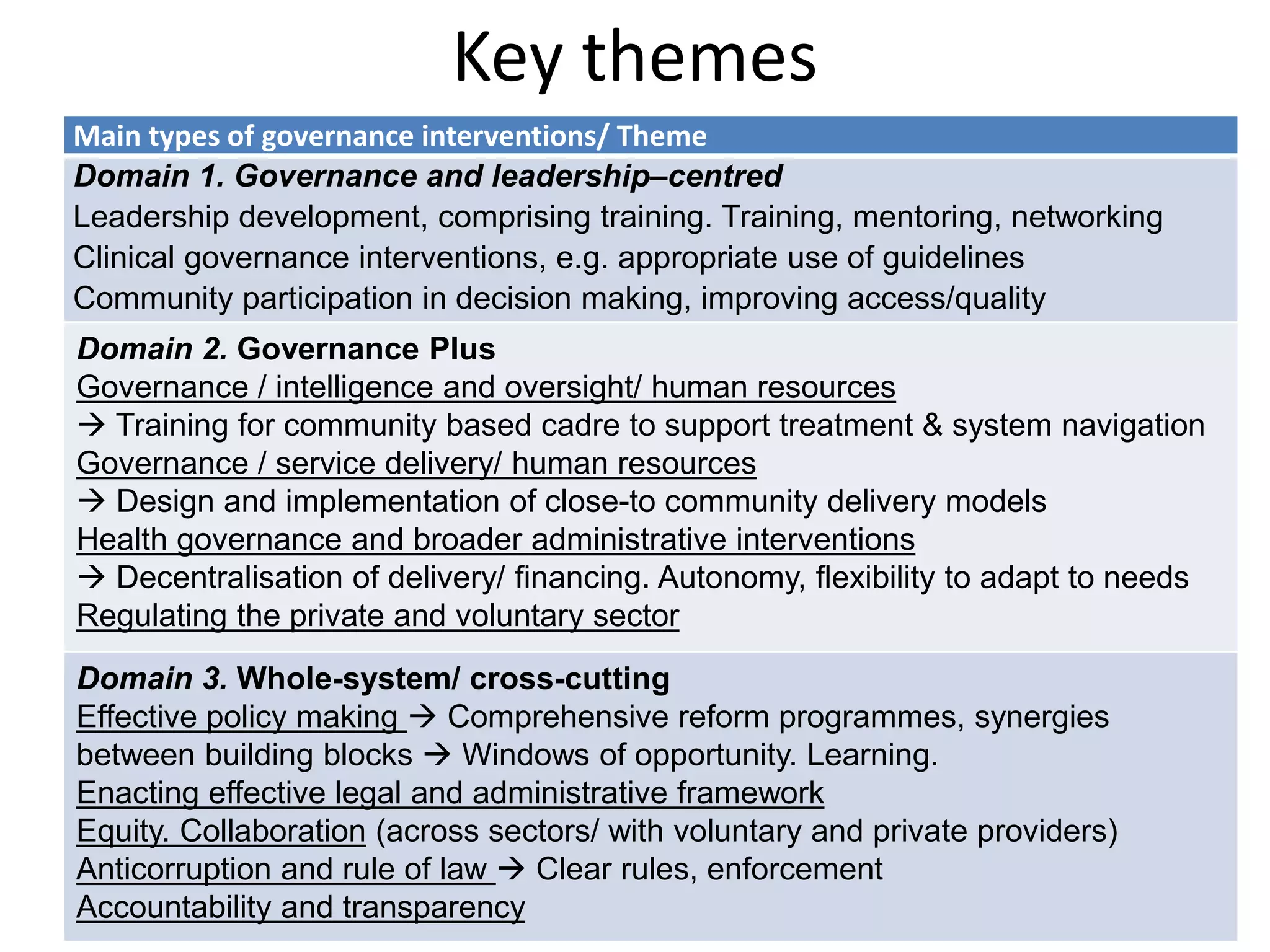
The document discusses health system strengthening (HSS), emphasizing its definition, assessment methods, and effectiveness in various contexts, particularly in low- and middle-income countries. It identifies challenges in evaluating HSS, outlines key governance and service delivery elements, and highlights the need for integrated approaches across multiple health system blocks to achieve sustainable improvements in health outcomes. The findings suggest that robust, context-sensitive evaluations and a deep understanding of the existing systems are crucial for HSS success.
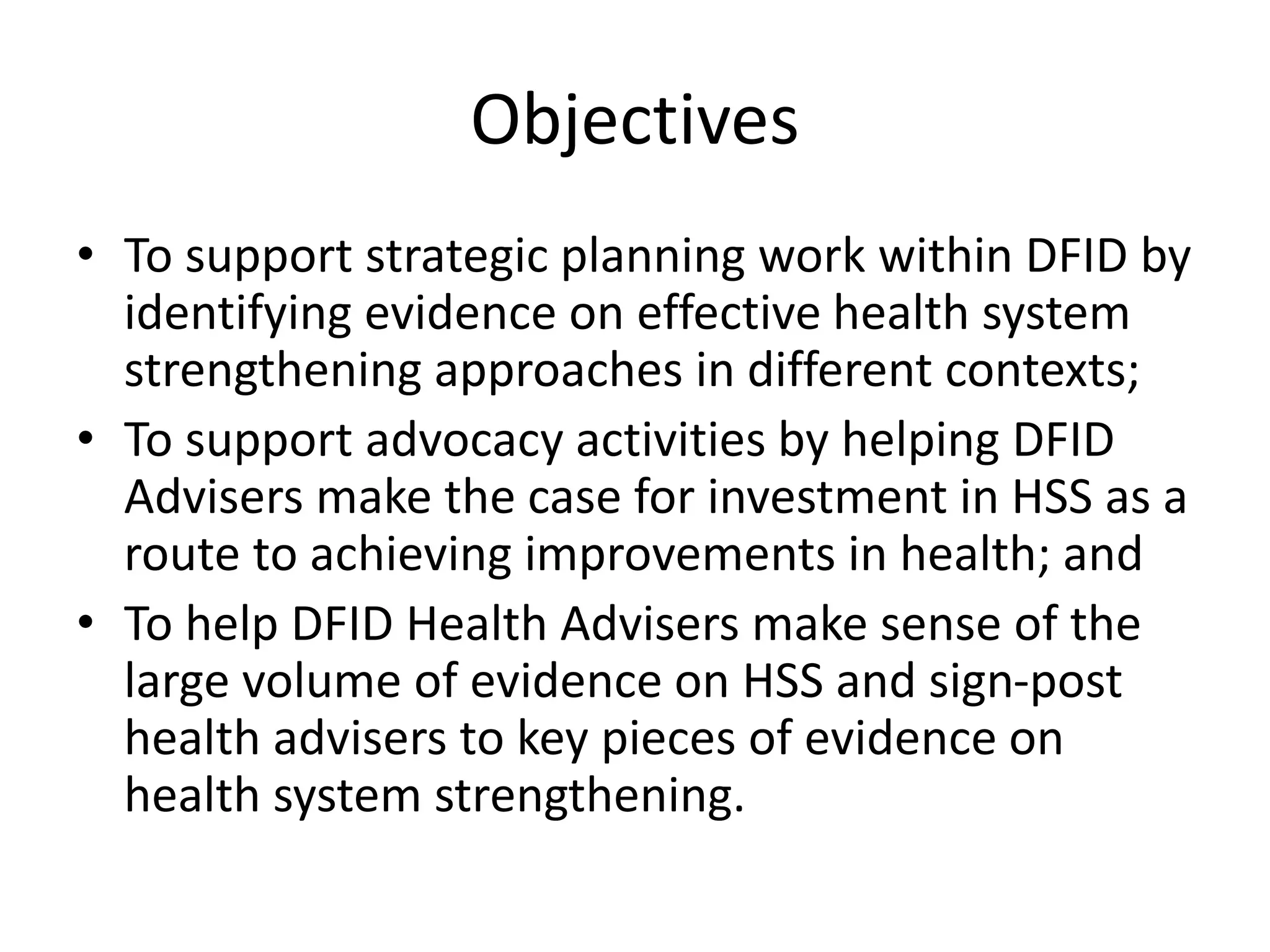
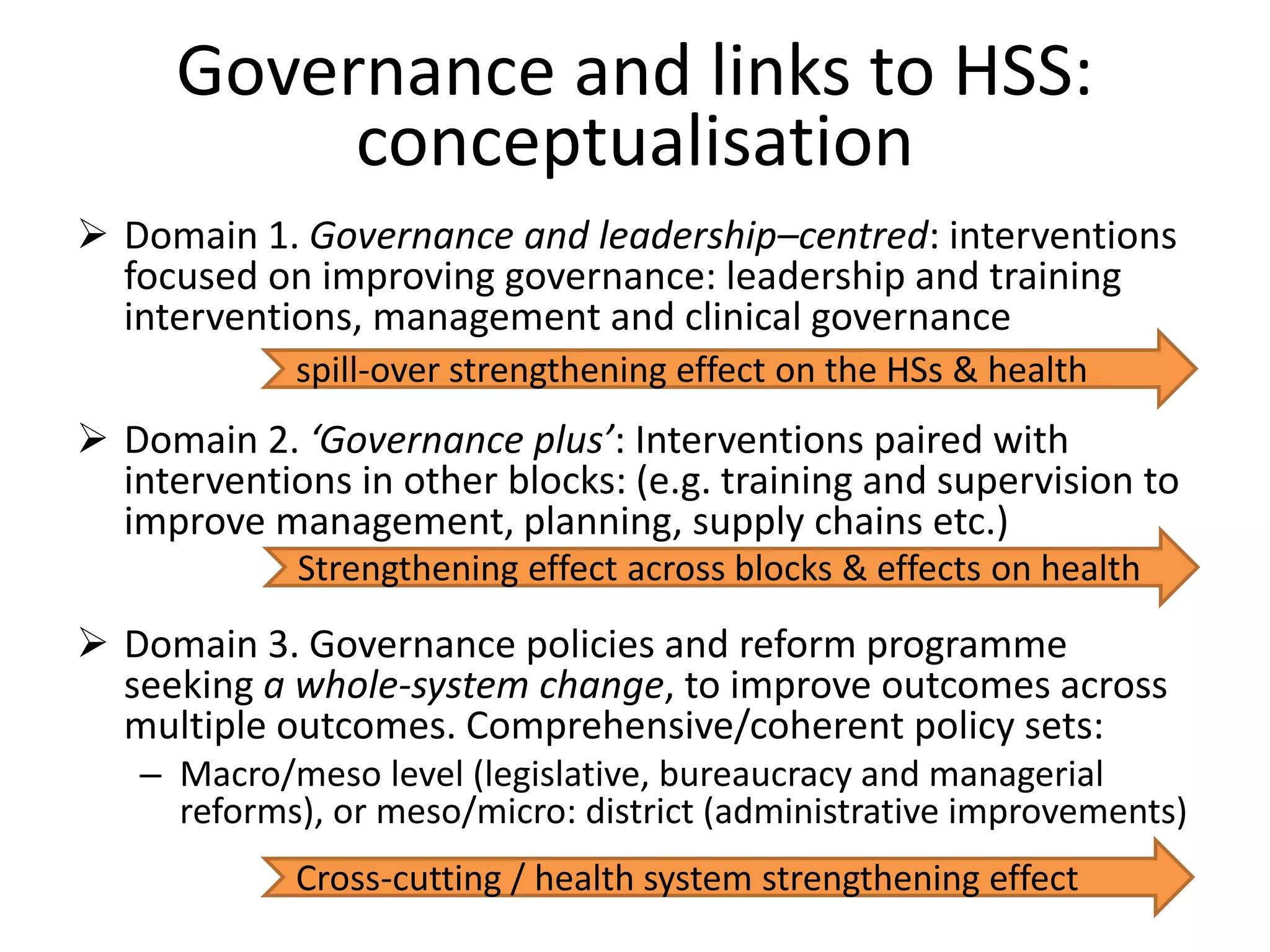
![Governance: selected findings
• Whole-system change: comprehensive HSS identify good
governance within complex, system-wide reform programmes
achieve impact across outcomes [7 studies, e.g. the Good Health at Low
Cost study)
– collaborative working, long-term strategic reforms across all levels of the
health system, using windows of opportunity
• Governance-focused interventions (civil participation and engaging
community members with health service structures) improve
health, uptake and quality of care (e.g. MCH)
• Leadership programmes blending skills development, mentoring
and teamwork improve service quality, management
competence and motivation [Bhoma, effect but sustained]
• Mixed evidence on decentralisation: can be promoting or
obstructing depending on the quality of management and
wider political processes](https://image.slidesharecdn.com/hssfordfid300719-190731093522/75/Health-system-strengthening-what-is-it-how-should-we-assess-it-and-does-it-work-12-2048.jpg)