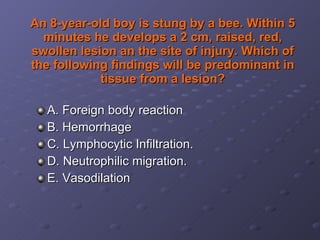
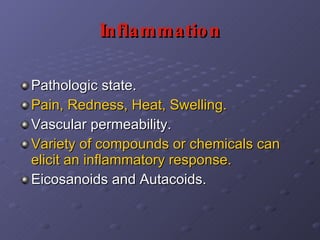
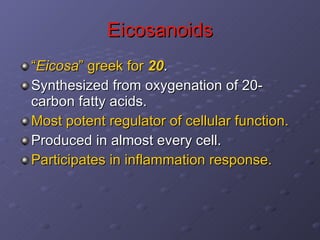
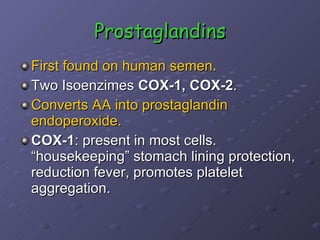
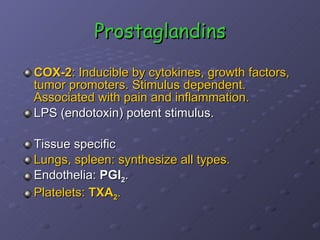
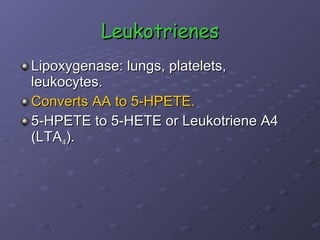
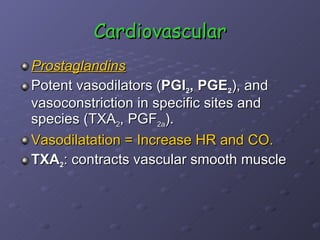
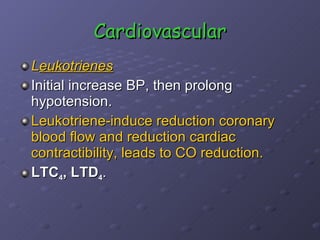
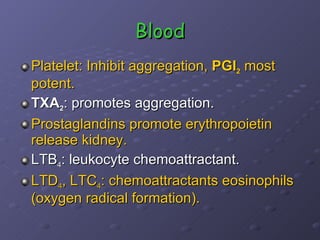
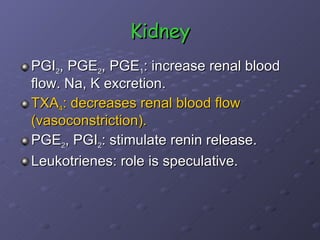
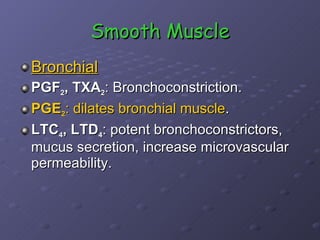
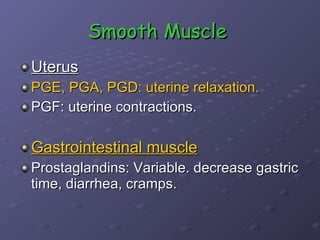
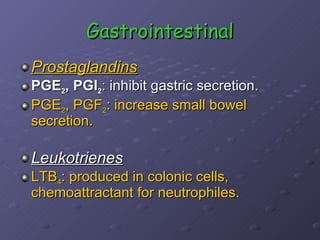
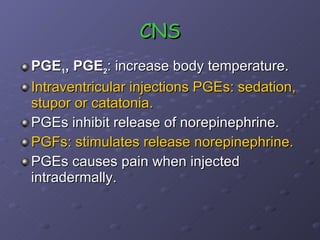
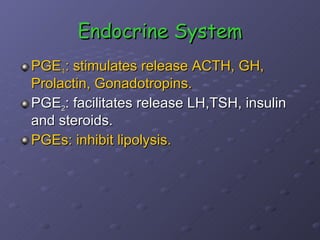
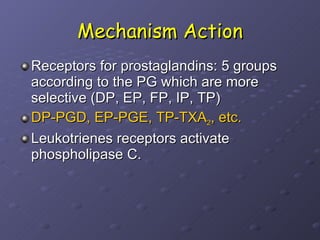
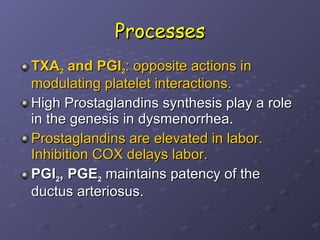
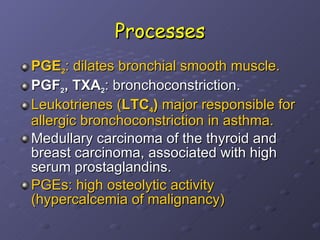
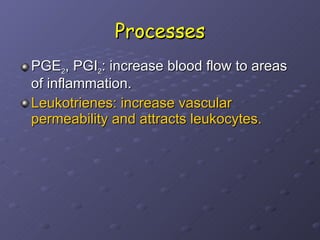
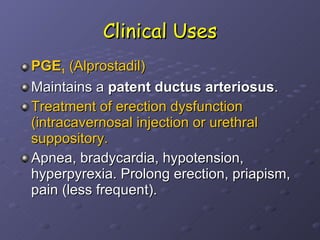
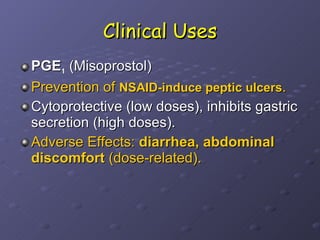
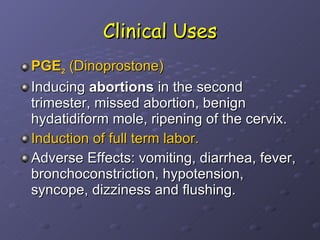
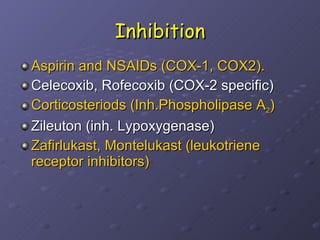
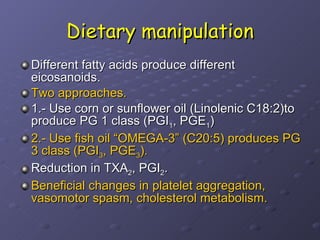
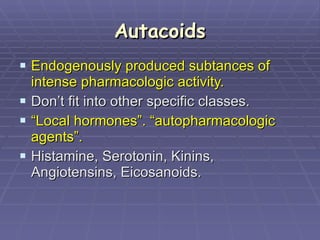
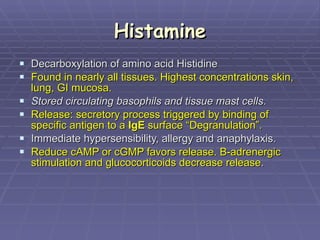
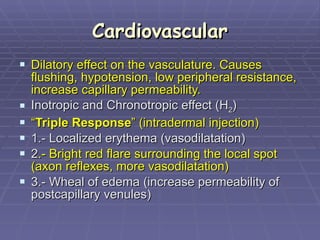
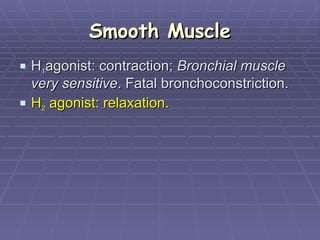
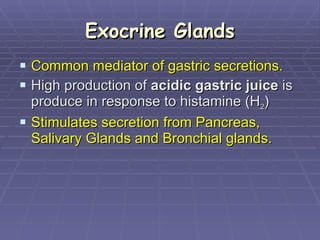
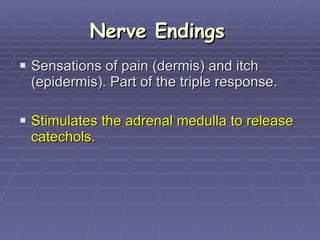
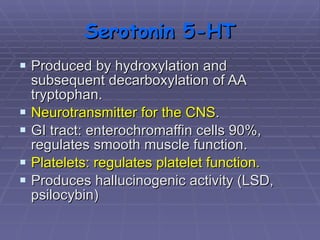
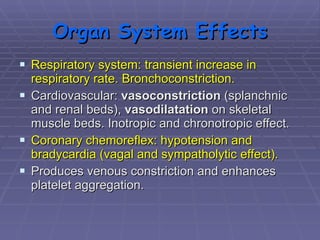
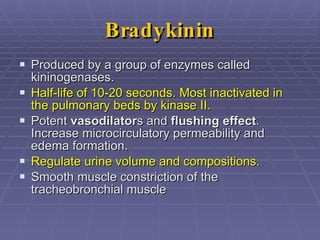
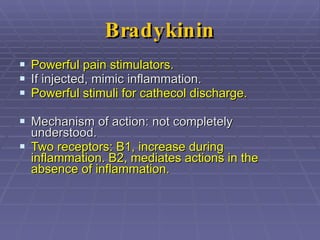
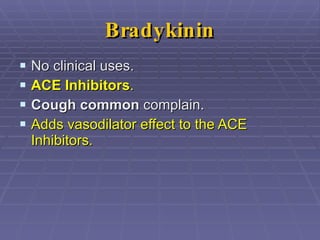
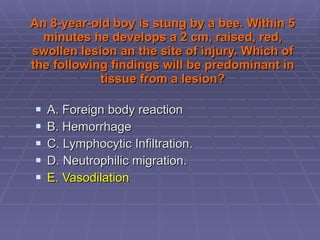
The document discusses autacoids and inflammation. It describes how within 5 minutes of being stung by a bee, a boy develops a swollen, red lesion at the site of injury. The predominant finding in tissue from the lesion would be neutrophilic migration (D). Autacoids like eicosanoids and histamine are involved in the inflammatory response and produce effects like vasodilation, pain, swelling and fever. Prostaglandins, thromboxanes and leukotrienes derived from arachidonic acid mediate inflammation.