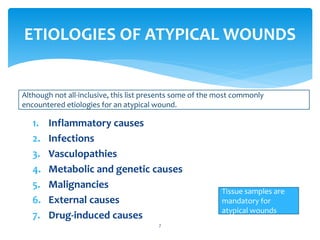
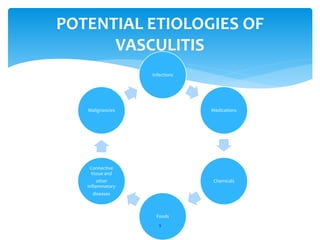
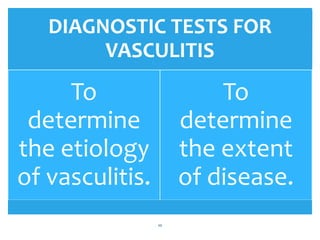
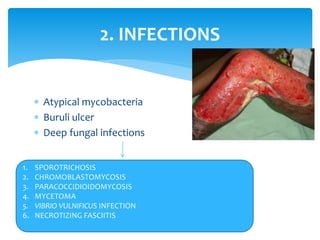
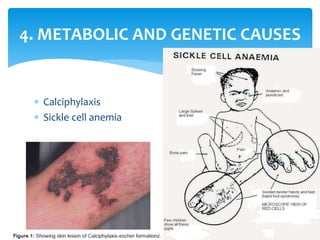
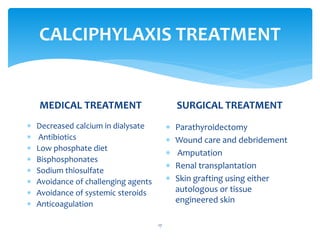
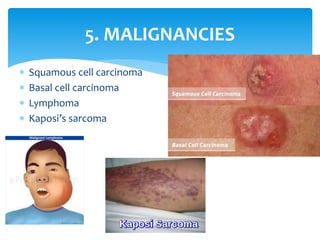
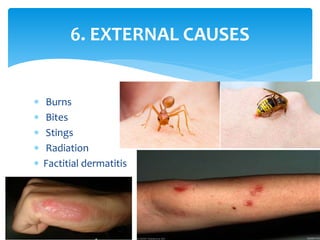
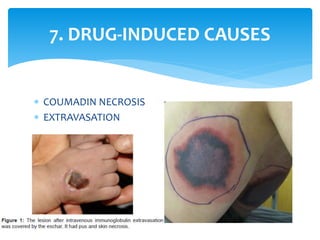
This document discusses atypical wounds, which are wounds with uncommon causes that do not respond to typical treatment. It defines atypical wounds and lists some main types, including pressure ulcers, venous leg ulcers, and diabetic foot ulcers. The document then discusses various etiologies of atypical wounds, such as infections, vasculopathies, inflammatory conditions, and malignancies. It provides examples of specific conditions for each category and considerations for treatment.