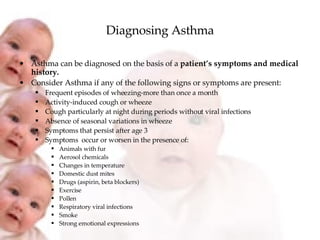
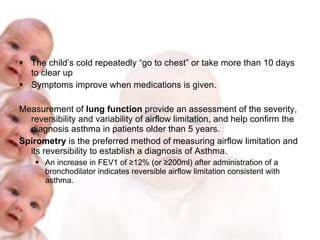
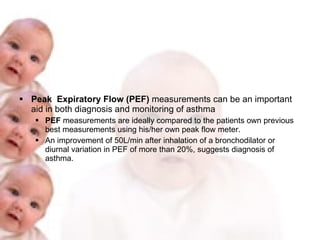
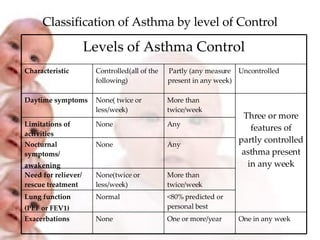
Asthma is a chronic inflammatory disorder of the airways that causes recurring episodes of wheezing, breathlessness, chest tightness and coughing. It affects people of all ages and its prevalence is increasing worldwide. Asthma can be diagnosed based on symptoms and medical history and confirmed through lung function tests. Effective asthma management requires a partnership between the patient and doctor to control symptoms, identify and reduce risk factors, treat exacerbations, and monitor the condition.