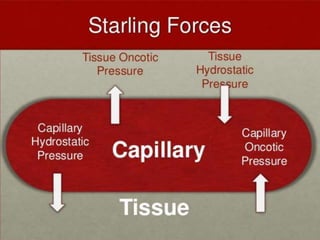
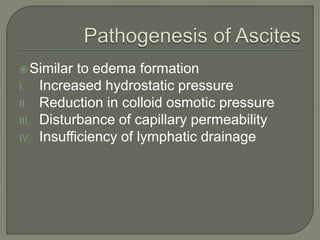
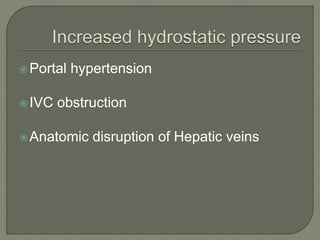
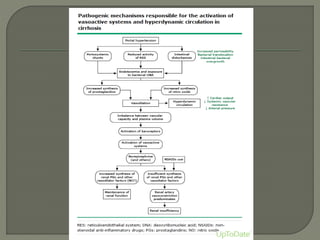
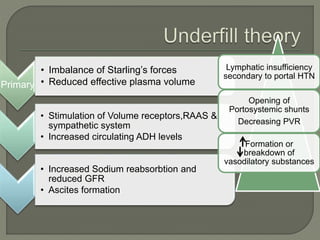
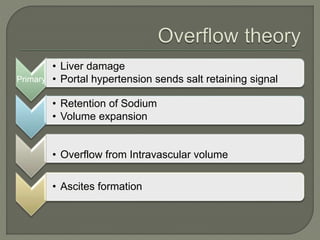
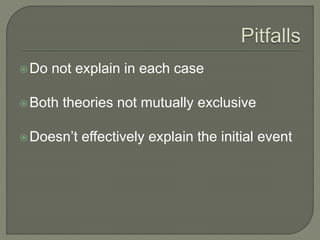
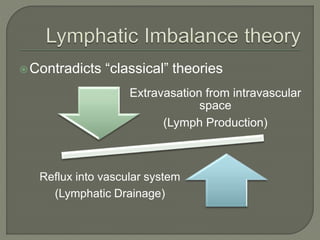
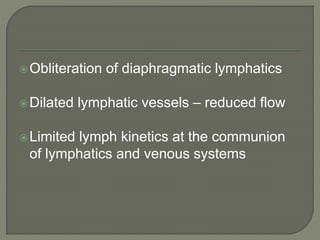
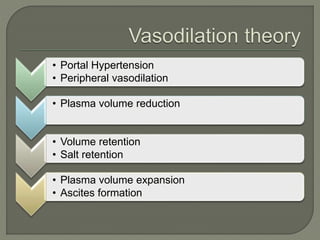
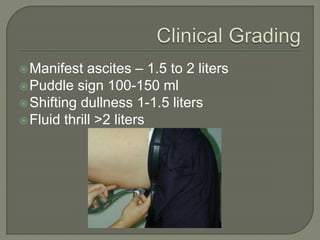
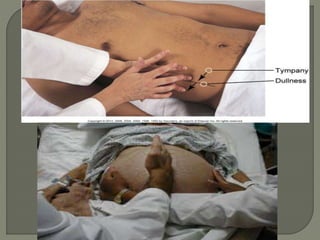
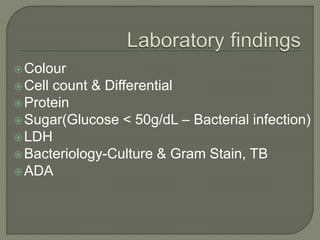
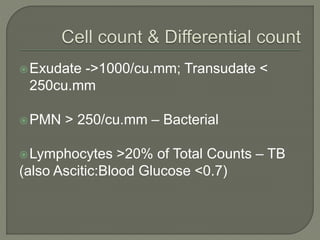
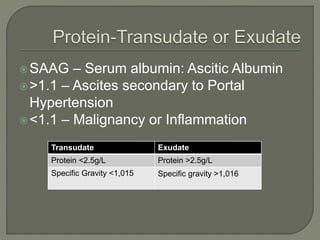
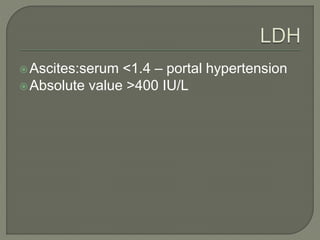
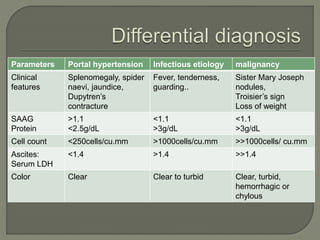
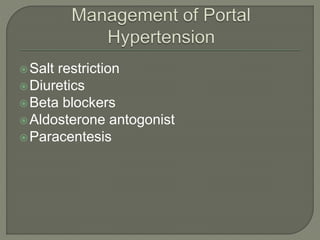
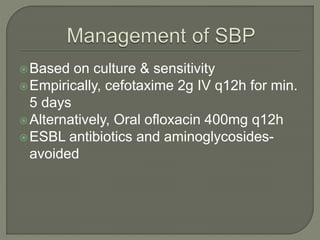
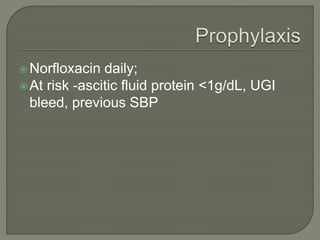
This document discusses ascites, which is an accumulation of fluid in the peritoneal cavity. It was first coined by Aulus Cornelius Celsus, a Roman physician from 25 BC to 50 AD. The document covers the definition, pathogenesis, theories of ascites formation, differential diagnosis, management, and laboratory findings of ascites. It discusses how ascites can be caused by portal hypertension, liver damage, infection, or malignancy. Diagnosis involves analyzing ascitic fluid for characteristics like SAAG, cell count, protein level, and LDH to determine the underlying etiology. Management depends on the cause and may include salt restriction, diuretics, beta blockers, paracentesis, or antibiotics.