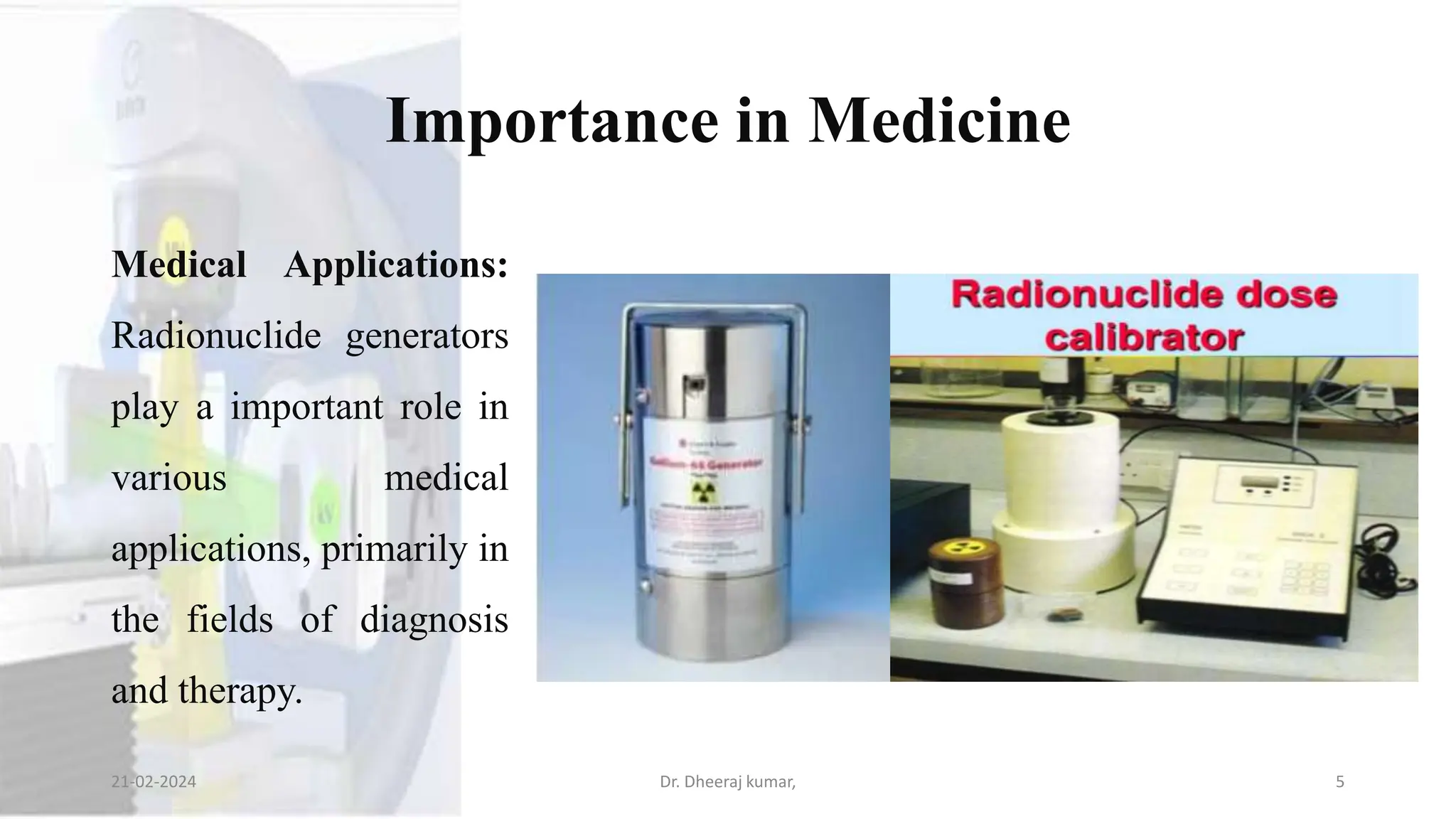
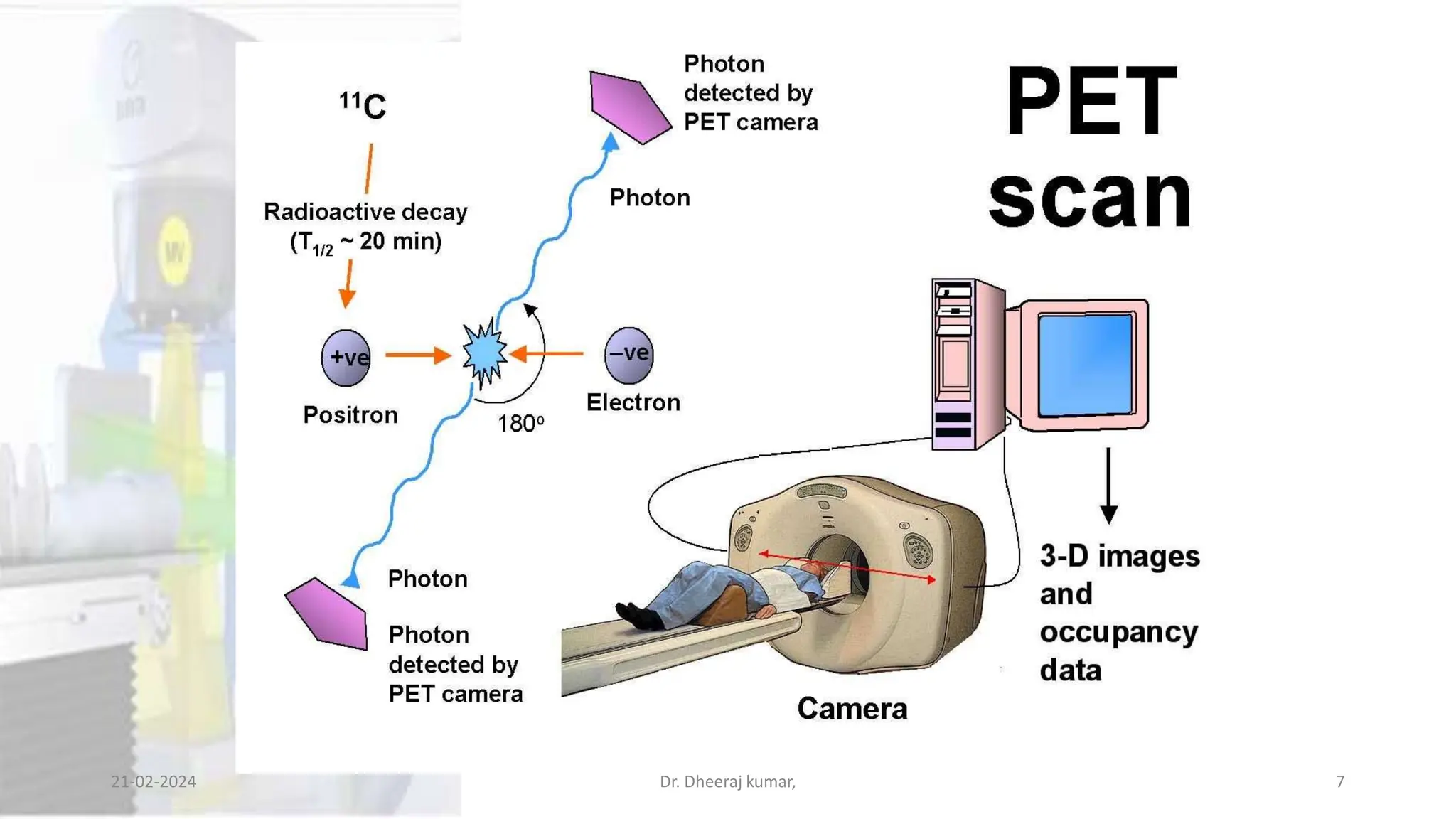
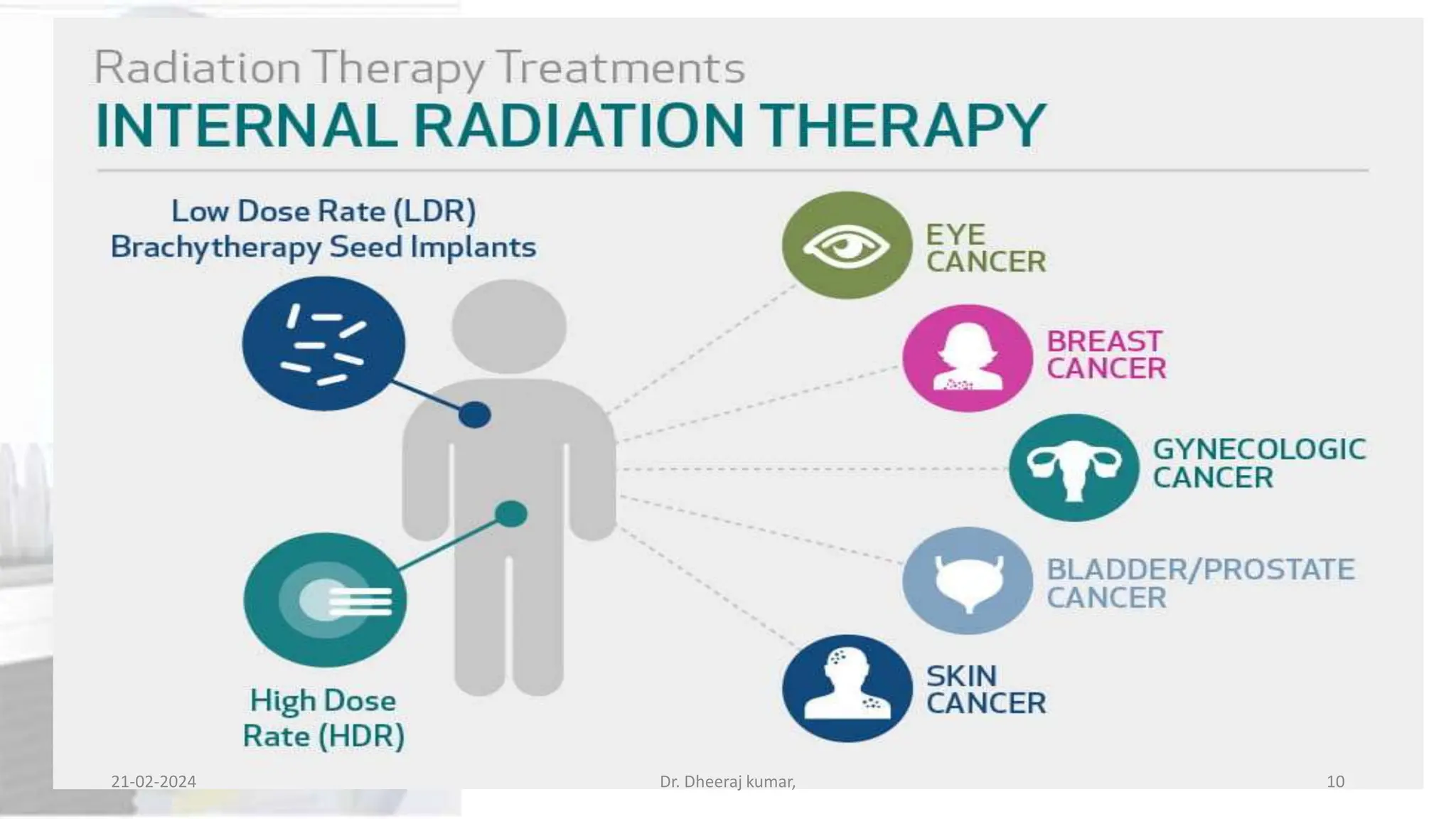
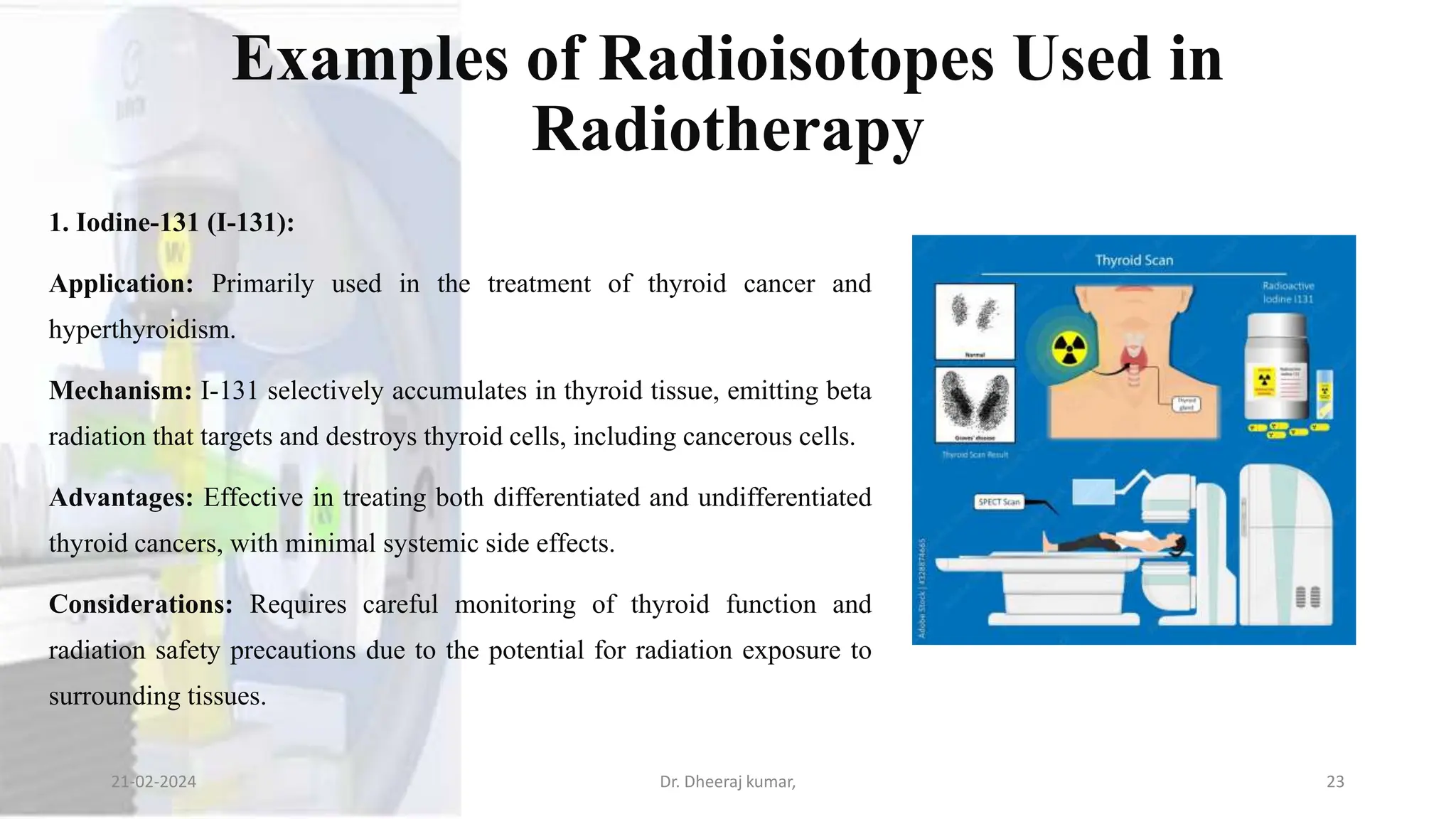
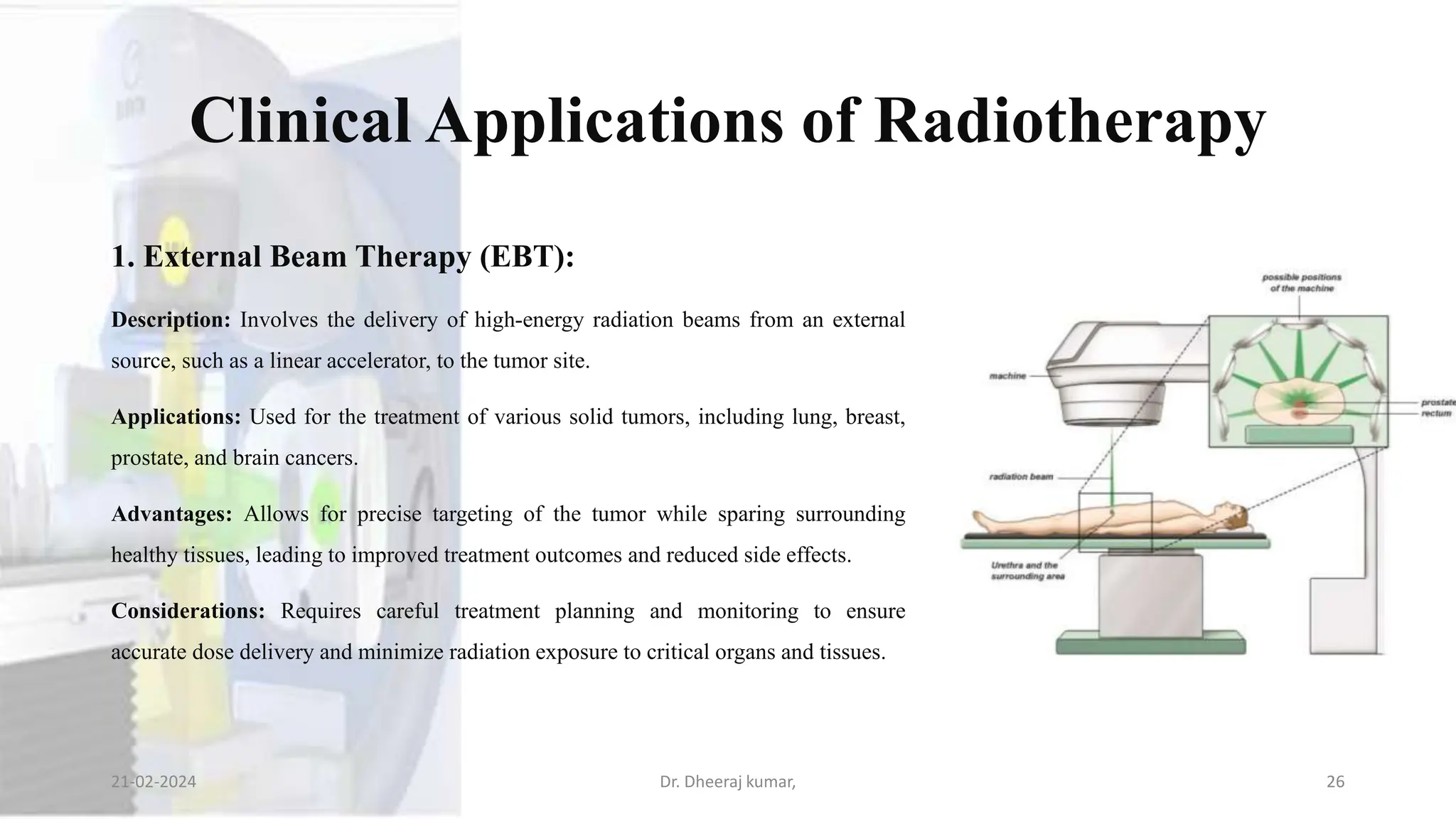
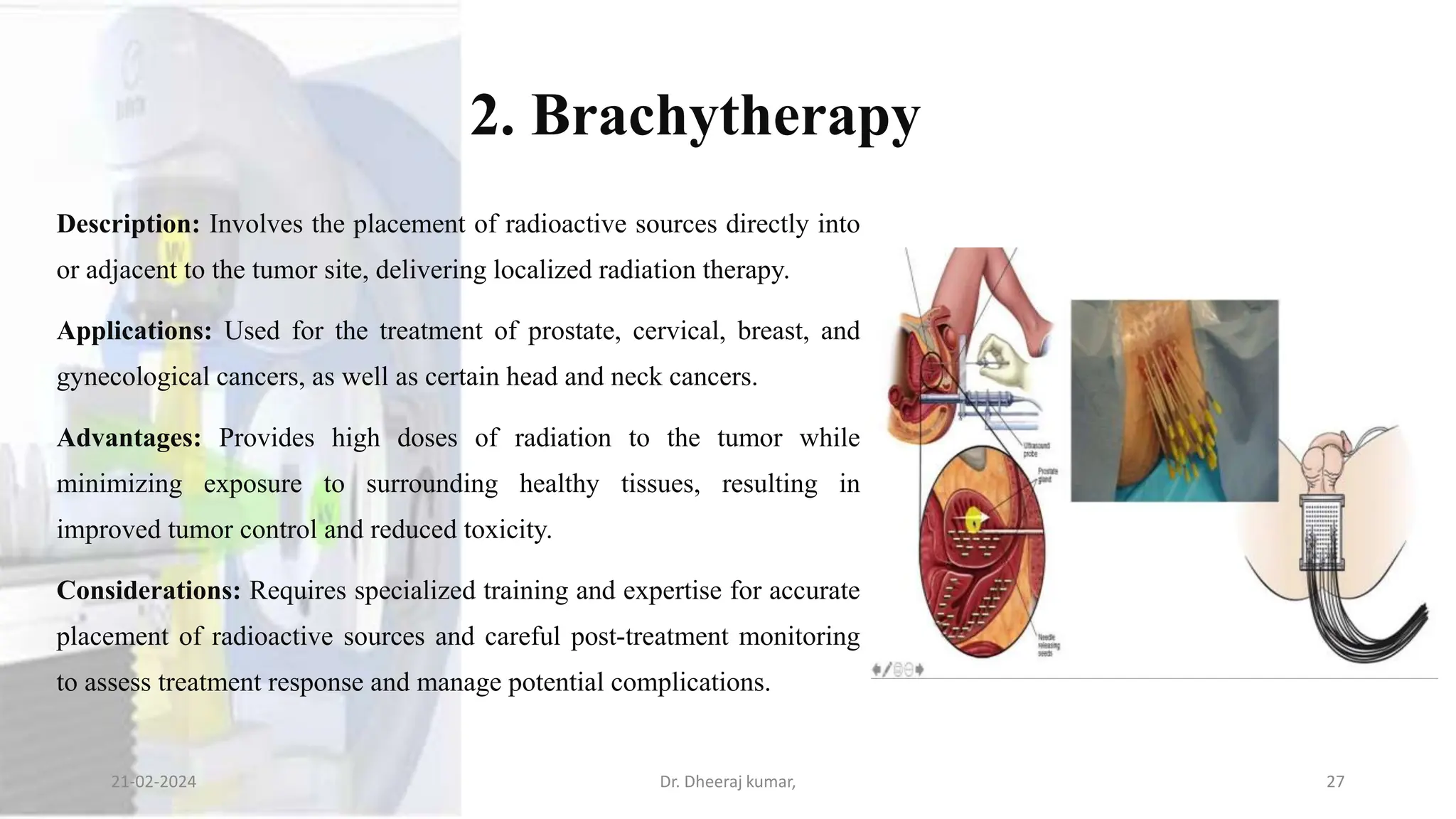
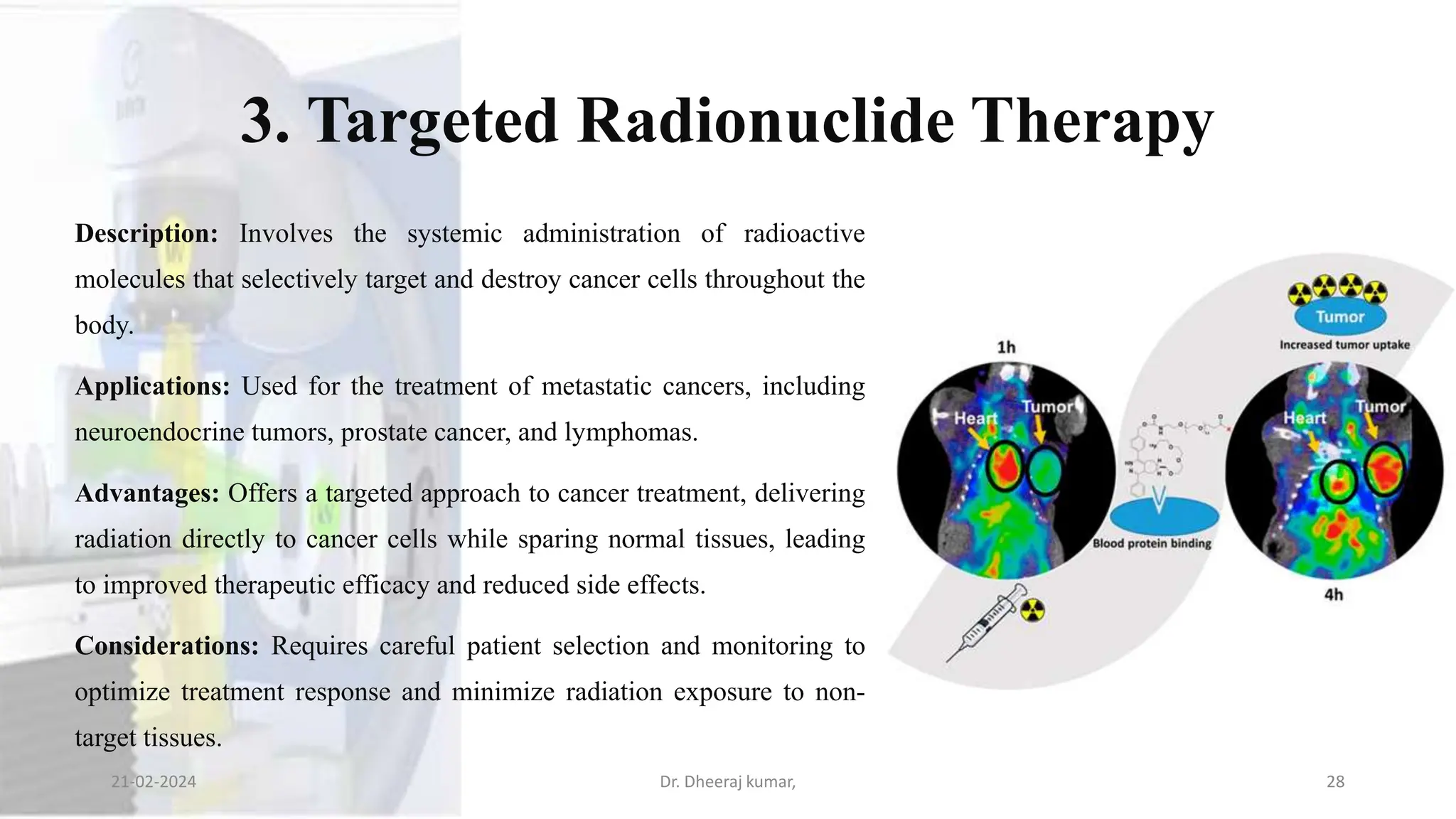
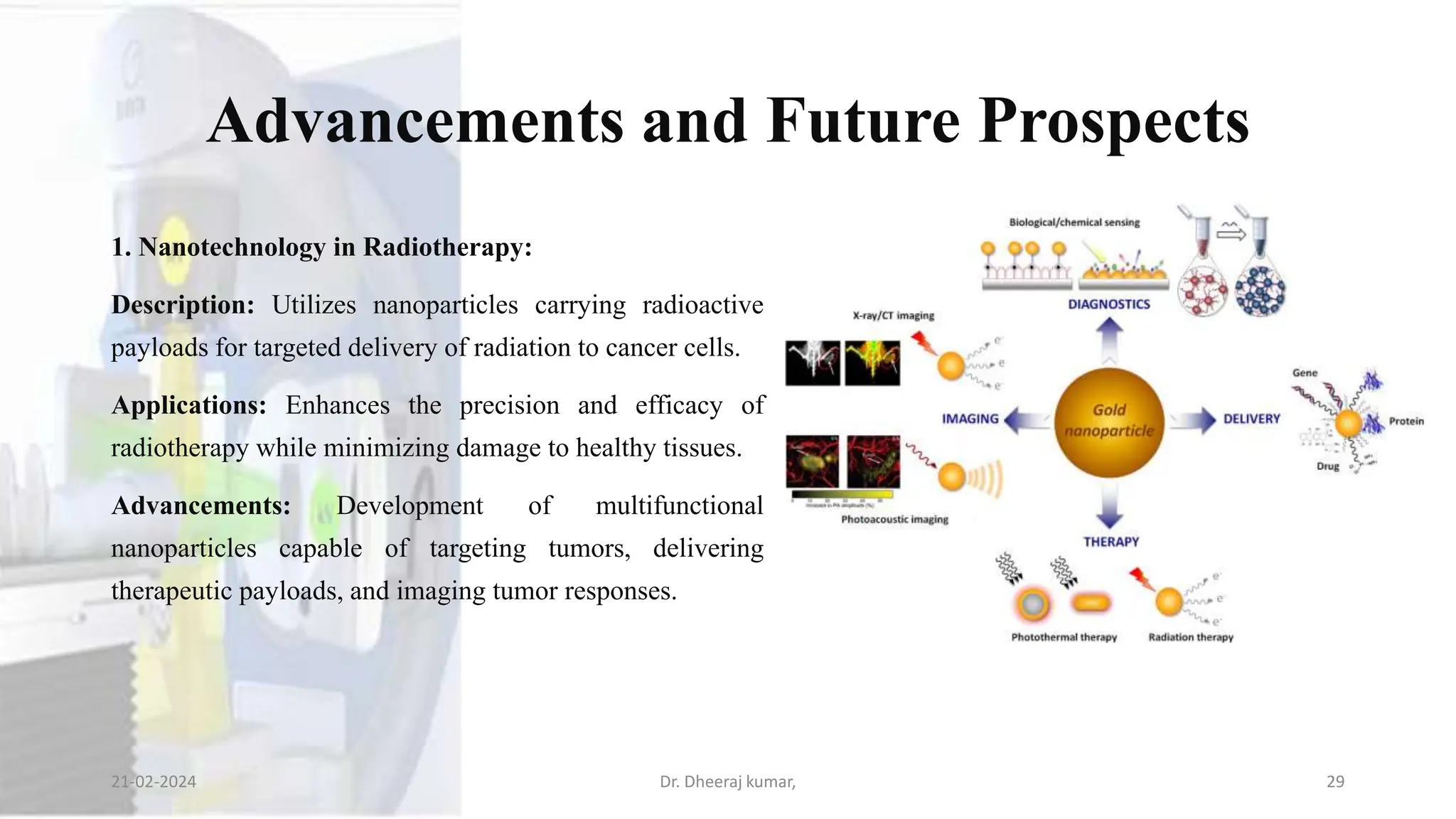
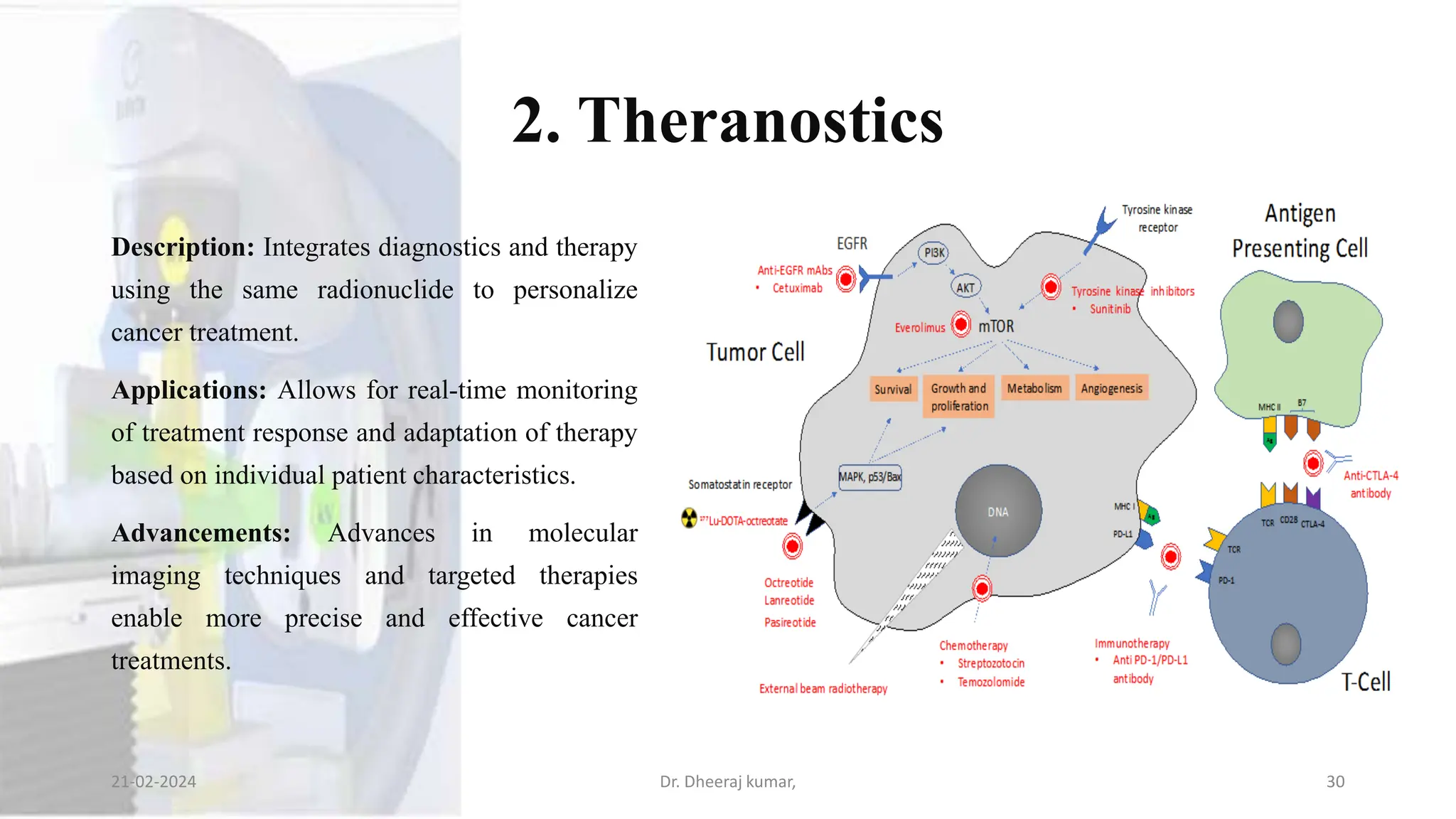
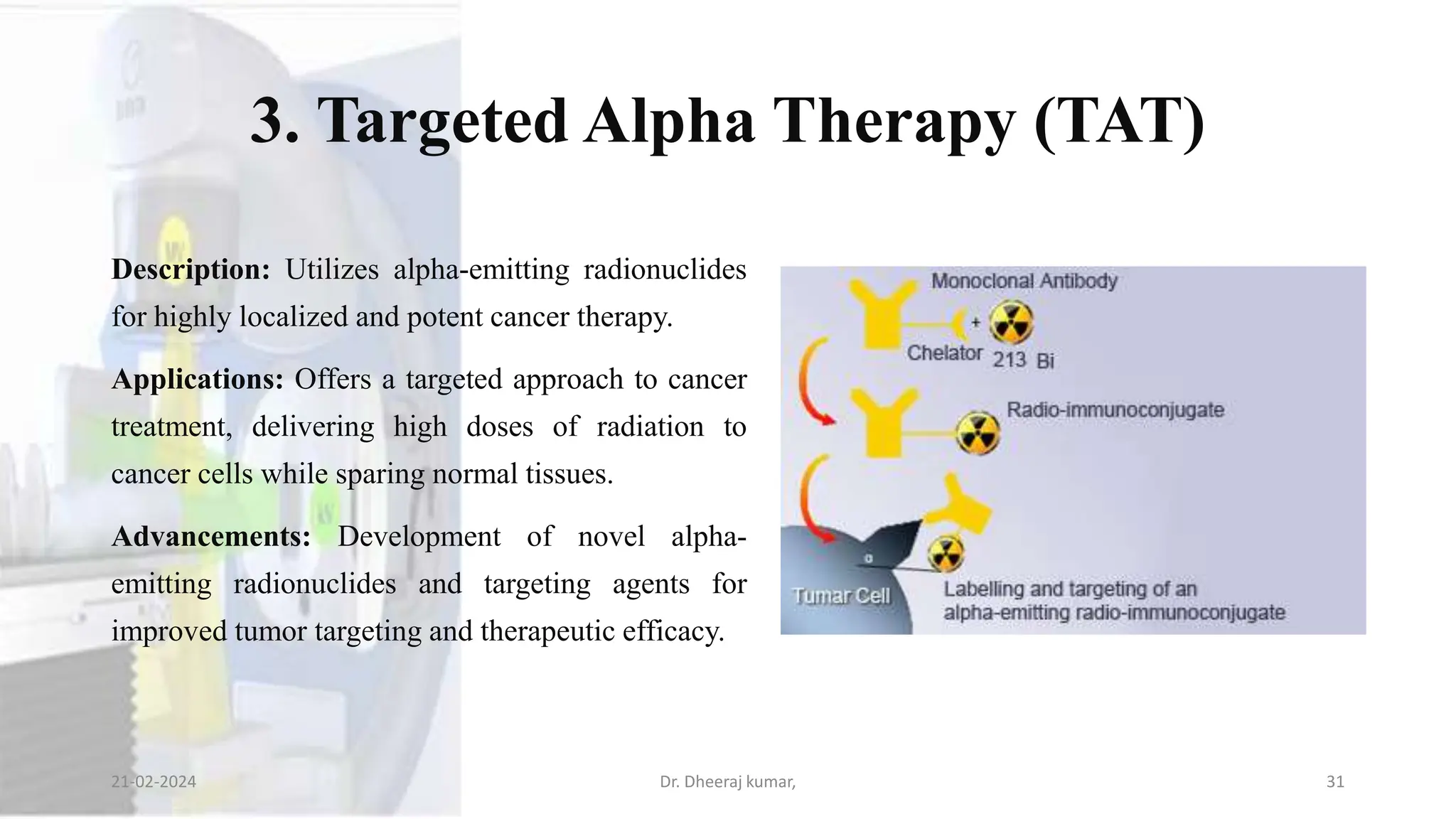
The document discusses artificial radionuclide generators used in medicine, focusing on their roles in diagnostics and therapy, especially in radiotherapy. It explains the mechanism of radionuclide generators, highlighting their importance in providing specific radioisotopes for medical applications and detailing various types of generators. Additionally, the document covers the advantages of radionuclide generators in targeted cancer treatments, safety protocols, and future advancements in radiotherapy.