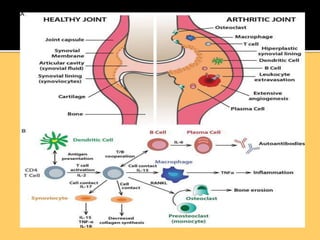
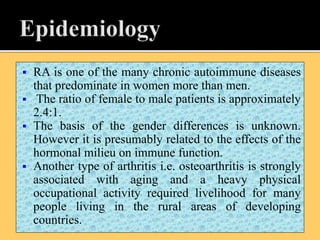
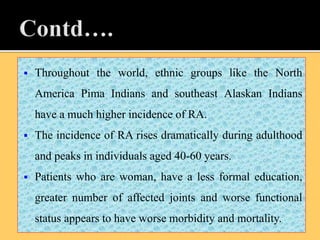
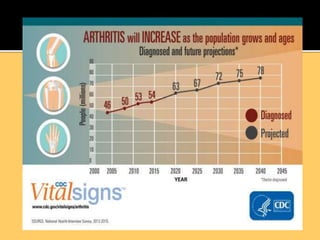
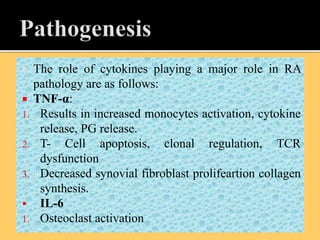
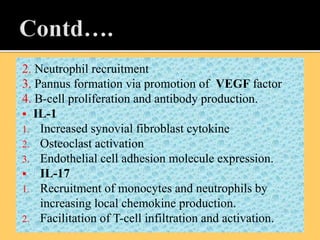
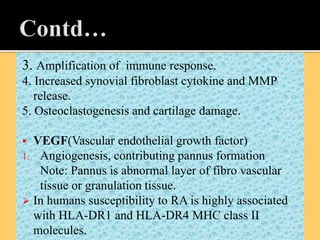
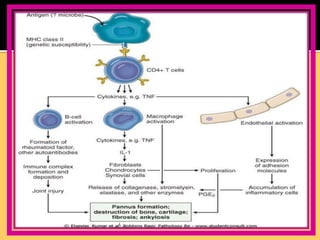
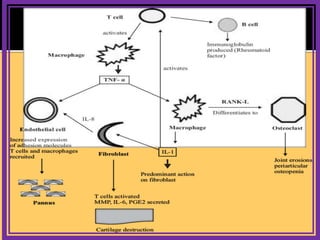
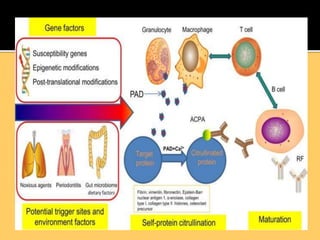
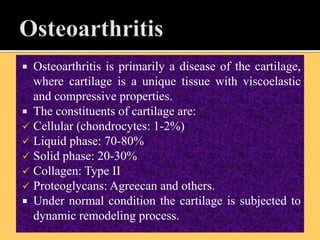
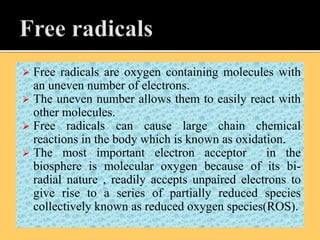
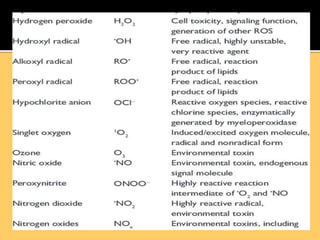
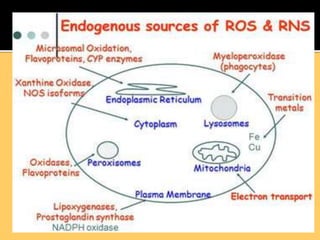
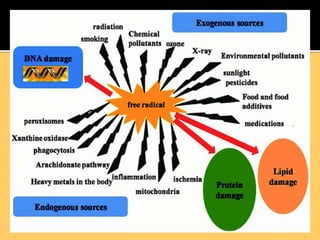
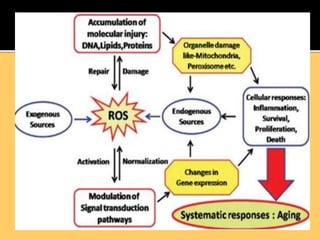
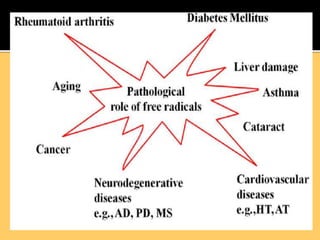
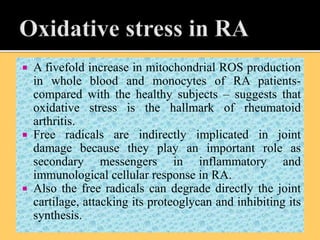
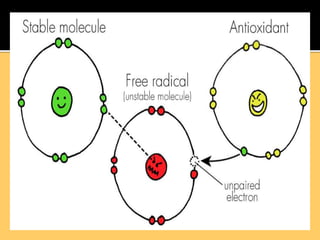
The document discusses the significance of herbal medicine in global healthcare, highlighting that around 80% of the African population uses traditional herbal remedies, which are linked to a market nearing US $60 billion. It also elaborates on various types of arthritis, including rheumatoid arthritis and osteoarthritis, emphasizing their causes, symptoms, and treatment options. Moreover, the document outlines the role of free radicals and oxidative stress in the pathology of rheumatoid arthritis, as well as the prevalence of arthritis in the US population.