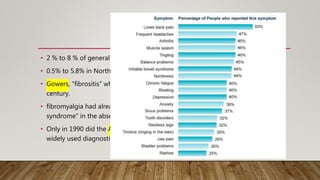
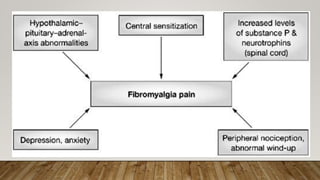
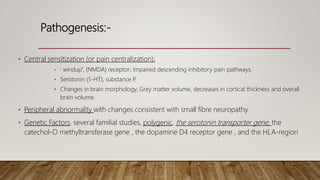
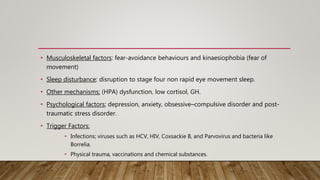
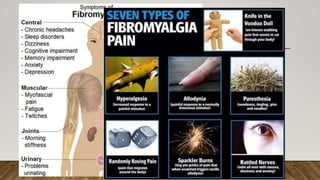
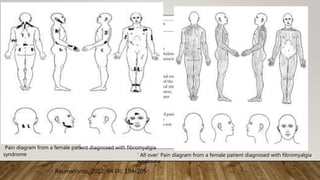
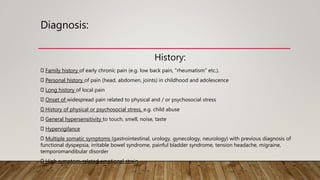
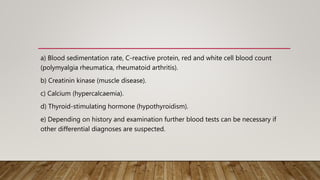
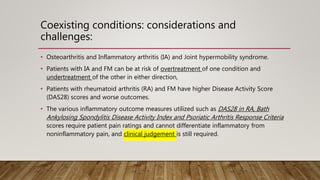
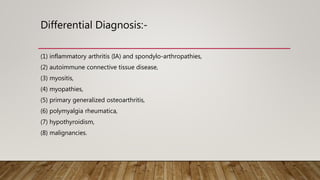
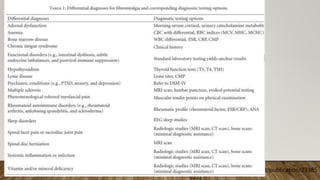
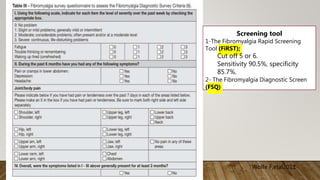
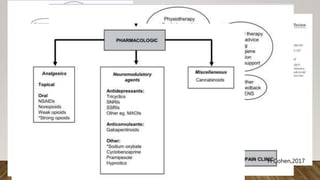
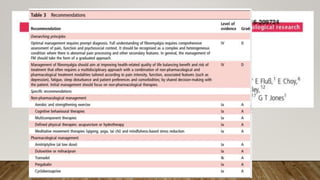
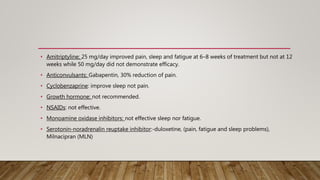
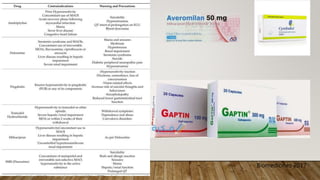
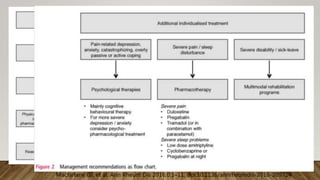
This document summarizes information about fibromyalgia syndrome (FMS), including its classification, symptoms, pathogenesis, diagnosis, and treatment. FMS is characterized by widespread pain, joint stiffness, and other symptoms like fatigue, sleep issues, and mood disorders. It affects 2-8% of the population. The cause is unclear but may involve central and peripheral nervous system sensitization. Diagnosis involves evaluating symptoms and tender points while ruling out other conditions. Treatments aim to reduce pain and improve sleep, mood, and function, and may include medications like duloxetine, milnacipran, and gabapentin.