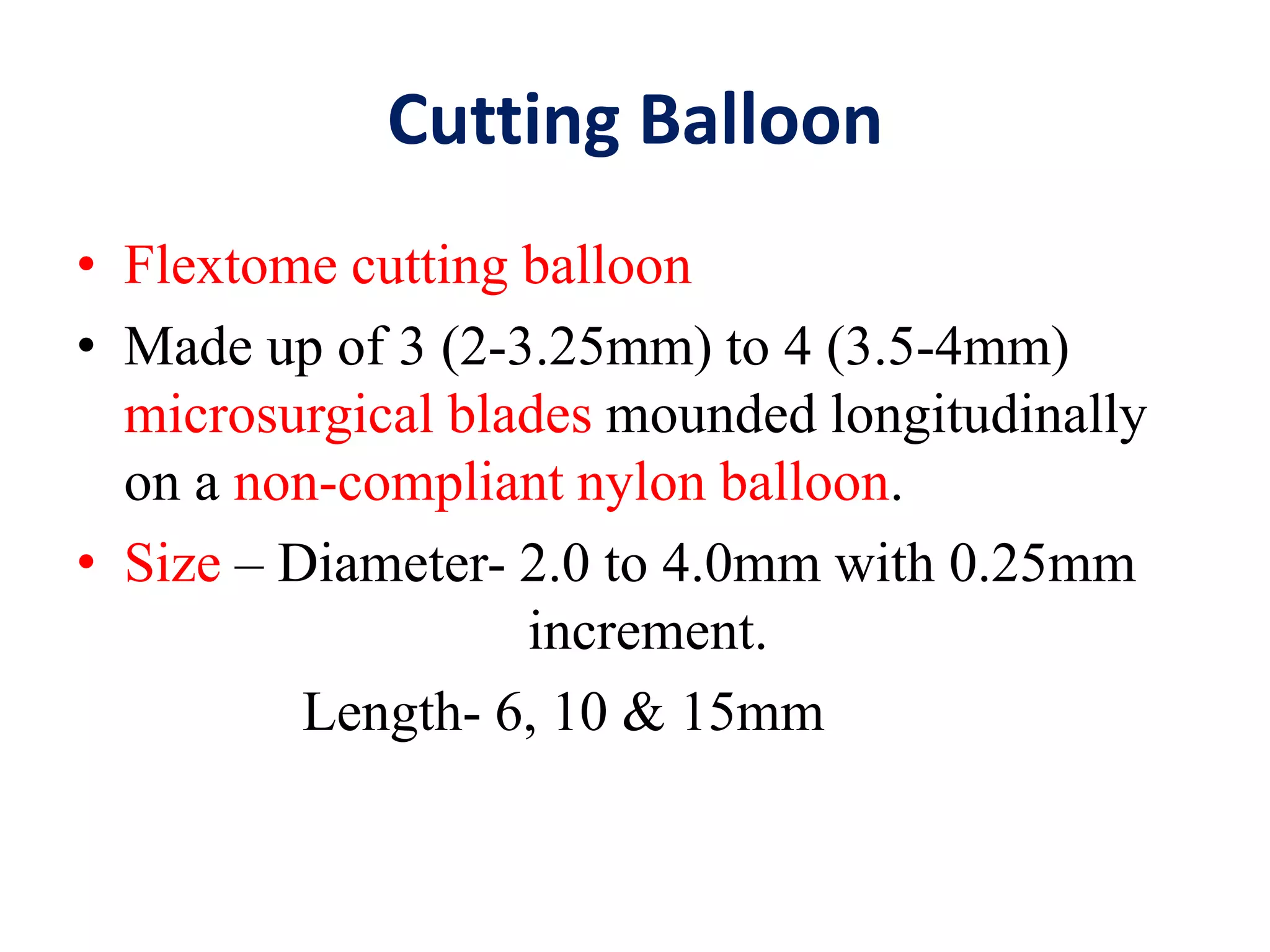
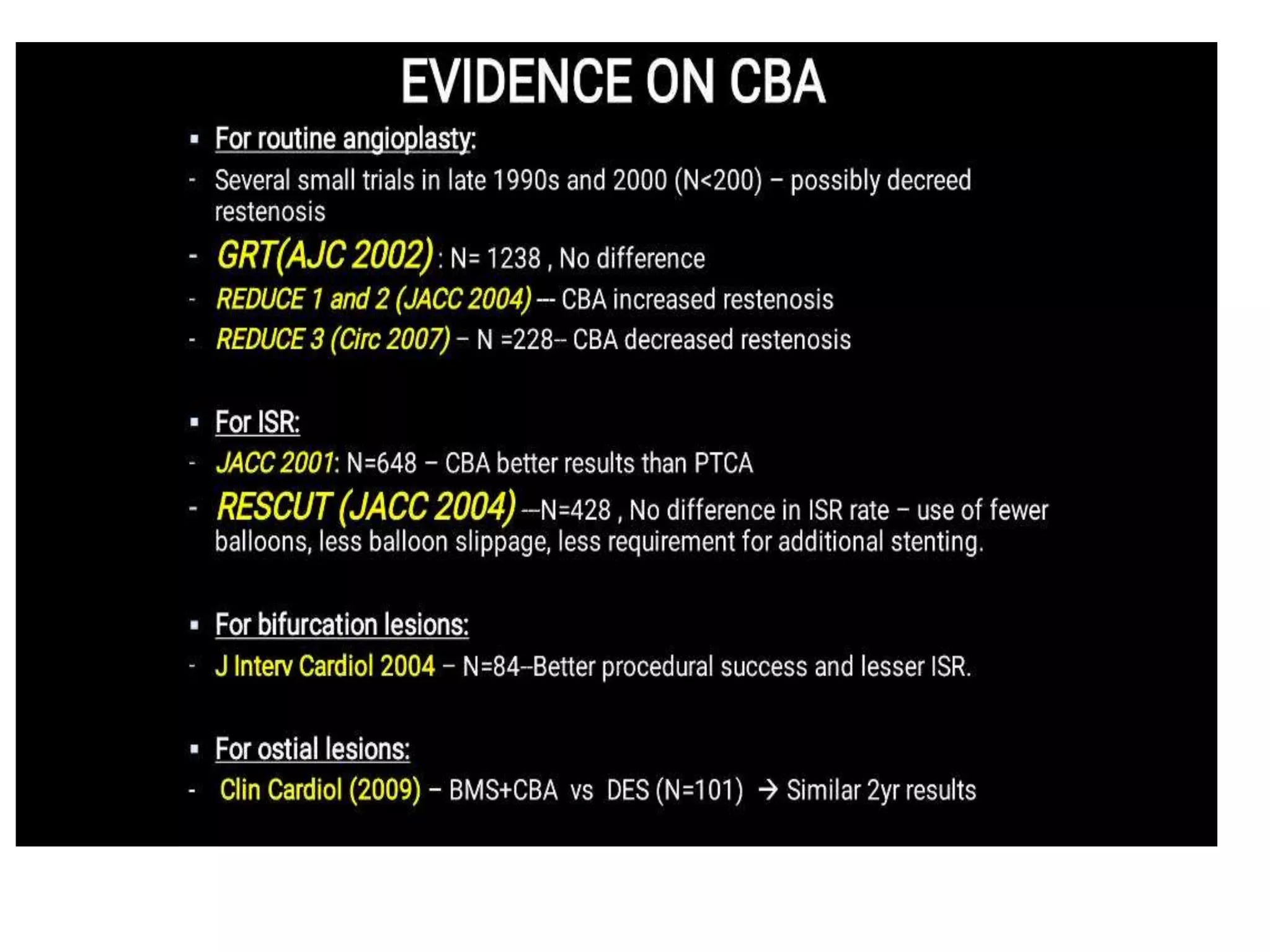
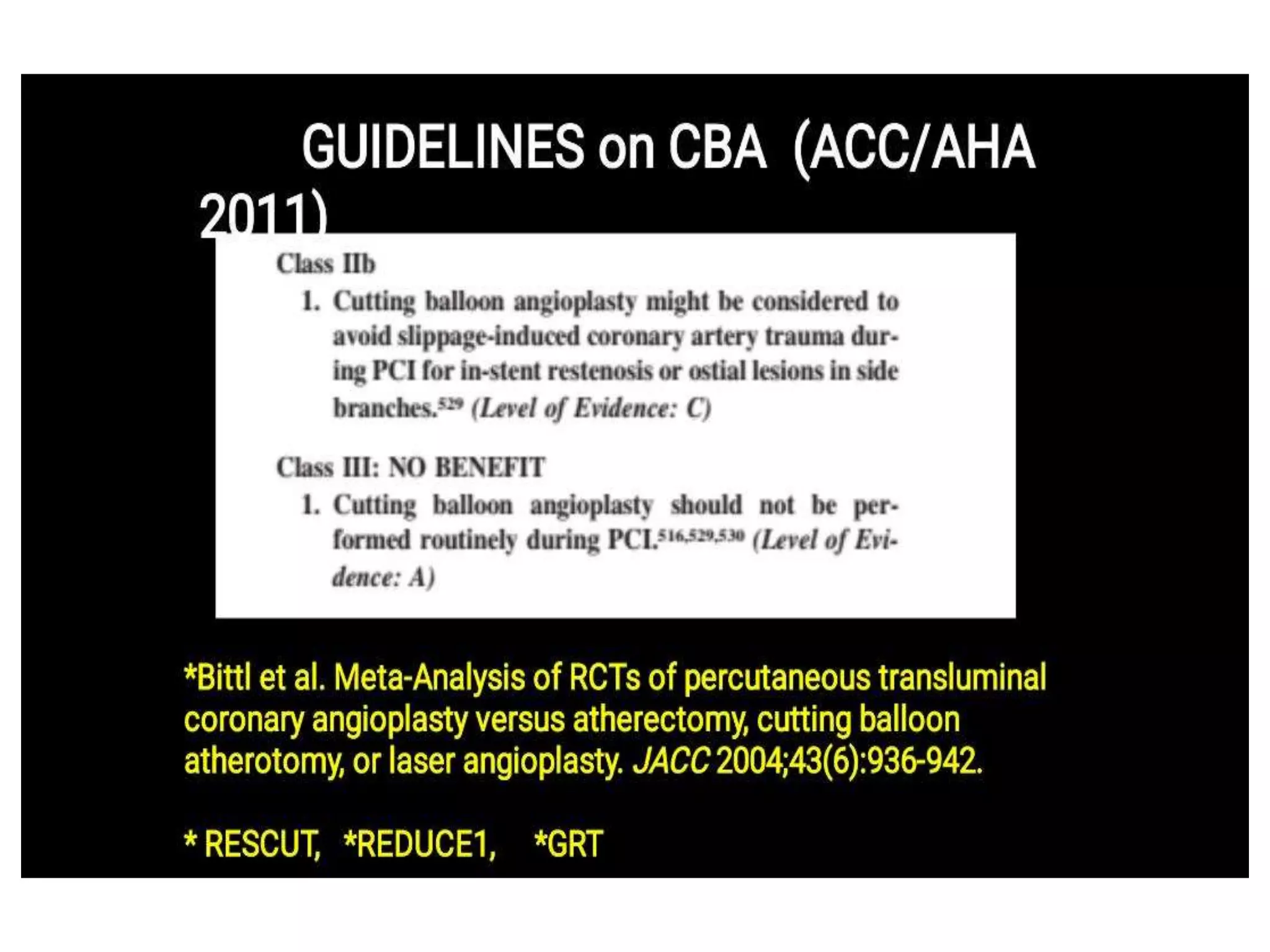
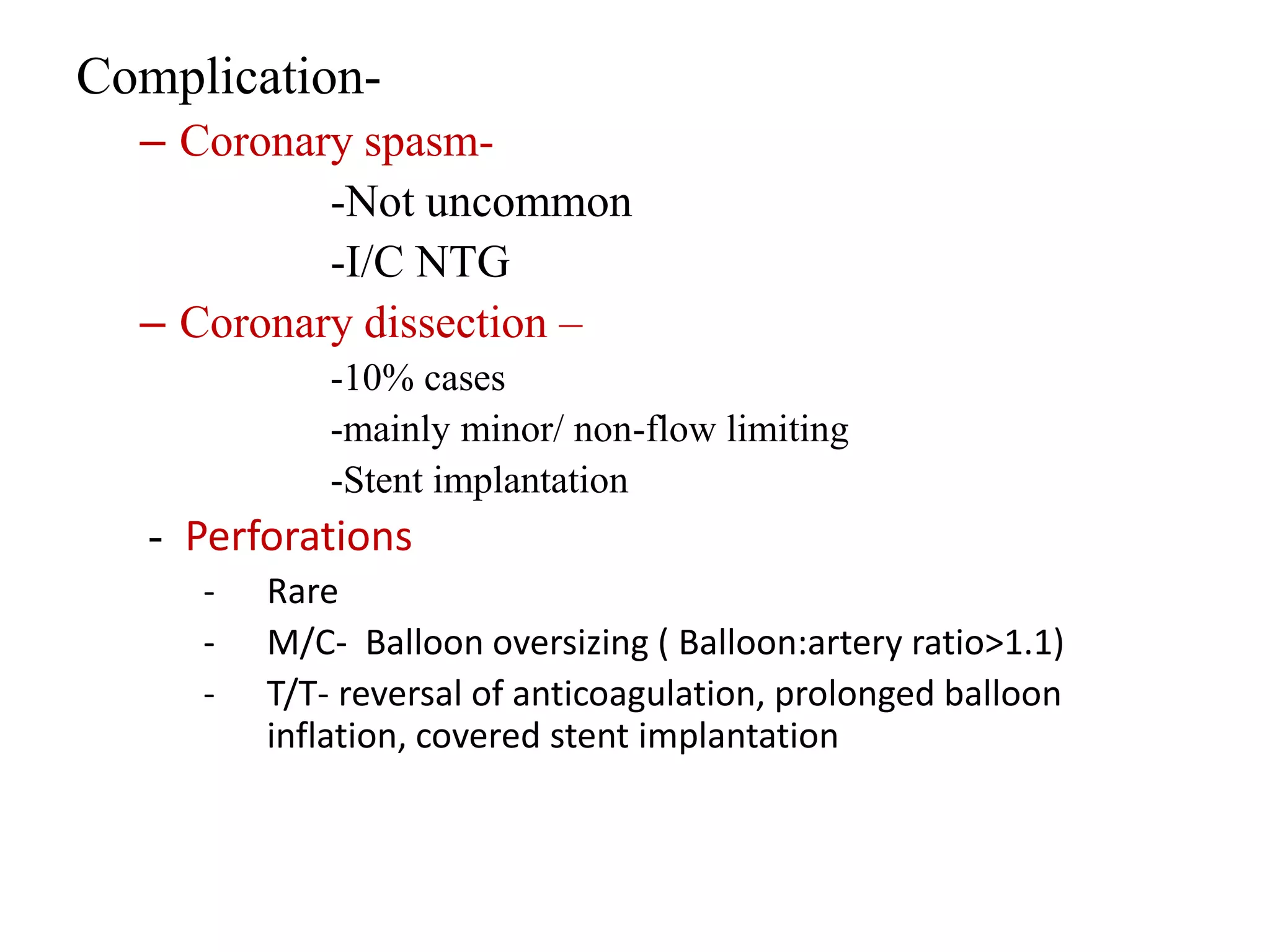
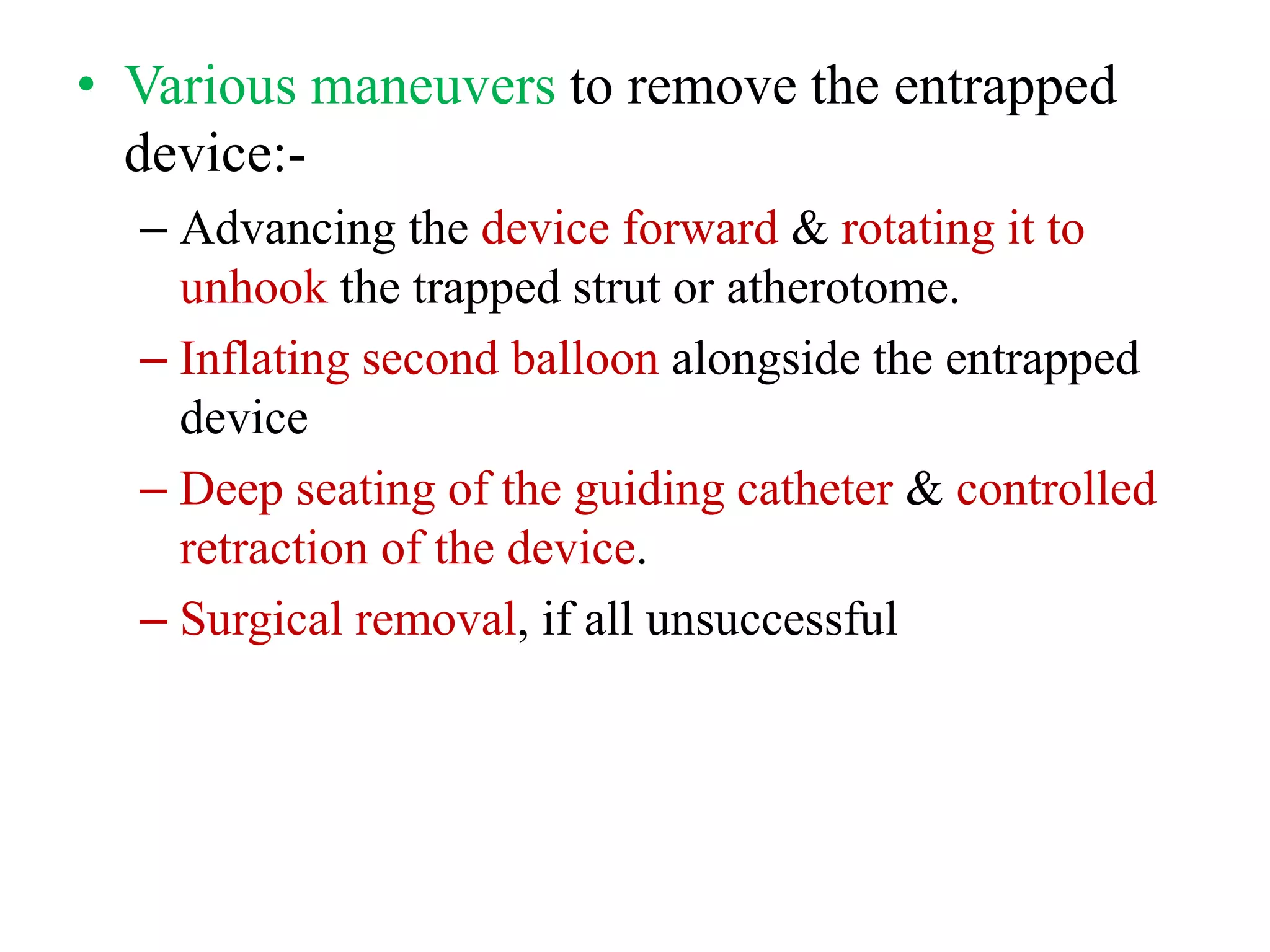
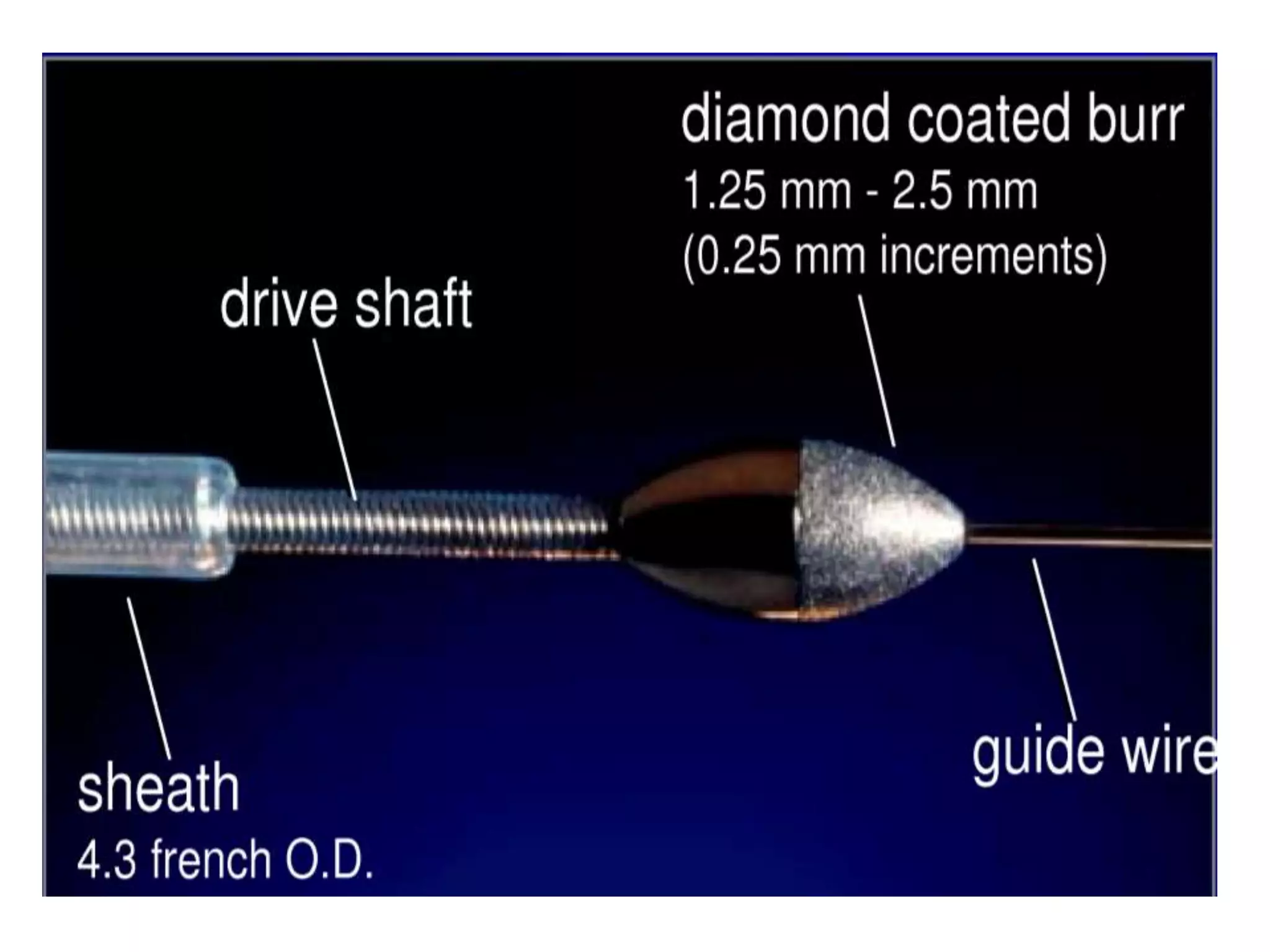
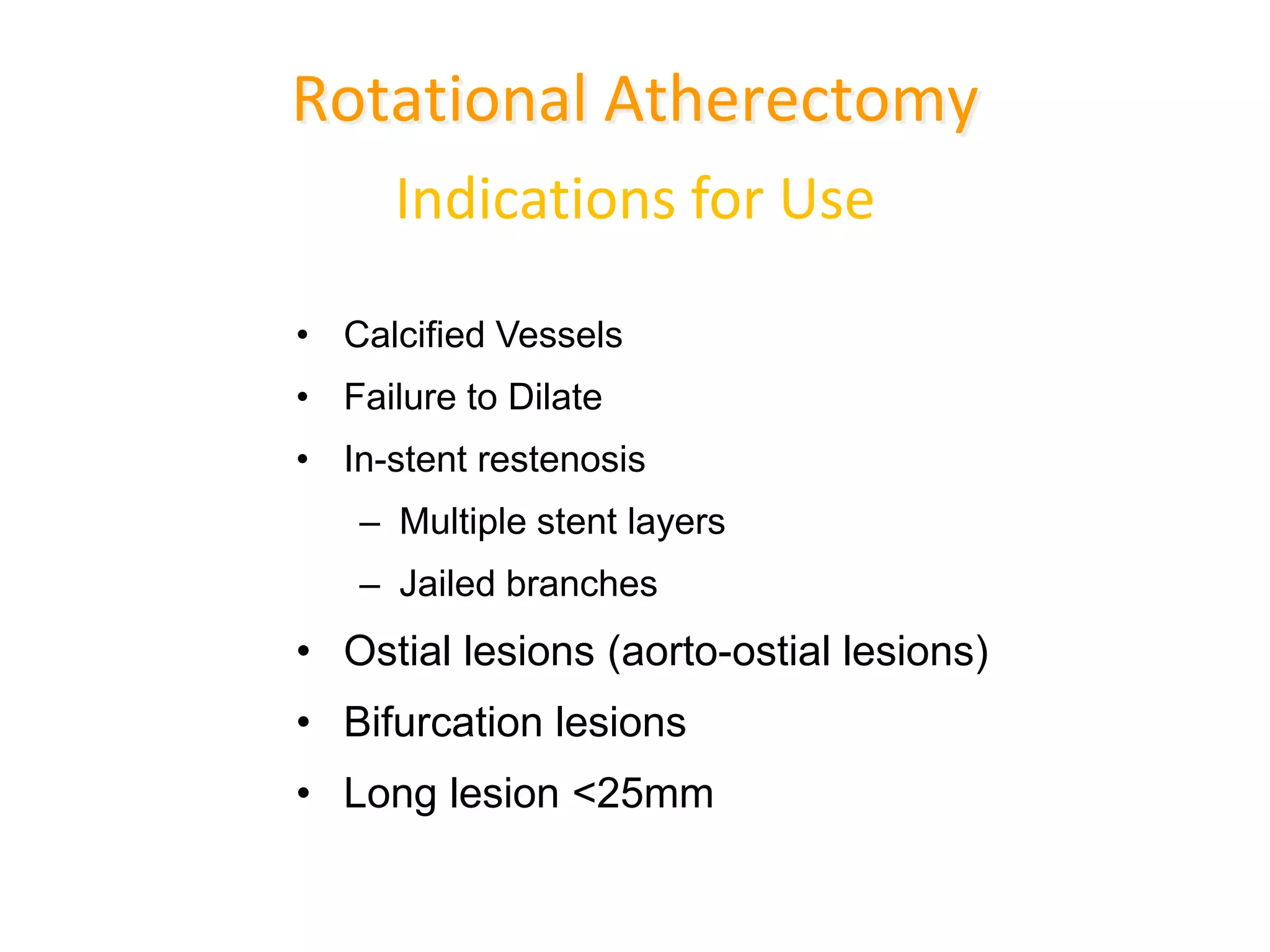
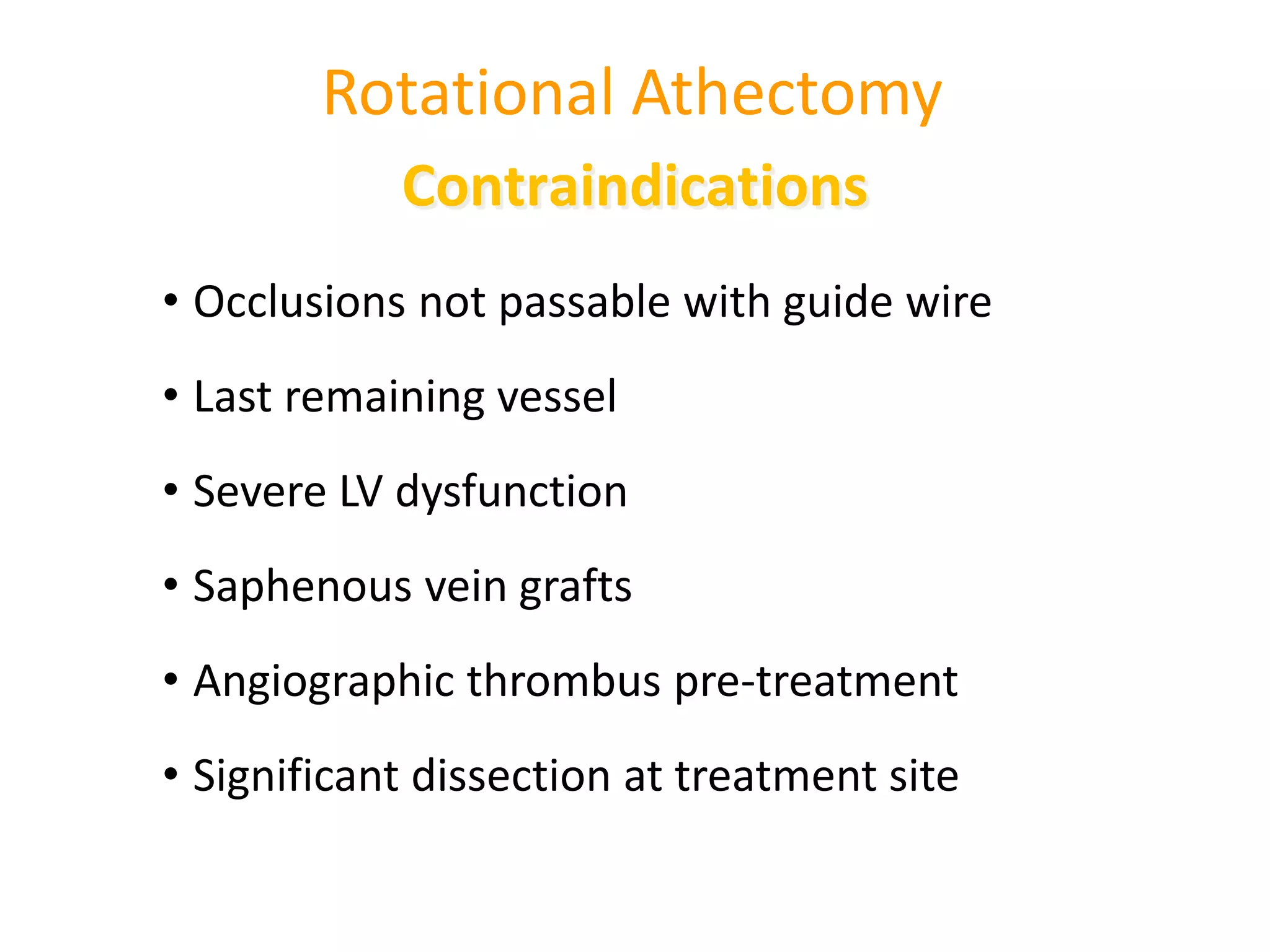
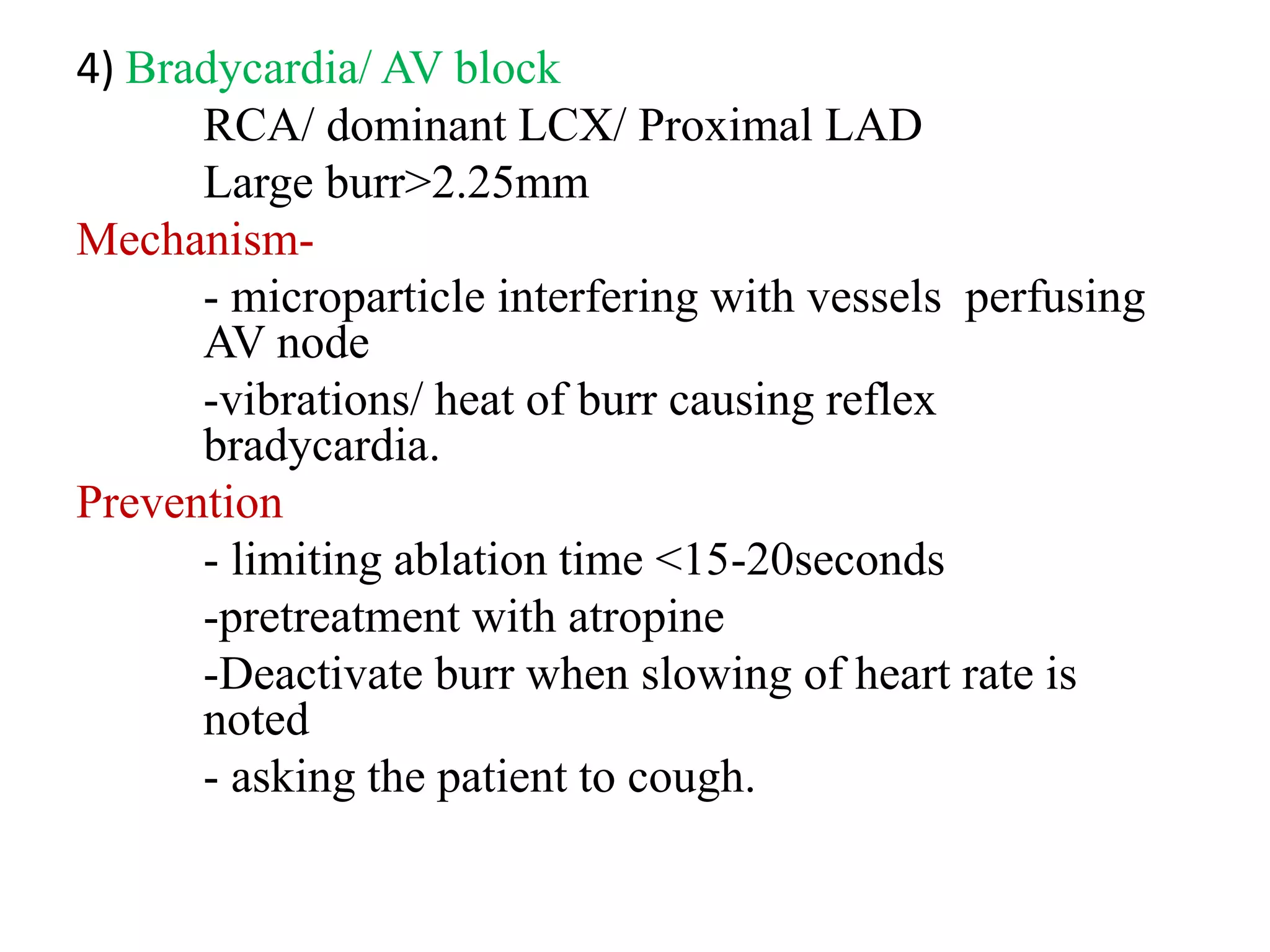
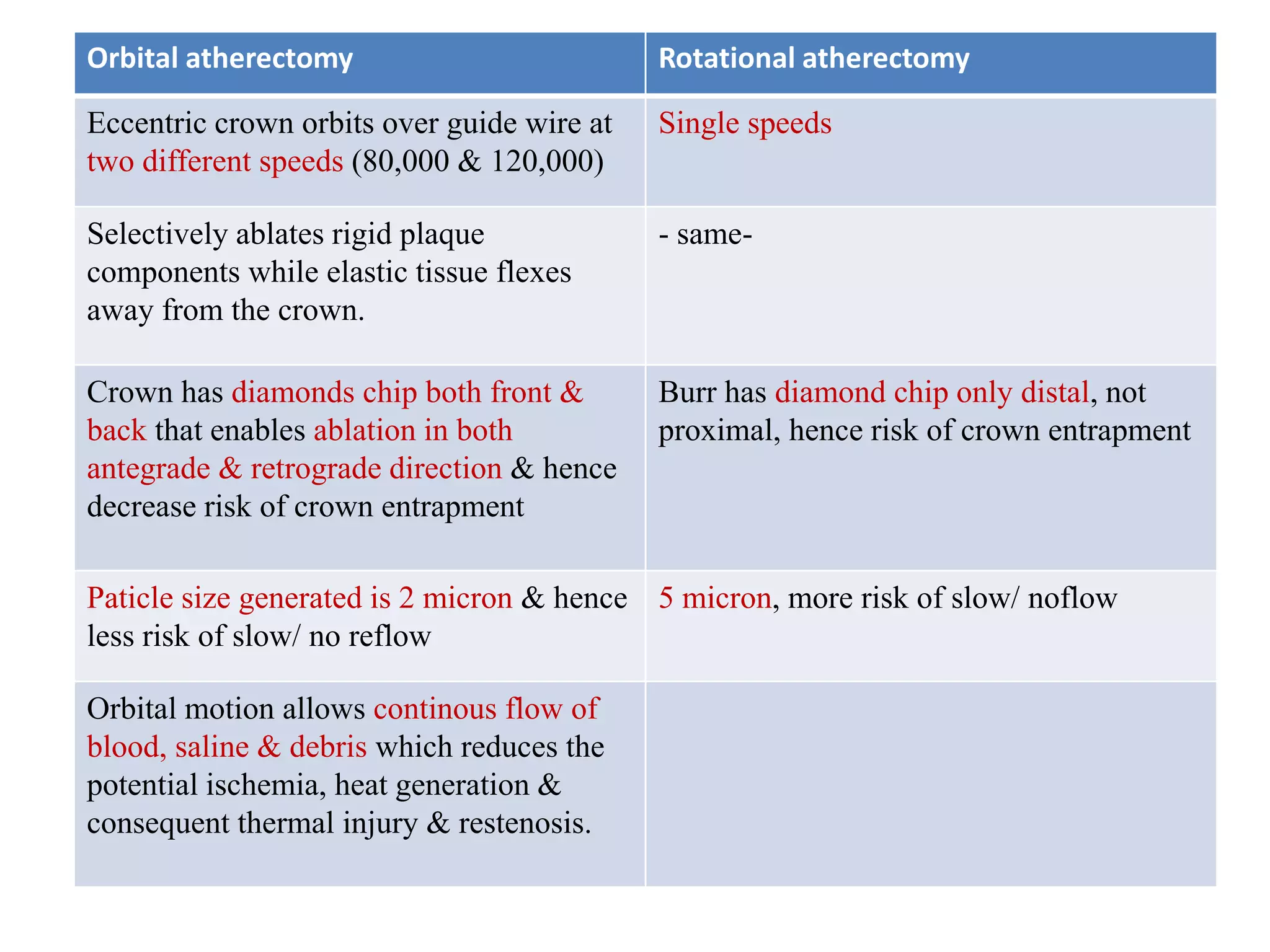
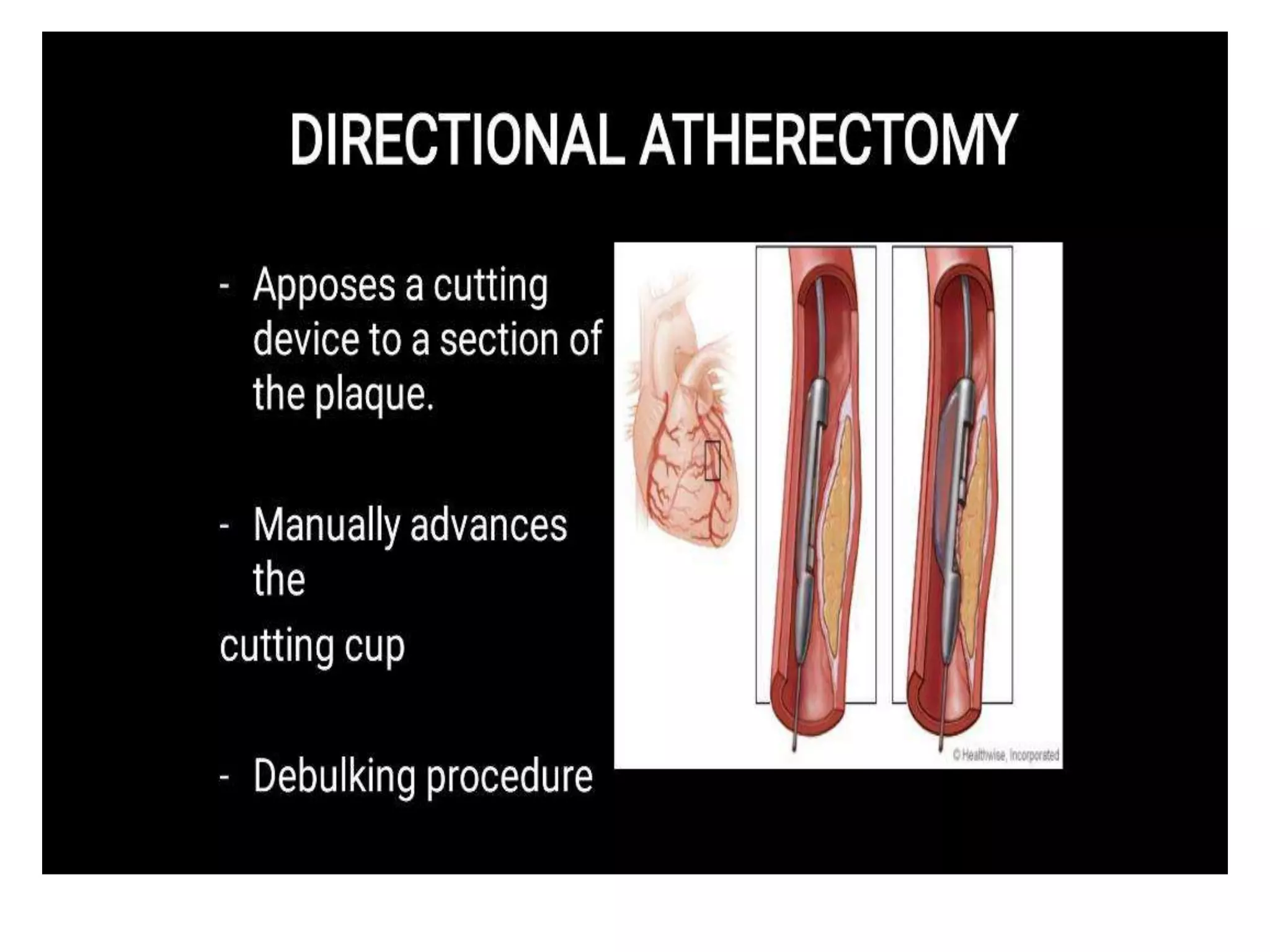
This document discusses various debulking devices used in coronary interventions including cutting balloons, scoring balloons, rotational atherectomy, orbital atherectomy, and laser atherectomy. It provides details on the mechanisms of action, sizes, indications, complications and how to manage complications for each device. The goal of these debulking devices is to remove rigid plaque to facilitate balloon dilatation and stent implantation while minimizing vessel wall injury.