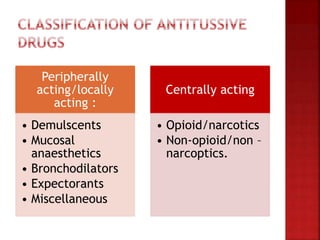
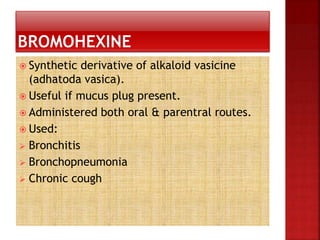
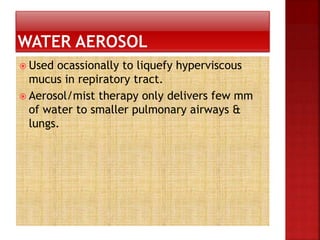
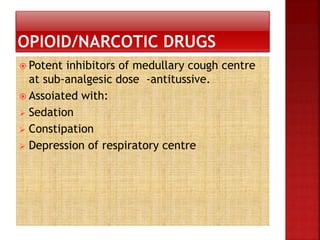
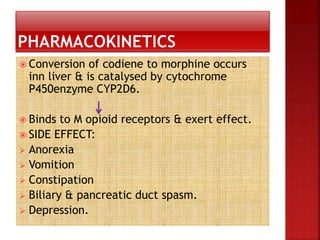
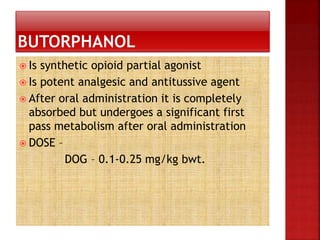
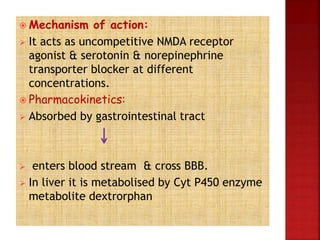
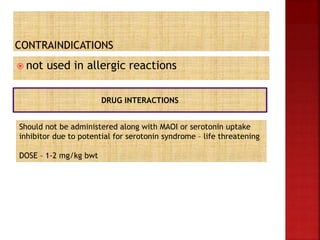
This document discusses various agents used to treat cough. It begins by describing the pathophysiology of cough and differentiating between acute, chronic, and subacute cough. It then categorizes cough medications as peripherally or centrally acting. Peripherally acting medications include demulcents, mucosal anesthetics, bronchodilators, expectorants, and miscellaneous agents. Centrally acting medications include opioid/narcotics and non-opioid/non-narcotics. Specific medications are discussed under each category along with their mechanisms of action, pharmacokinetics, indications, and side effects. The document provides detailed information on commonly used antitussive medications to treat cough.