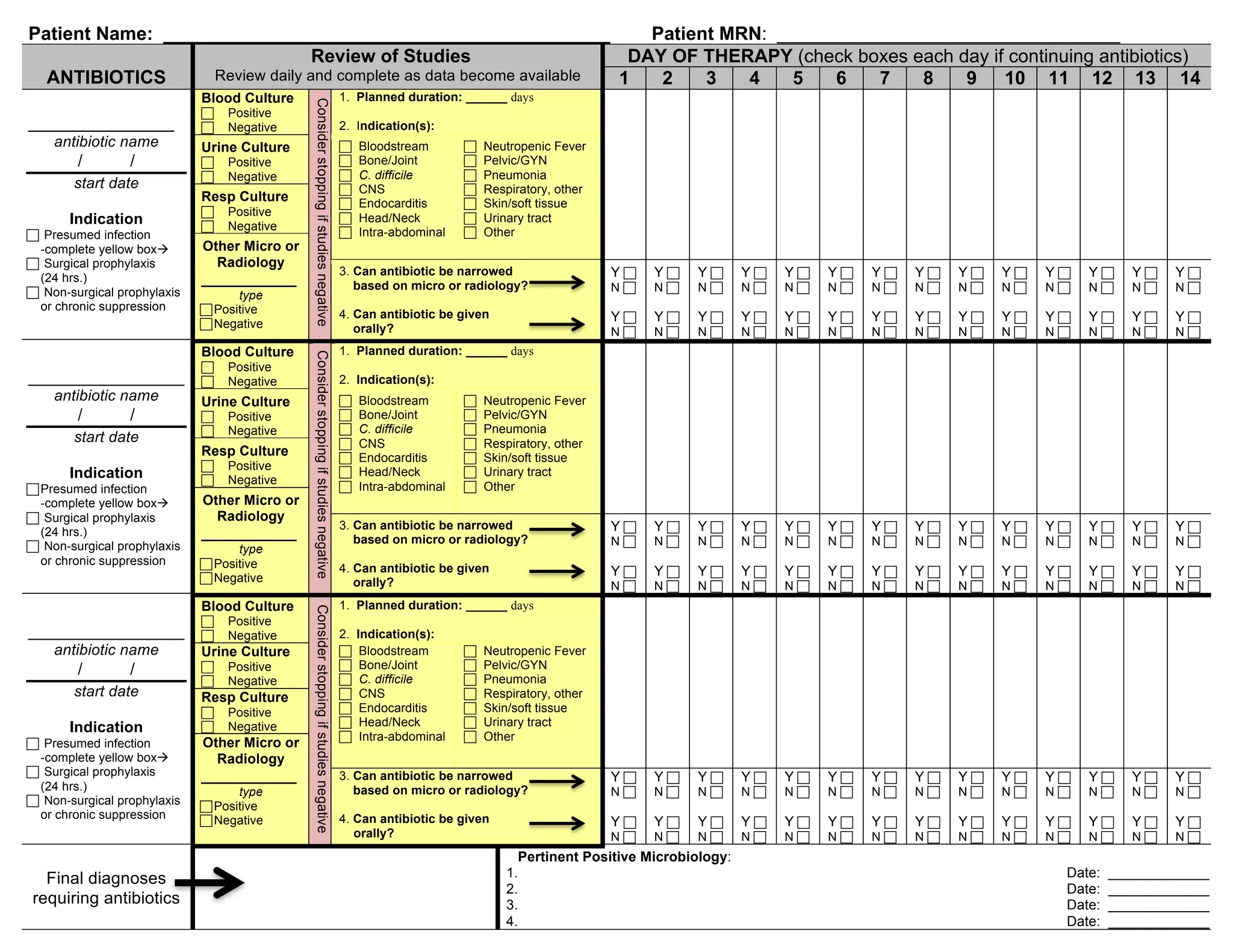
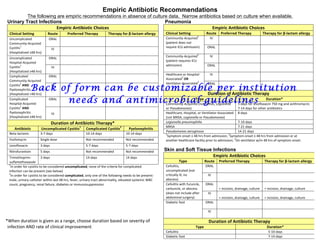
This document contains guidelines for reviewing antibiotic treatment, including indications for use, culture results, and considerations for narrowing or switching to oral antibiotics. It includes sections on empiric antibiotic recommendations for urinary tract infections, pneumonia, and skin and soft tissue infections. For each type of infection, it lists preferred antibiotic therapies and alternatives for beta-lactam allergies, as well as recommended treatment durations.