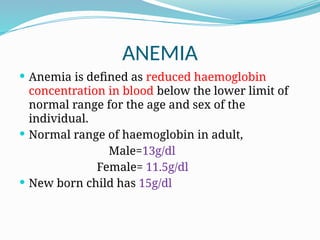
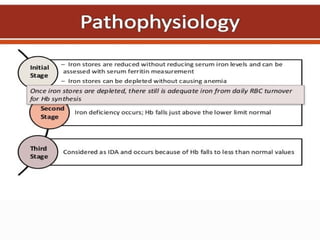
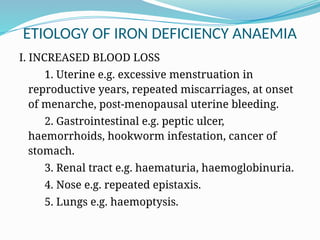
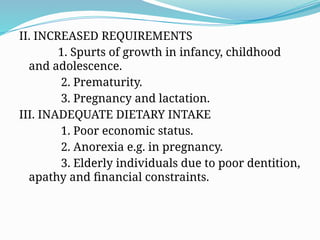
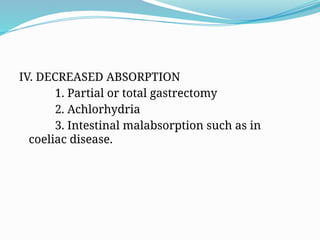
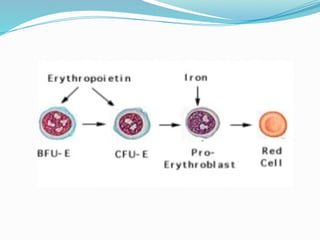
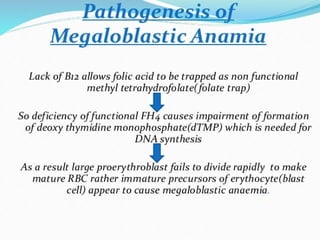
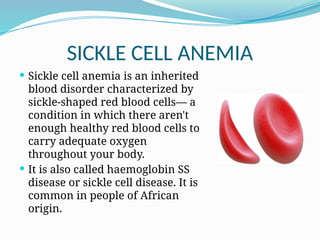
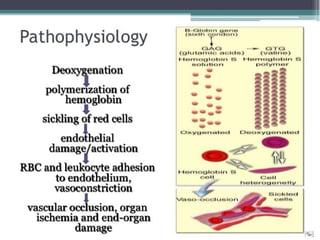
Hematological diseases primarily affect blood and blood-forming organs and include conditions like anemia and sickle cell anemia. Anemia, particularly iron deficiency anemia, is a significant global issue characterized by insufficient healthy red blood cells, often due to blood loss, inadequate dietary intake, or absorption issues. Other forms of anemia, such as megaloblastic anemia and sickle cell anemia, have distinct etiologies and impact on health, necessitating specific diagnostic and treatment approaches.