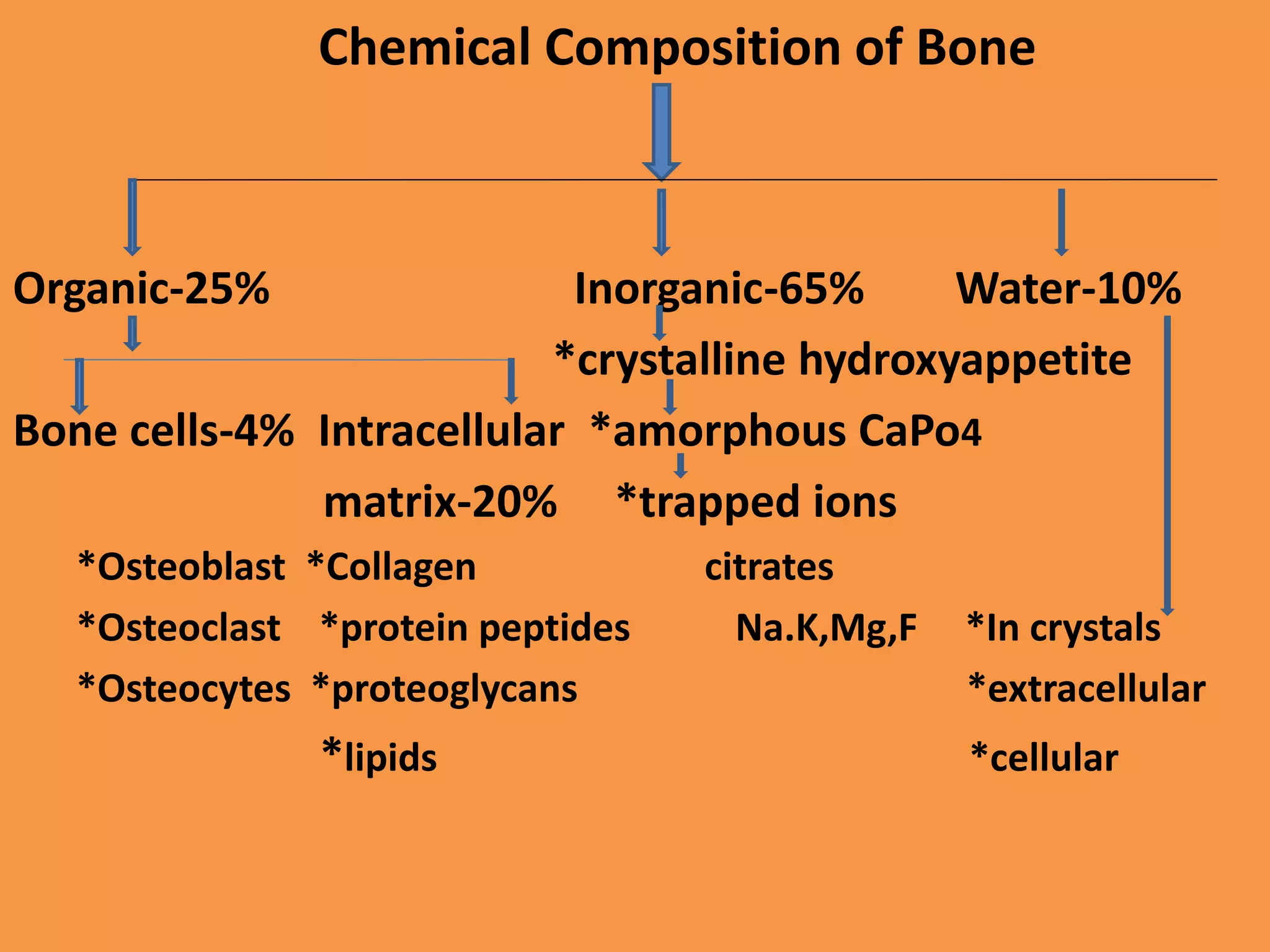
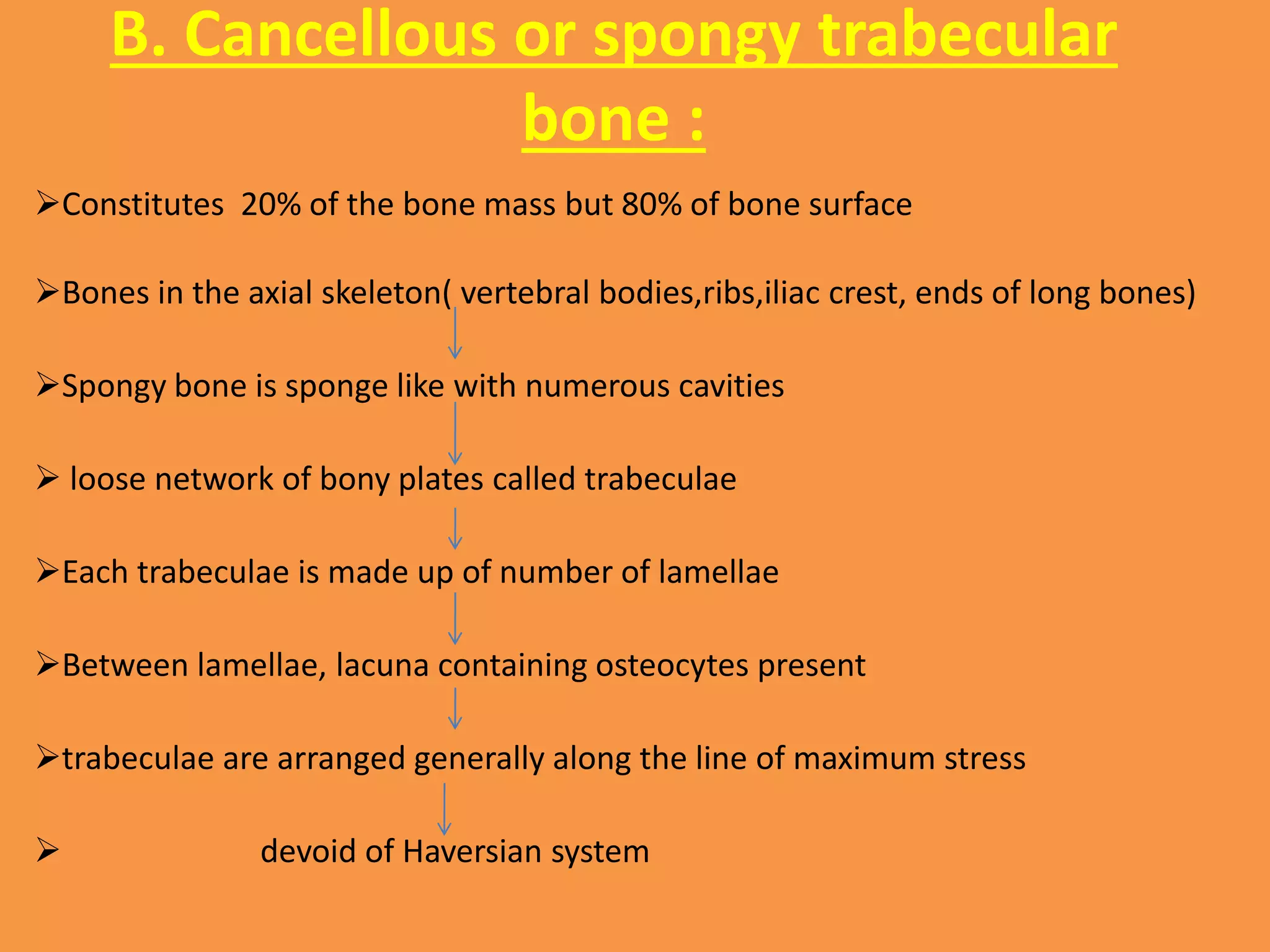
This document discusses the anatomy of bone, including its structure, function, classification, development, and blood supply. It describes bone as a composite connective tissue made up of organic components like bone cells and collagen and inorganic components like calcium crystals. It classifies bone tissue into woven bone, lamellar bone, cortical bone, and cancellous bone. Bone development occurs through either intramembranous or endochondral ossification. Finally, it outlines the dynamic process of bone remodeling carried out by osteoblasts, osteoclasts, and the blood supply to bone.