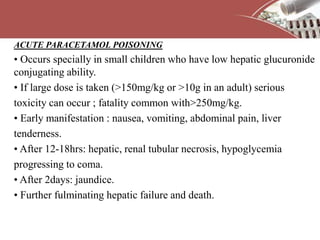
The document discusses non-steroidal anti-inflammatory drugs (NSAIDs) and their role in periodontal disease treatment. It covers the definition of NSAIDs, their history of use, classification, mechanisms of action including inhibition of prostaglandin synthesis, and various types including salicylates, propionic acid derivatives, and selective COX-2 inhibitors. NSAIDs are proposed to have host modulatory properties for periodontal disease by suppressing inflammation and bone resorption mediated by prostaglandins. However, risks of adverse gastrointestinal effects must be weighed against potential benefits for periodontitis.