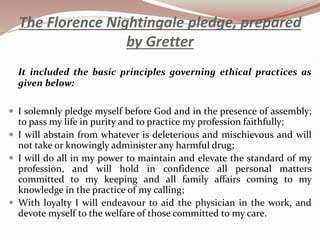
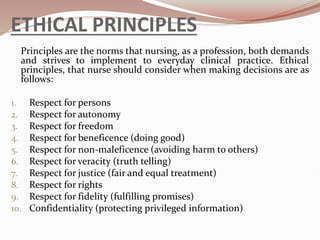
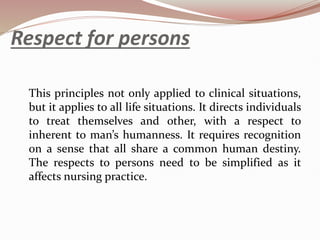
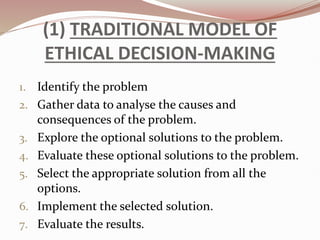
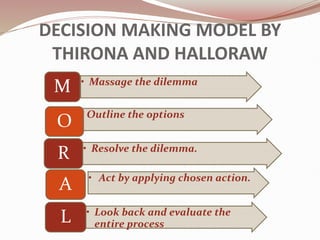
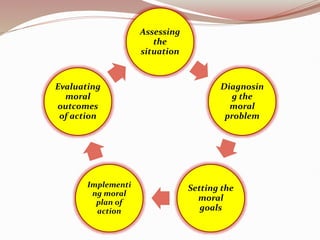
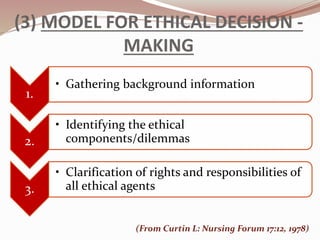
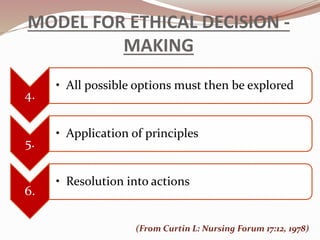
The document discusses the ethical aspects of nursing, focusing on principles such as respect for persons, beneficence, non-maleficence, and justice. It outlines the role of nurses in ethical decision-making, emphasizing their responsibility to promote health and alleviate suffering while adhering to professional codes of ethics. Additionally, it highlights the challenges of ethical dilemmas and the importance of decision-making models in nursing practice.