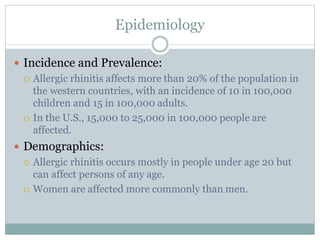
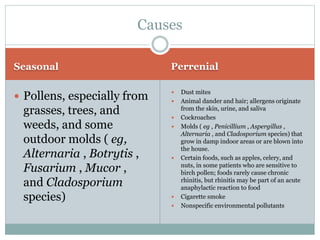
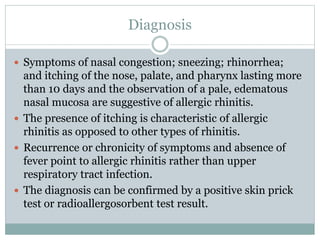
Allergic rhinitis is a chronic inflammatory disease of the nasal passages affecting over 20% of the population. It is characterized by sneezing, nasal congestion, rhinorrhea, and itching caused by an immune response to allergens such as pollen, dust mites, and animal dander. Treatment involves identifying and avoiding triggers, using intranasal corticosteroids as first line therapy to reduce inflammation, and oral antihistamines to relieve symptoms. Immunotherapy may be used for severe, treatment-resistant cases.