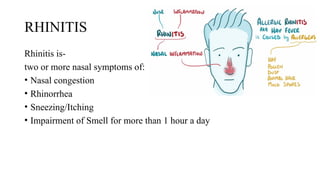
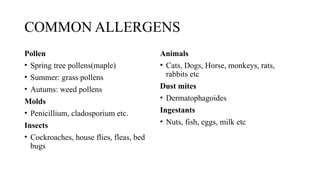
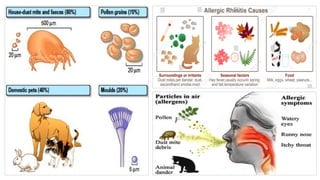
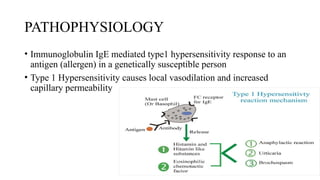
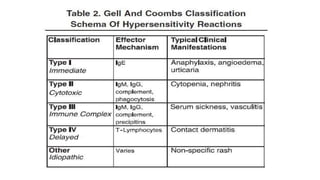
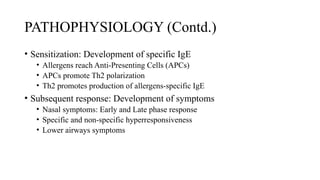
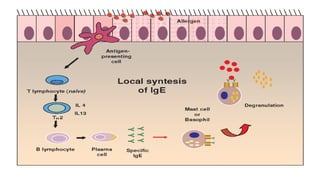
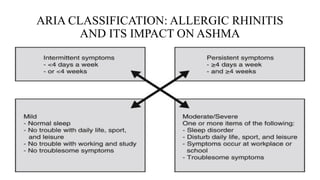
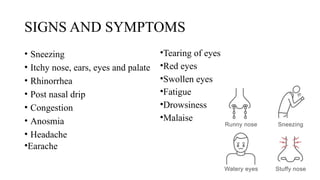
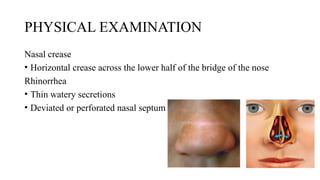
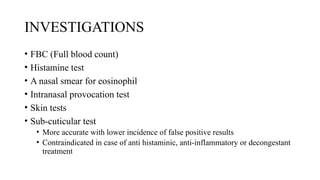
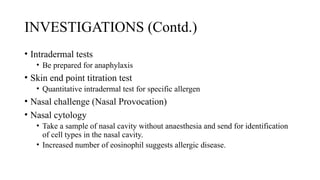
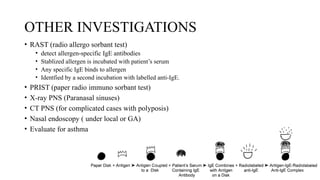
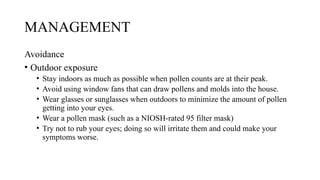
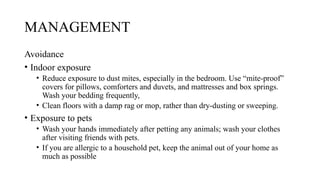
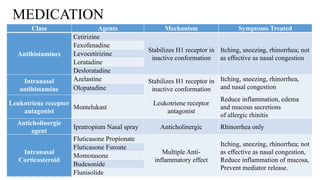
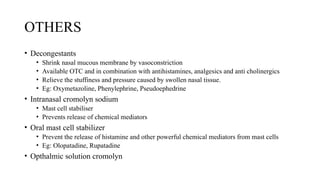
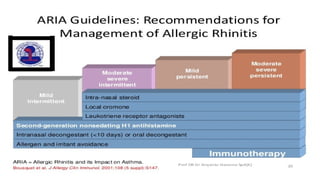
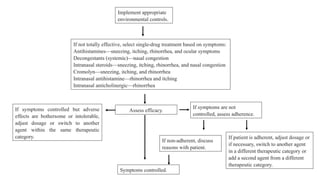
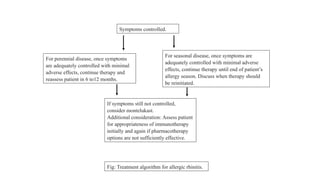
Allergic rhinitis is a common condition marked by nasal symptoms such as congestion, sneezing, and rhinorrhea, significantly affecting 10-25% of the population, especially children and adolescents. It is triggered by allergens and characterized by an IgE-mediated hypersensitivity response, classified into seasonal and perennial forms. Management includes avoidance of allergens, use of medications like antihistamines and intranasal corticosteroids, and in some cases, immunotherapy.