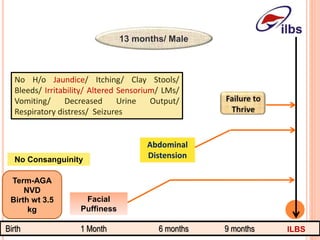
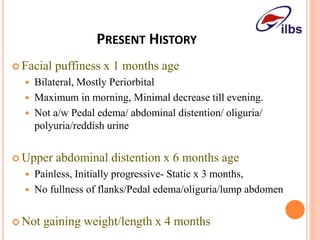
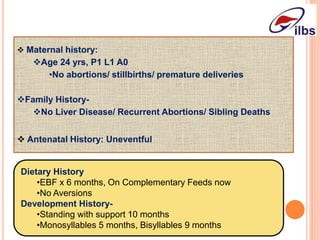
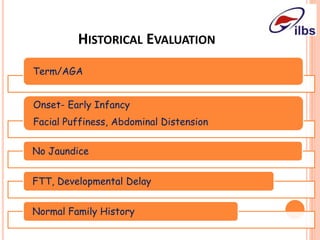
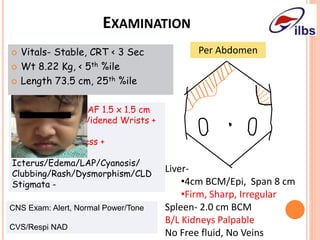
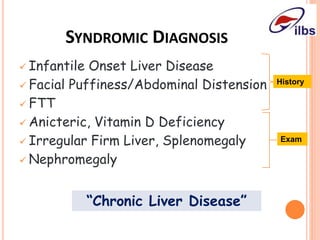
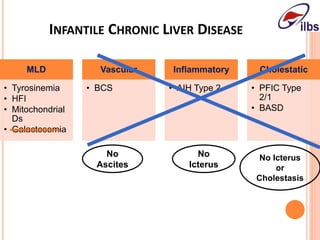
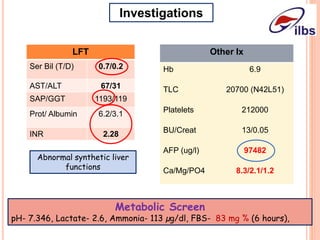
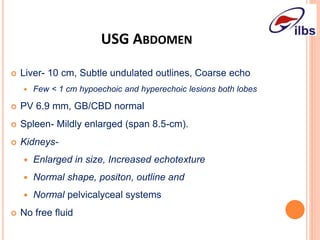
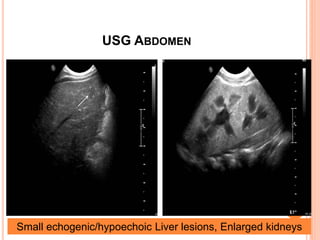
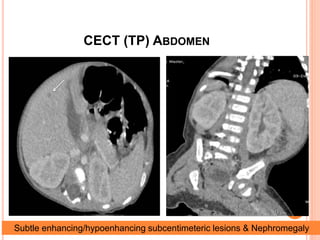
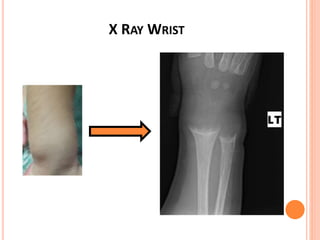
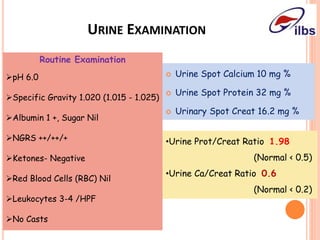
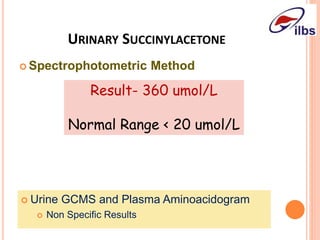
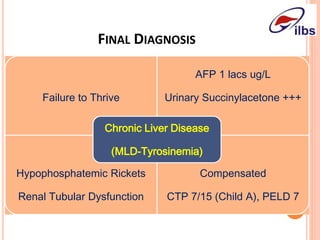
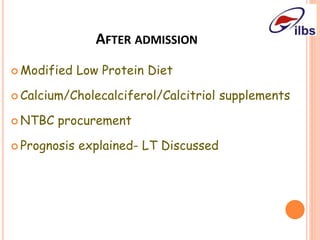
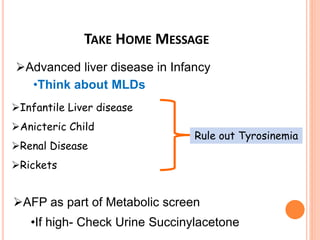
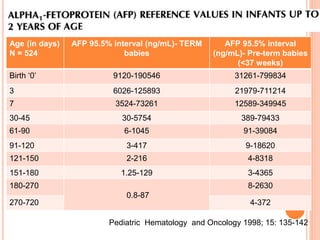
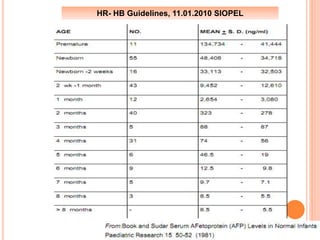
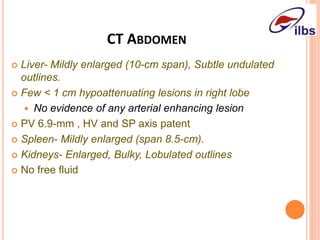
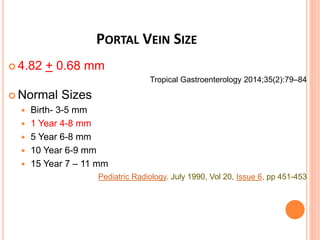
This document presents a case study of an infant presenting with facial puffiness, abdominal distension, and failure to thrive, ultimately leading to the diagnosis of chronic liver disease and renal tubular dysfunction. The infant exhibited signs of infantile liver disease, including elevated alpha-fetoprotein and abnormalities in liver function tests, alongside renal and nutritional issues. The management plan included a modified low protein diet and vitamin supplementation, with specific recommendations to rule out conditions such as tyrosinemia.