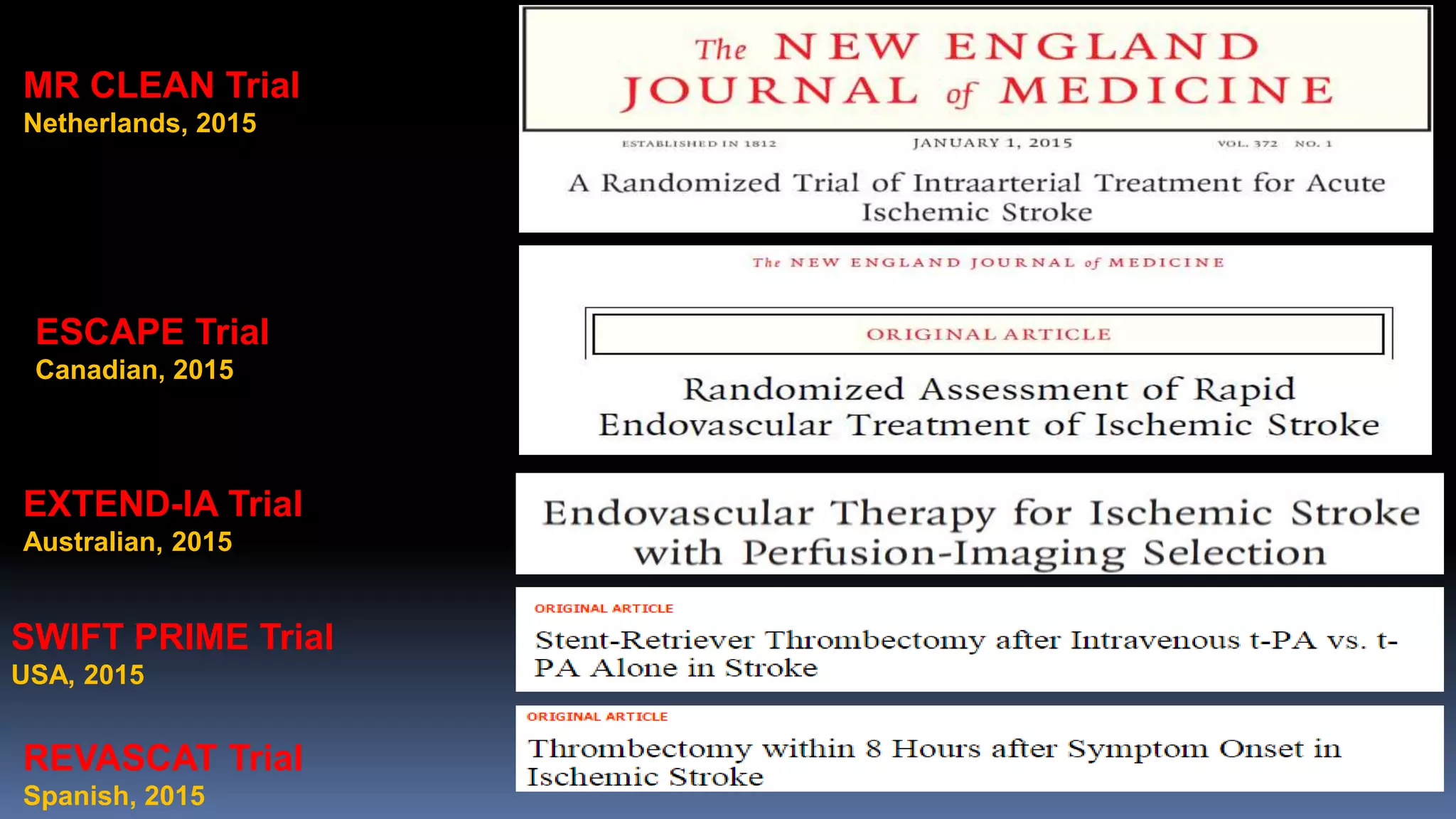
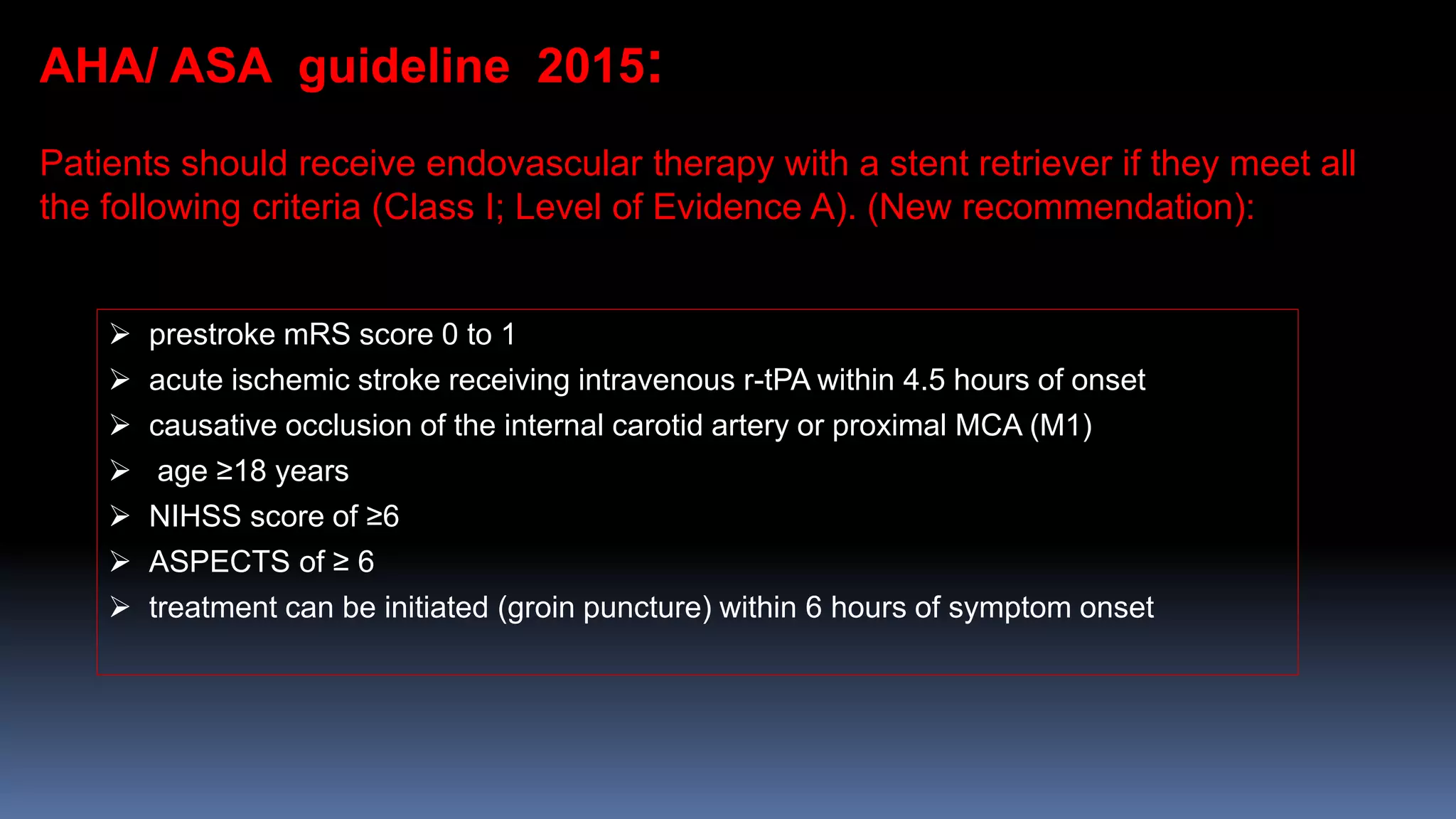
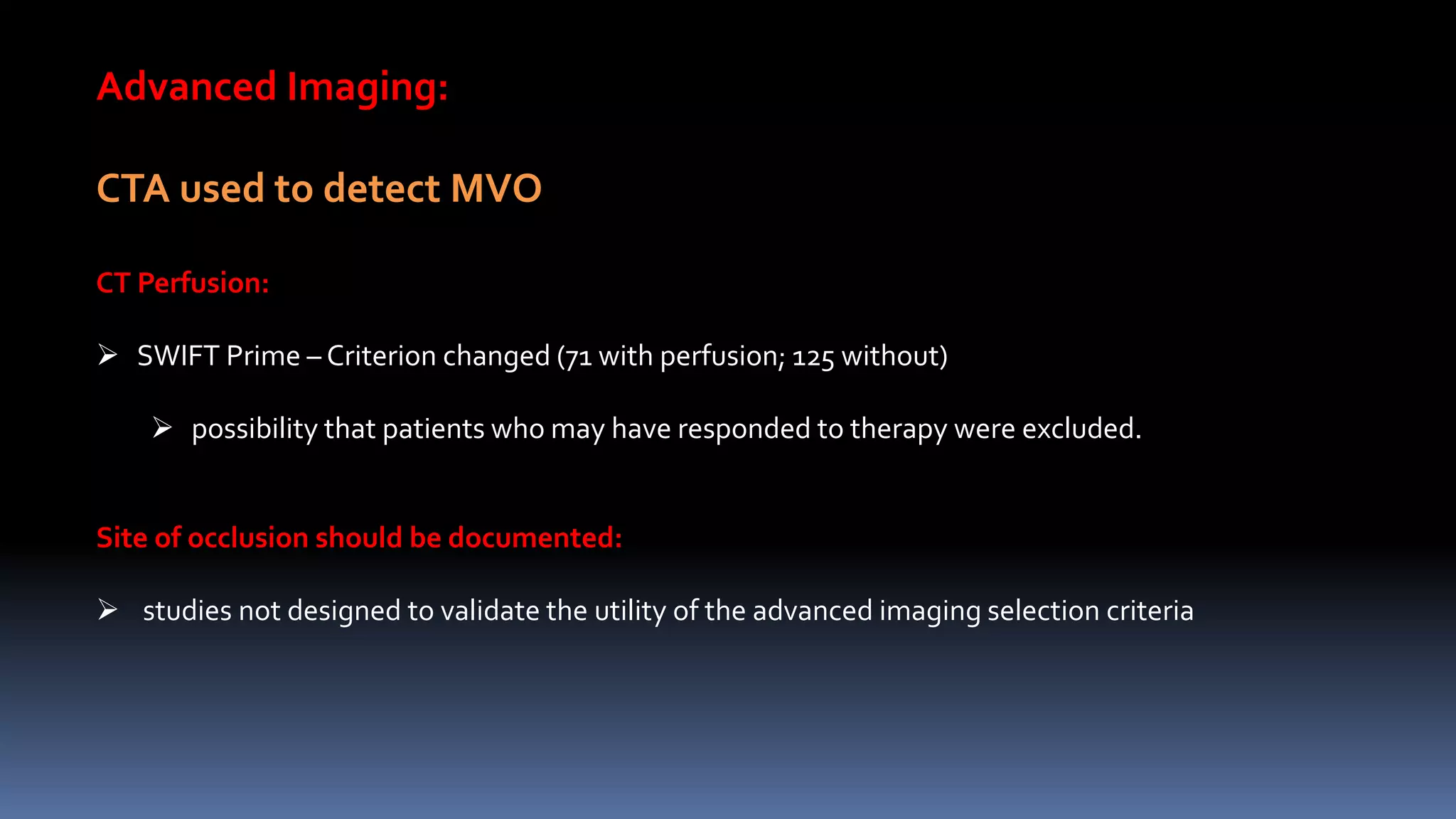
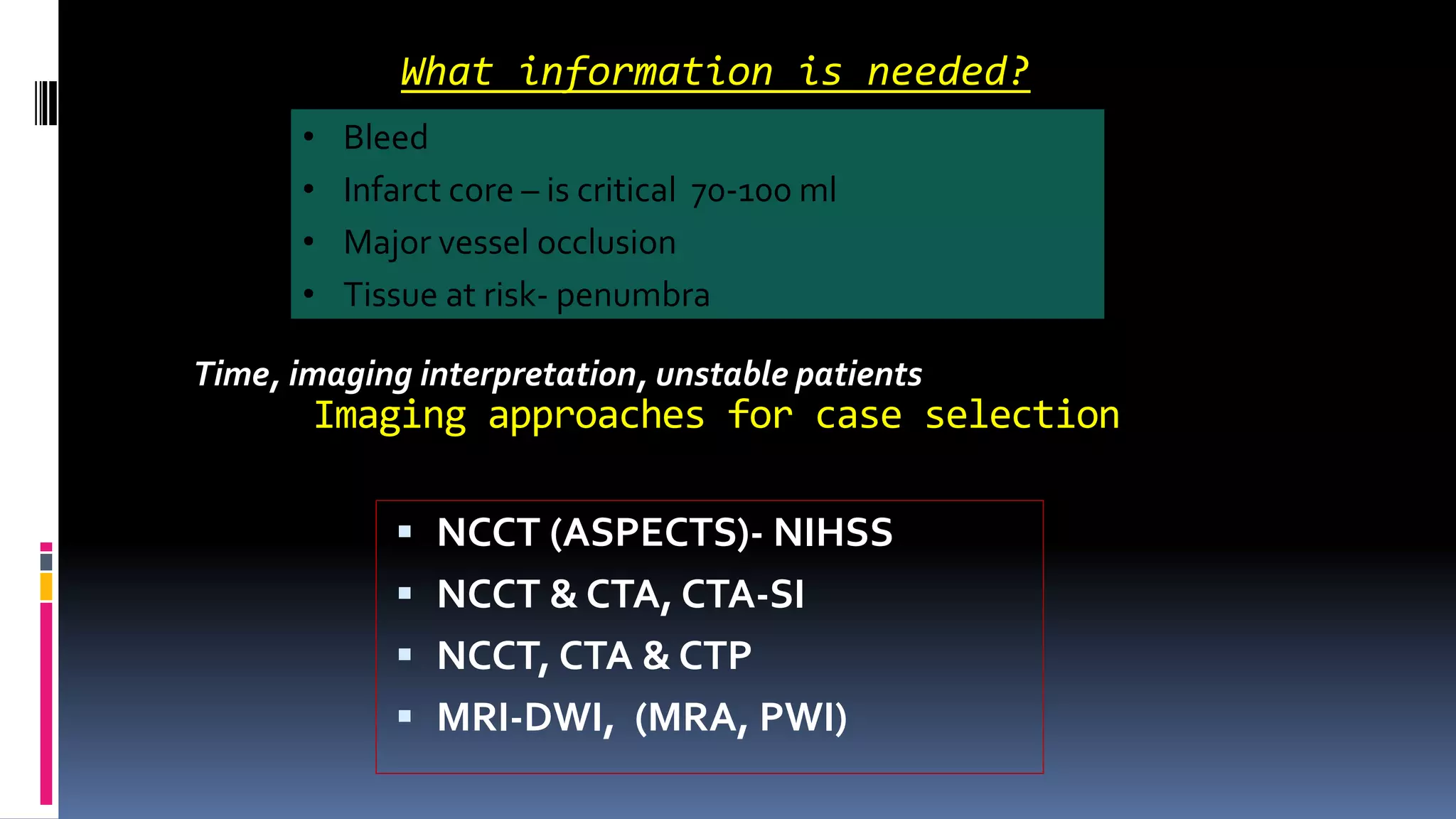
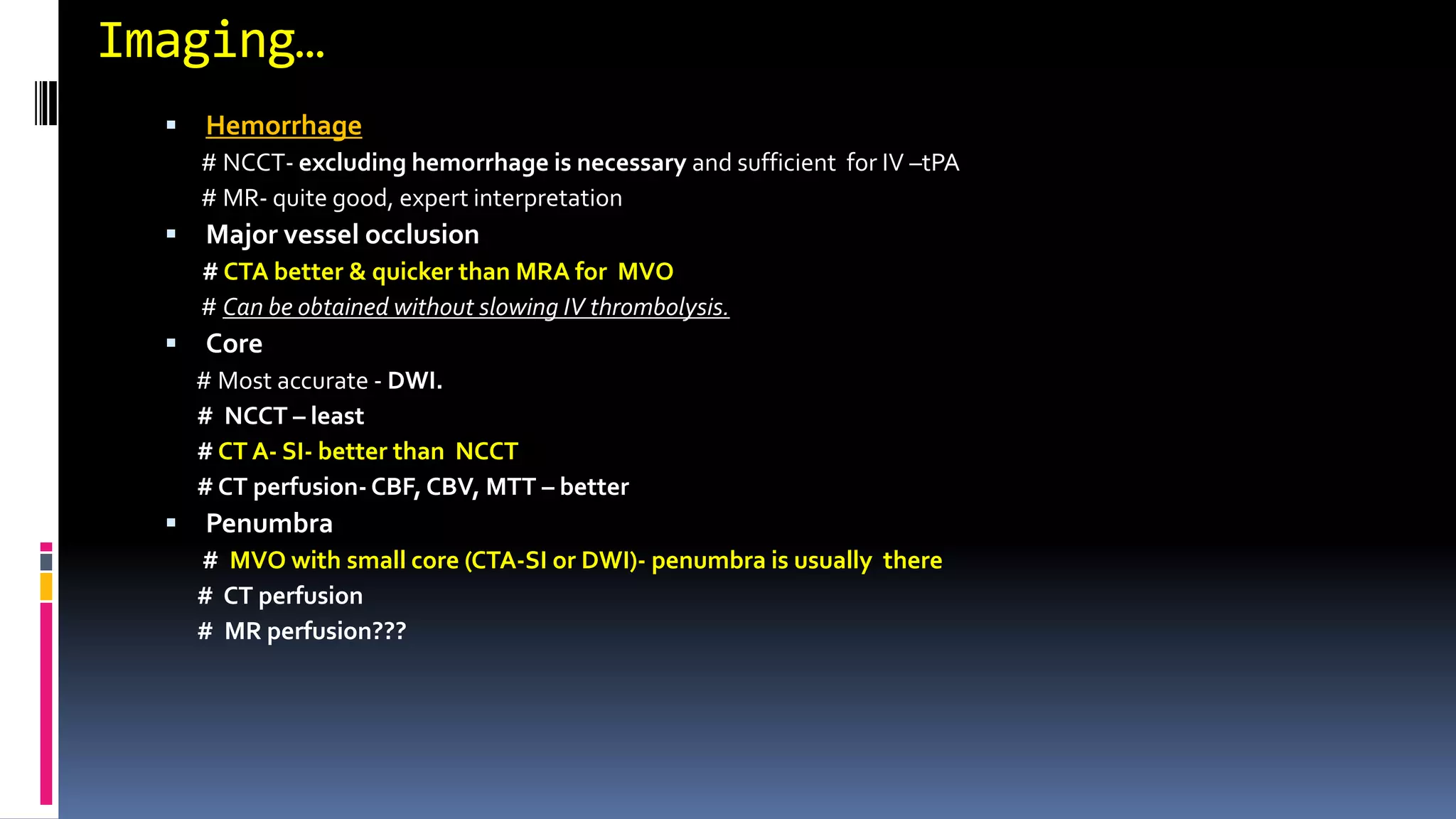
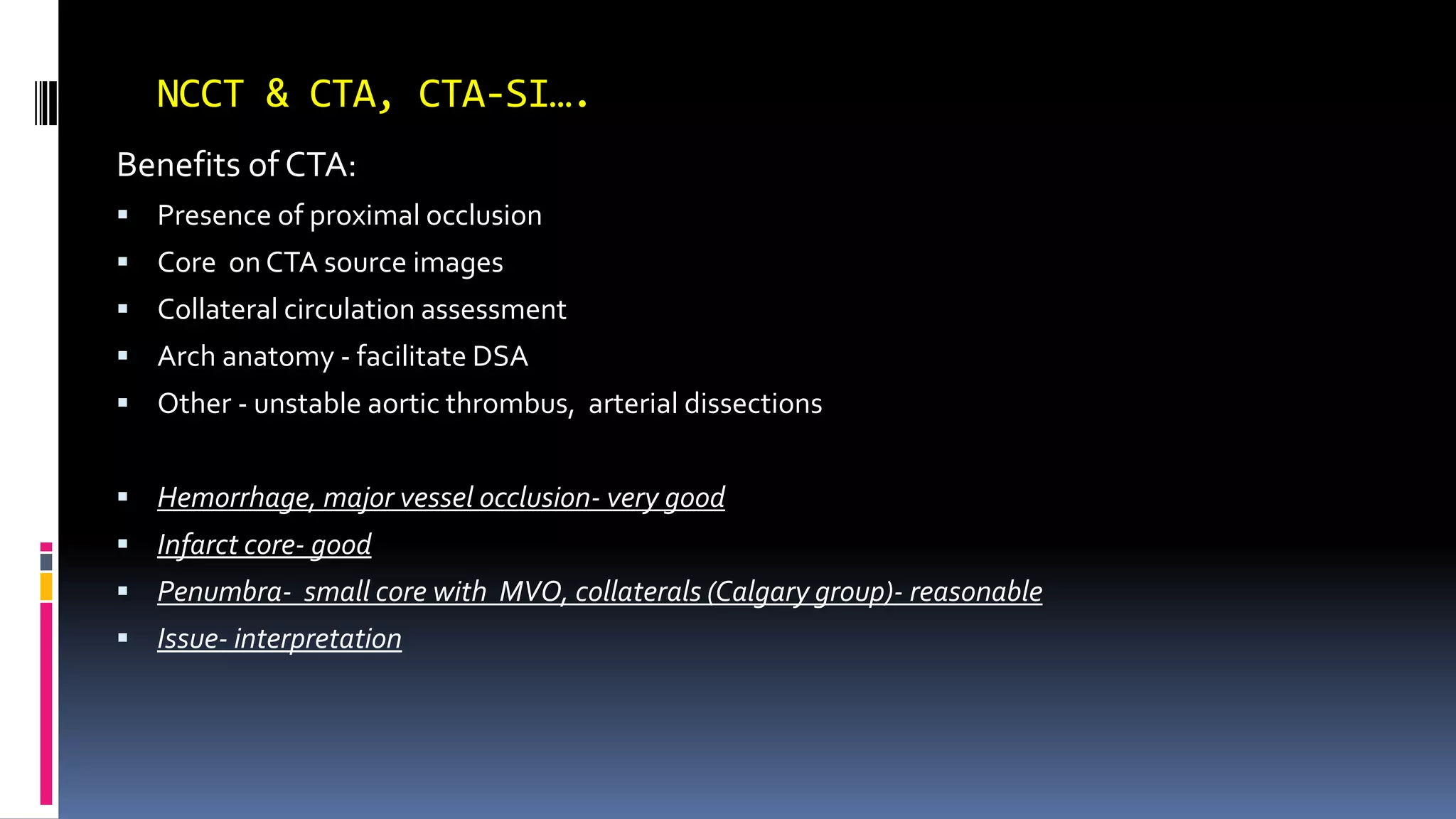
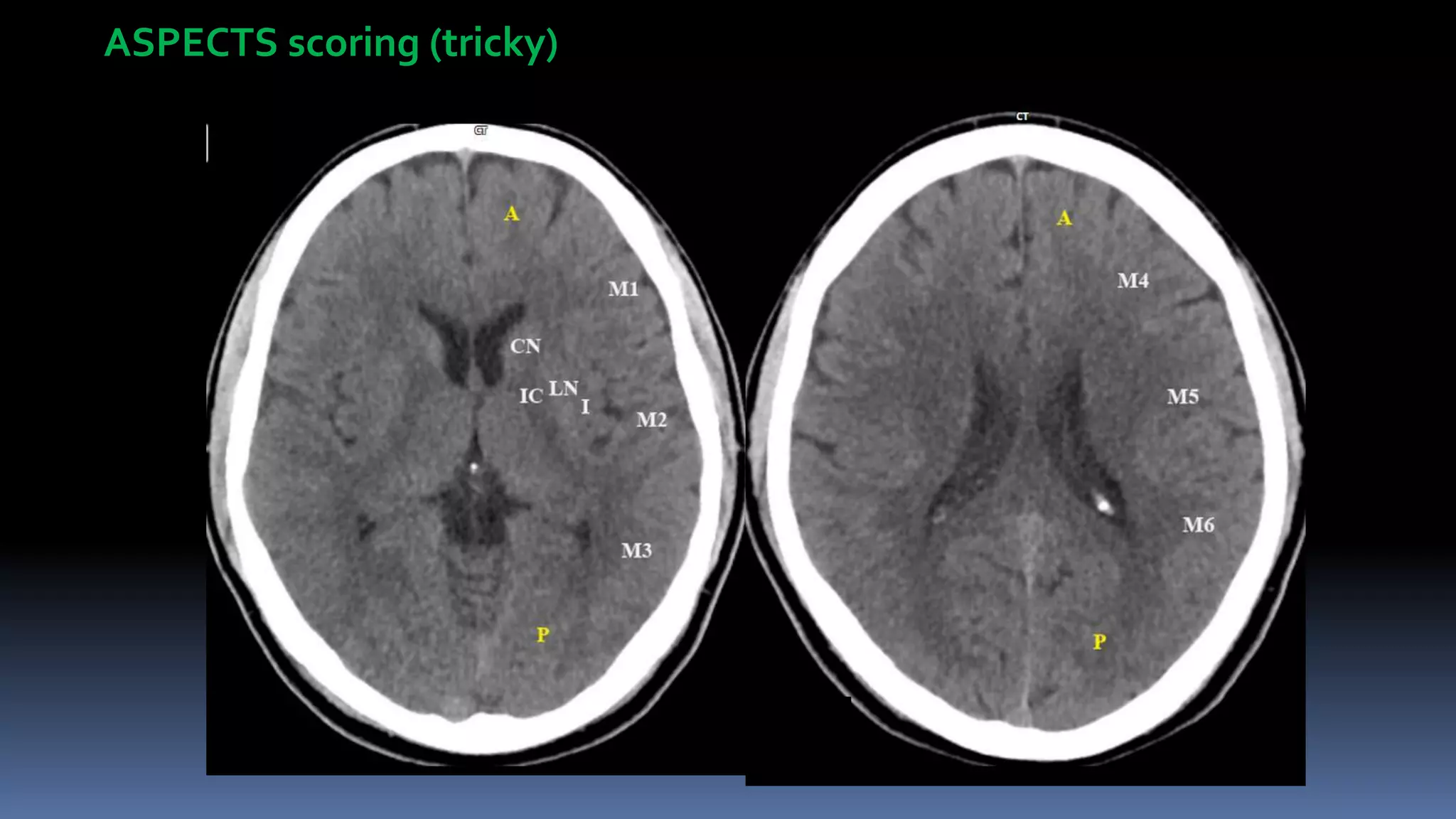
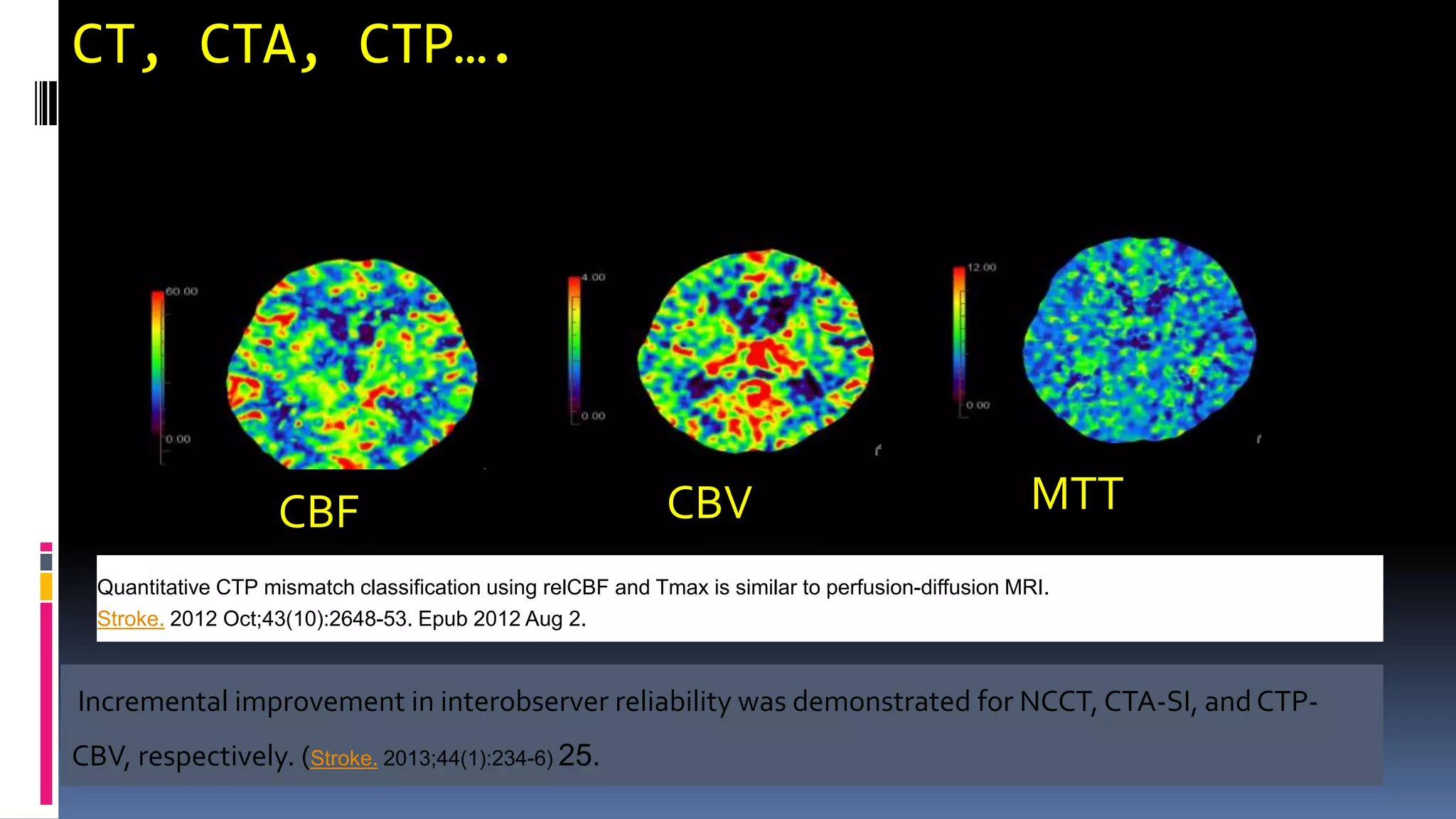
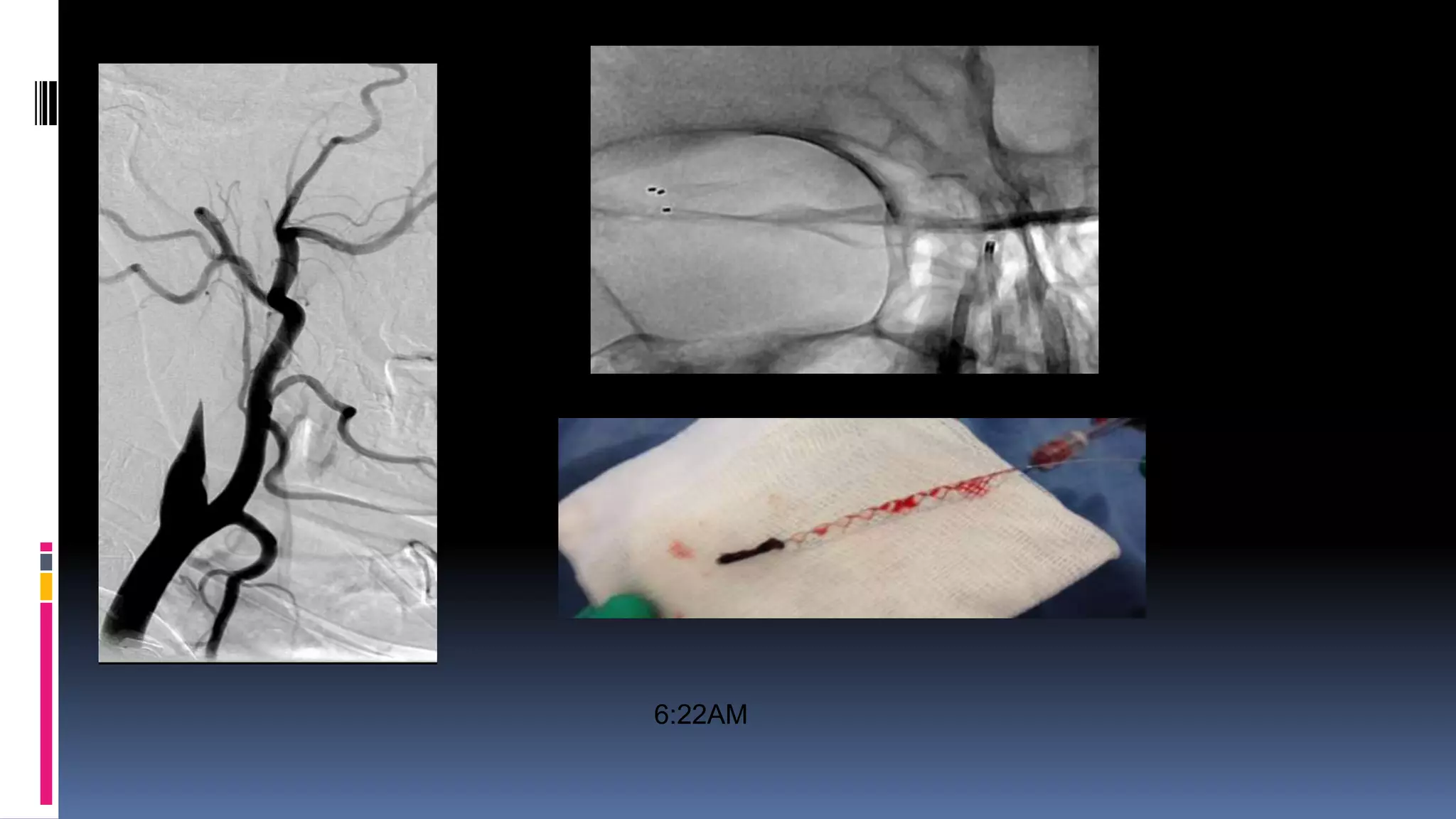
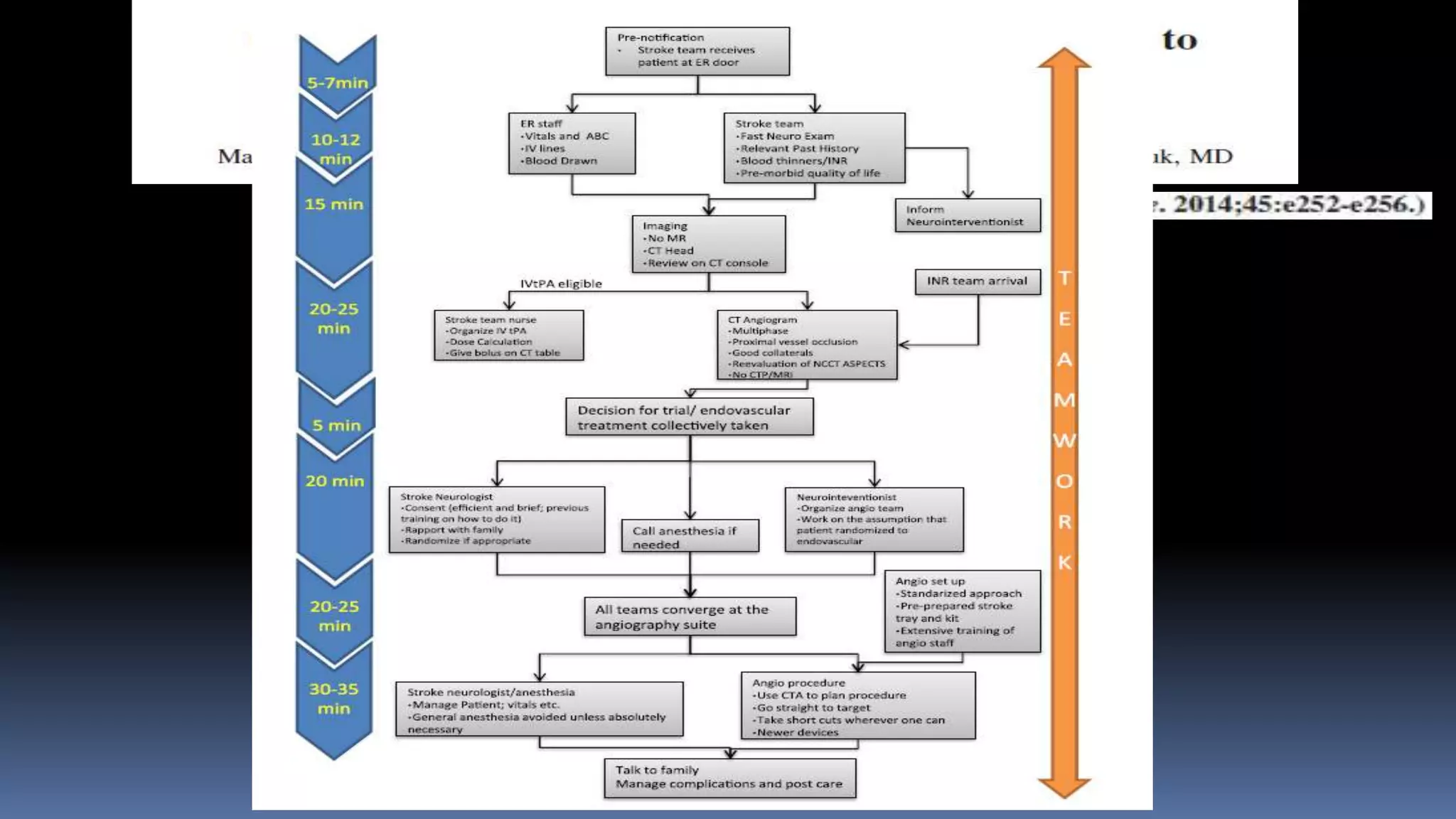
This document summarizes advances in imaging for ischemic stroke. It discusses the role of CT angiography (CTA) in detecting vessel occlusion and infarct core. Several major clinical trials demonstrated the benefits of endovascular therapy for certain patients. Guidelines now recommend endovascular treatment for those meeting specific criteria within 6 hours of onset. CT perfusion can identify penumbra and guide patient selection. While MRI is most accurate for core imaging, the time required may delay treatment. Faster door-to-treatment times are important to improve outcomes. Advanced imaging like CTA helps identify patients most likely to benefit from endovascular intervention.