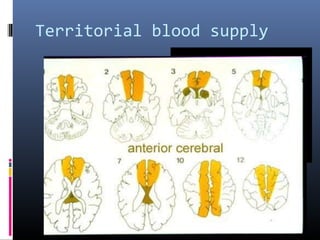
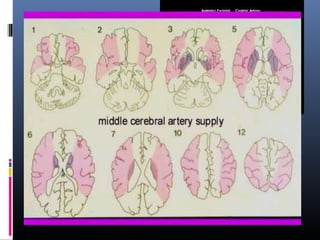
This document discusses imaging techniques used in ischemic stroke. It covers:
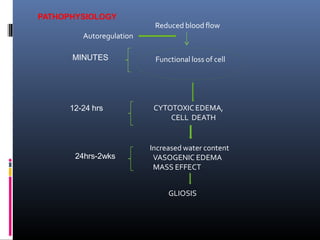
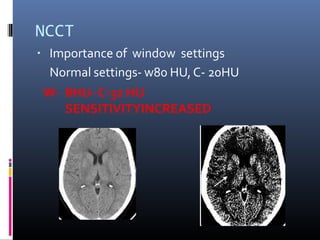
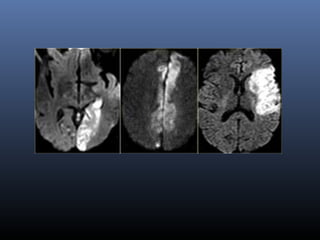
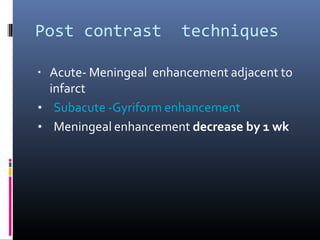
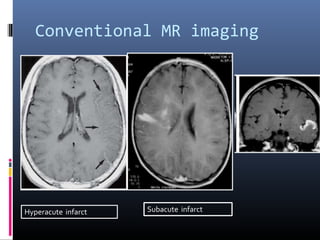
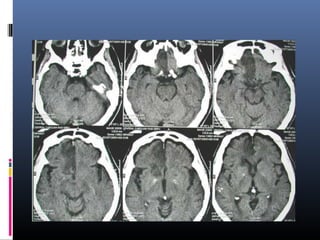
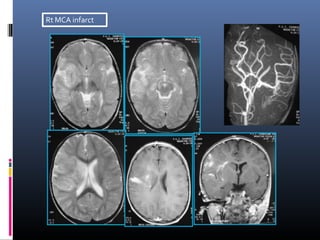
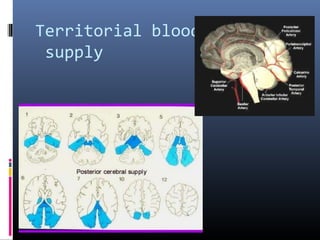
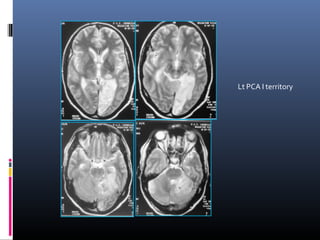
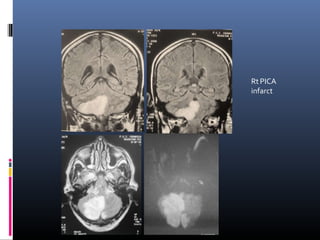
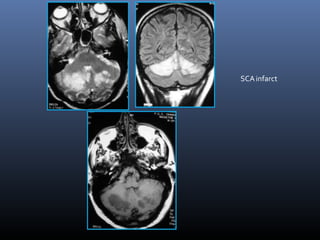
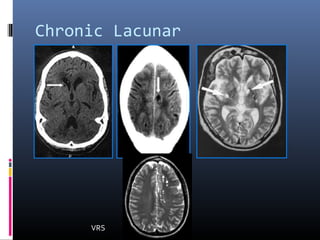
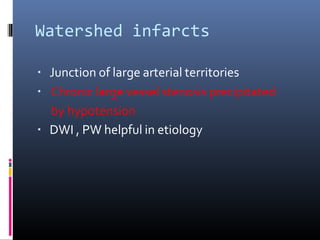
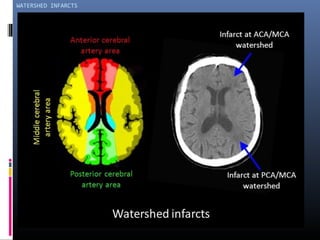
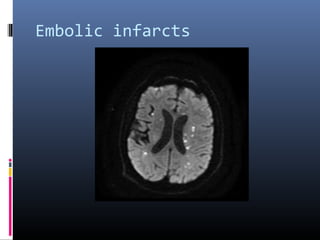
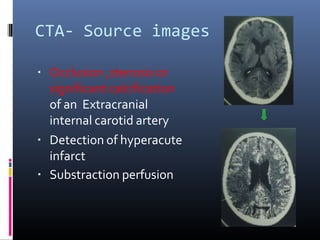
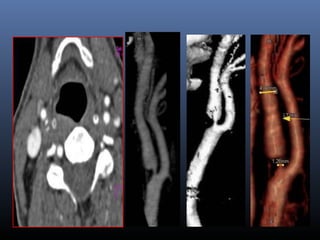
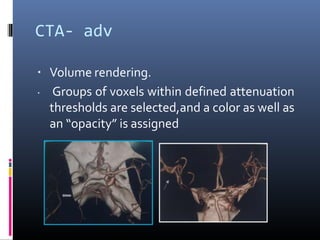
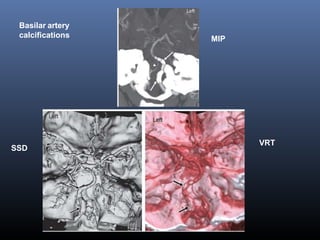
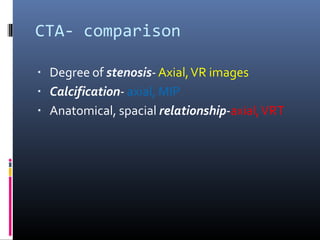
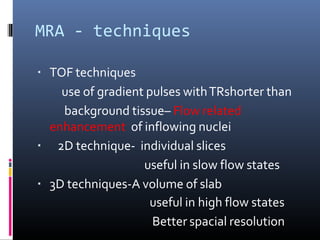
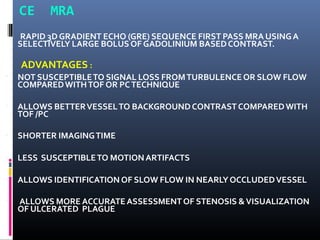
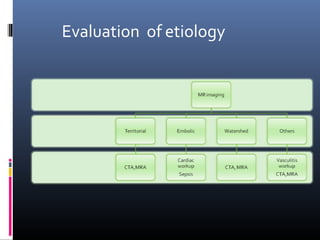
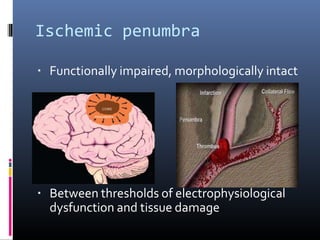
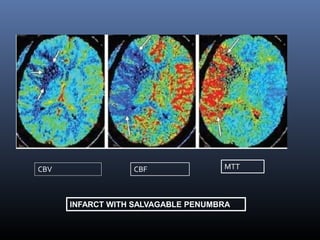
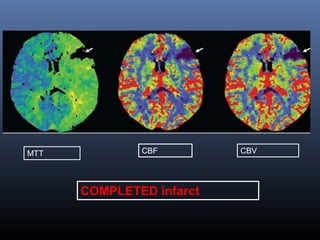
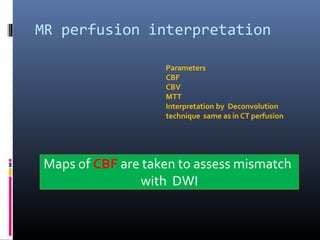
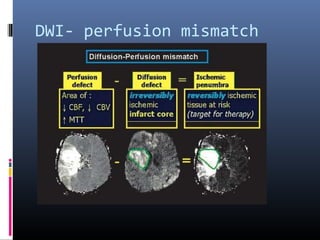
1. The role of various imaging modalities like non-contrast CT (NCCT), MRI, CTA, MRA, CT perfusion, and MRI perfusion in evaluating ischemic stroke at different time points and identifying areas of ischemia, penumbra, infarct core, and mimics like hemorrhage.
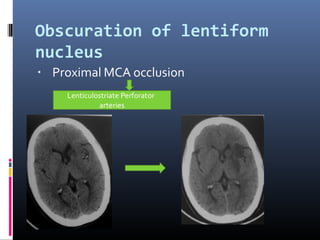
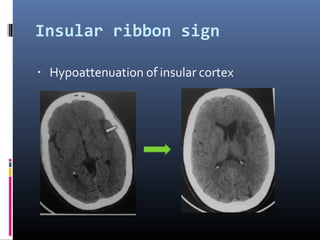
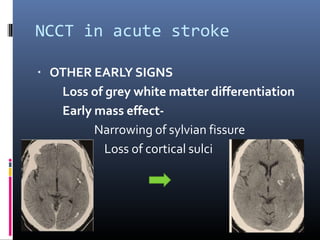
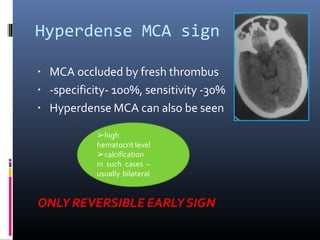
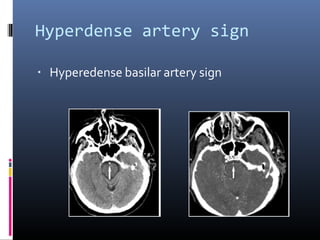
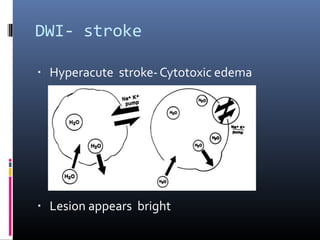
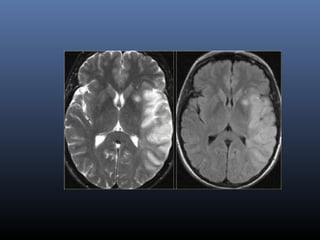
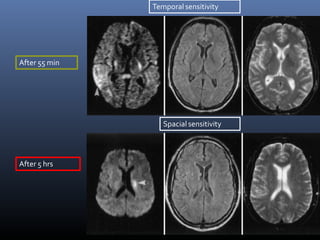
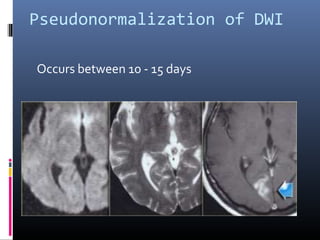
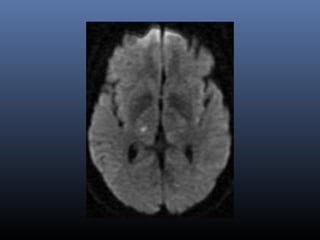
2. Key NCCT findings in acute ischemic stroke include hypoattenuating lesions and hyperdense artery sign. MRI sequences like DWI are very sensitive in detecting acute ischemia.
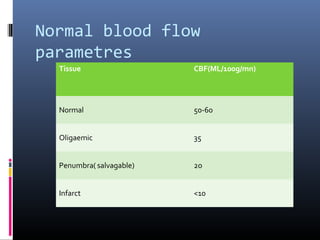
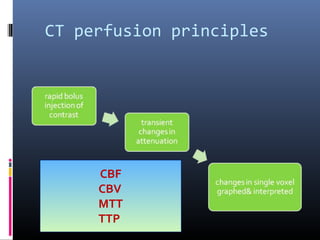
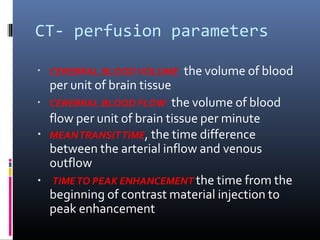
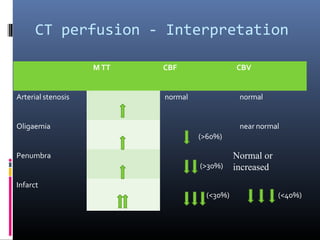
3. CT and MRI perfusion help identify the ischemic penumbra by measuring parameters like cerebral blood flow, volume, mean transit time which