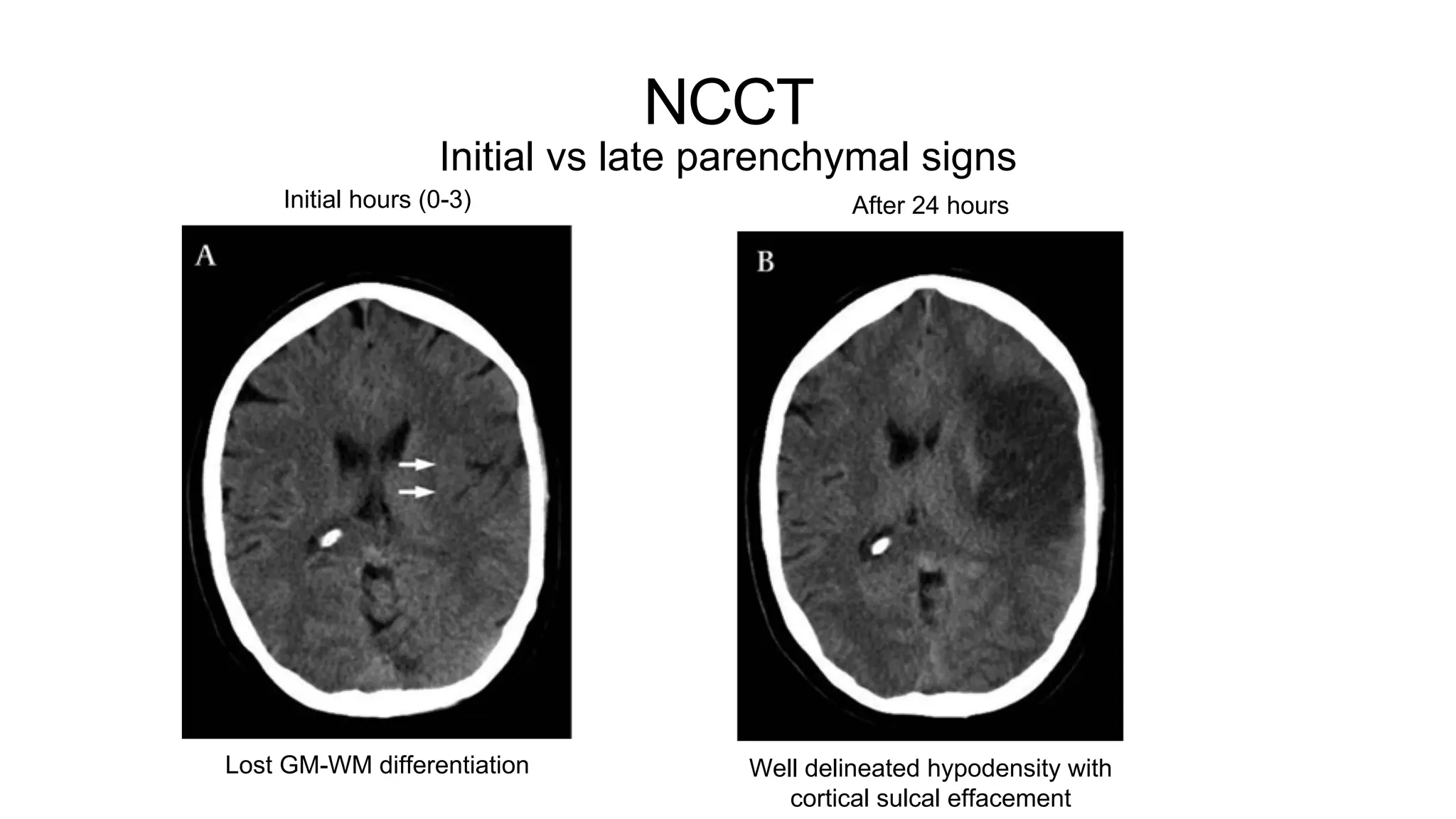
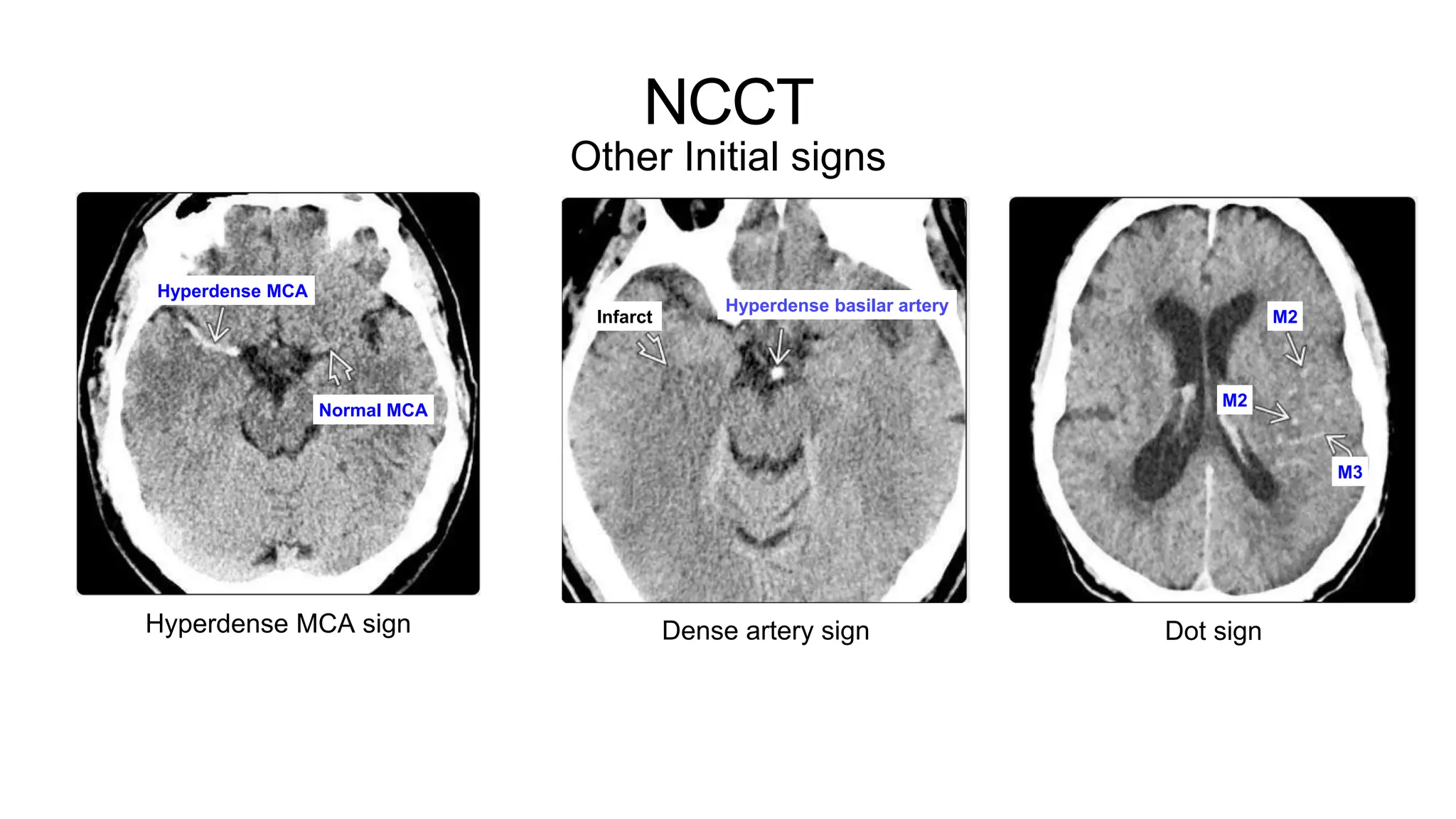
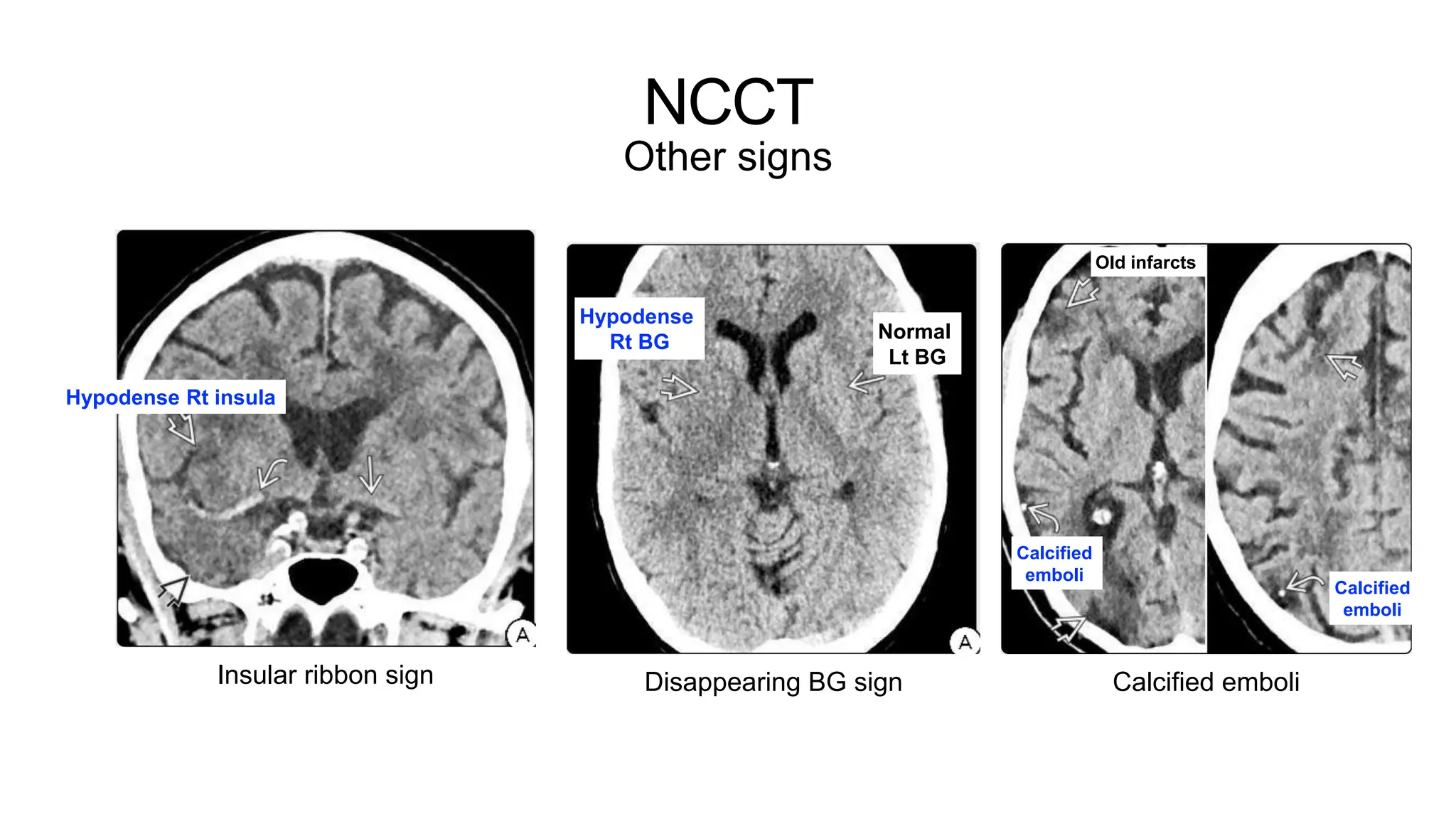
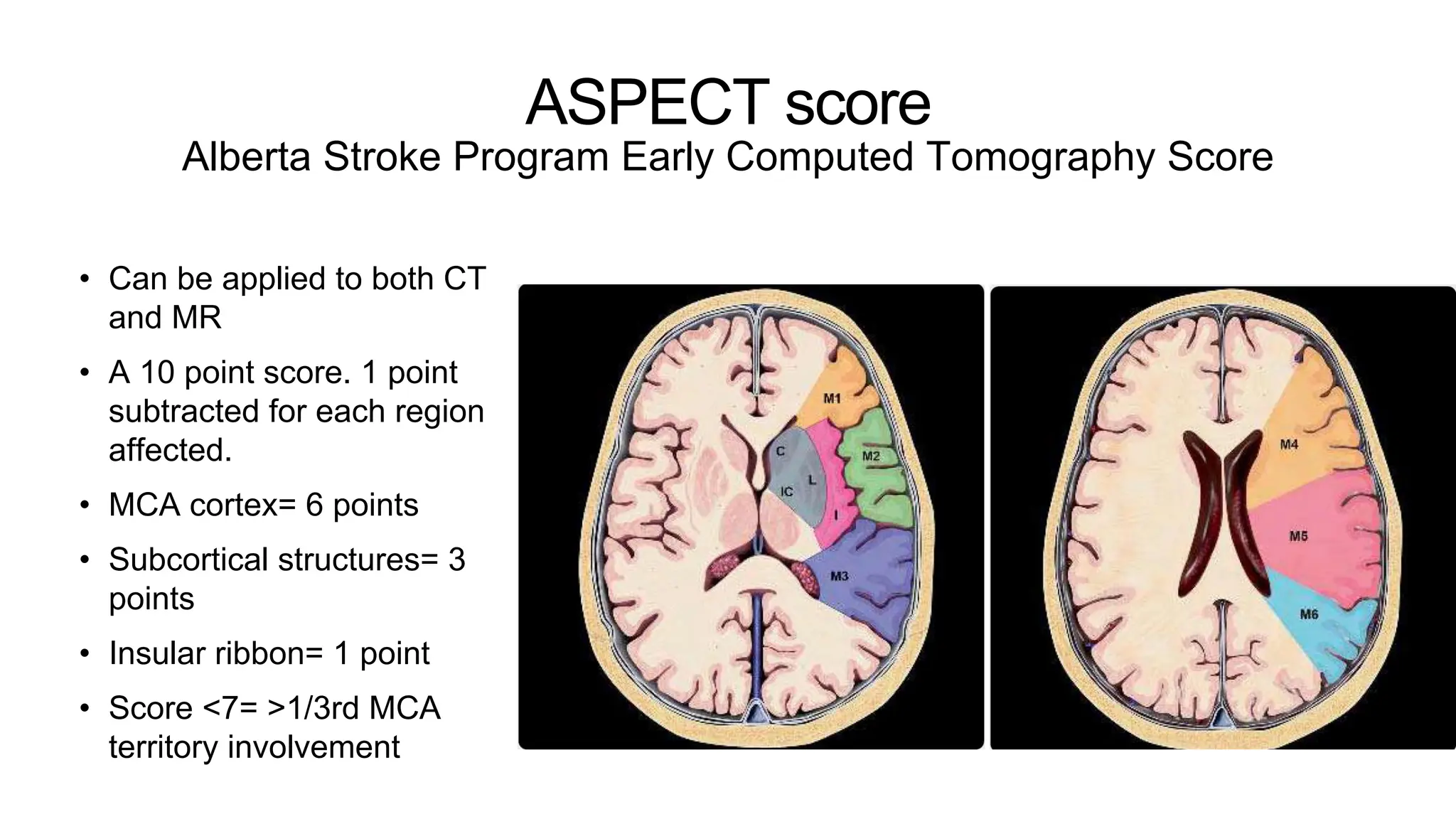
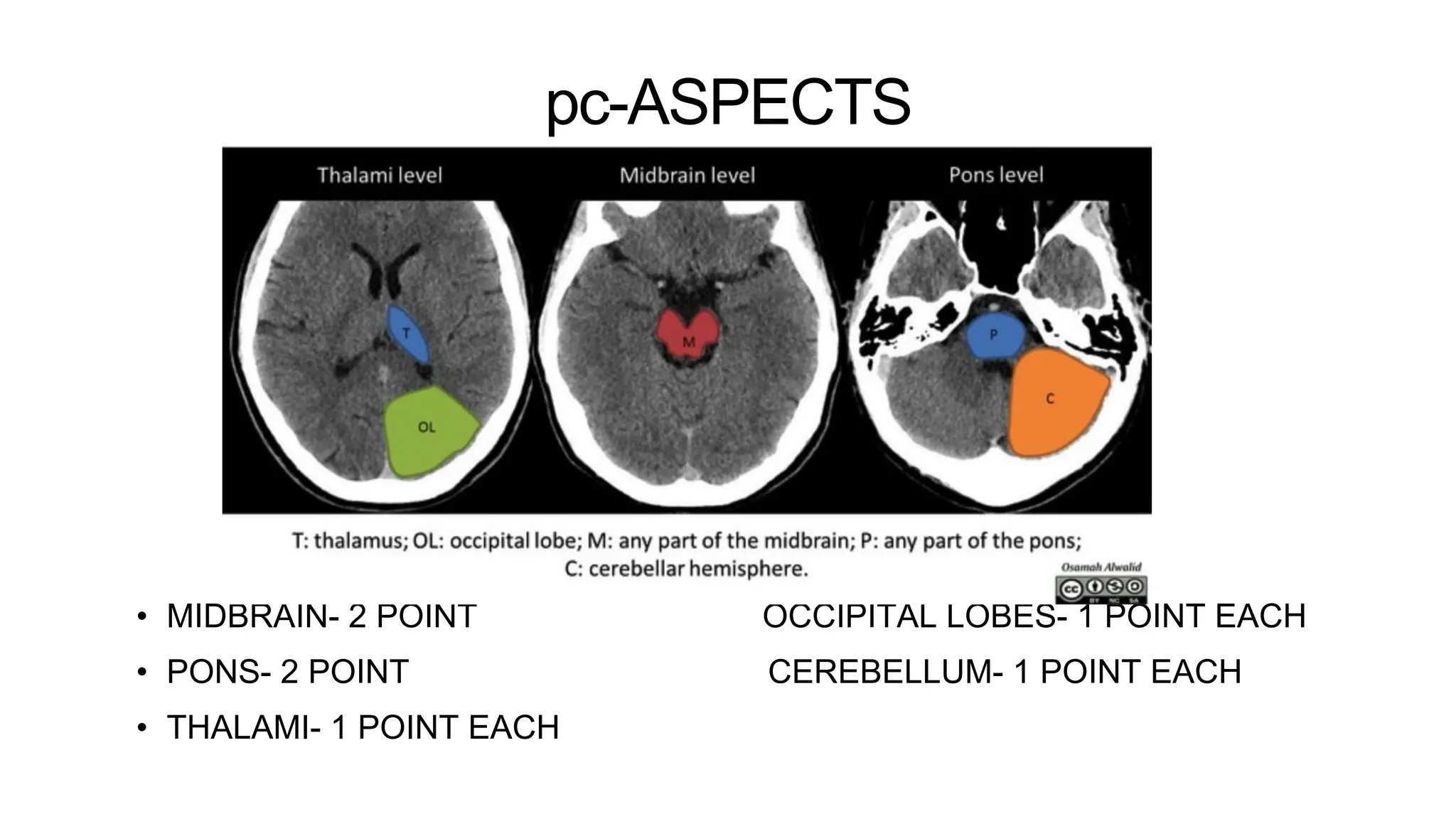
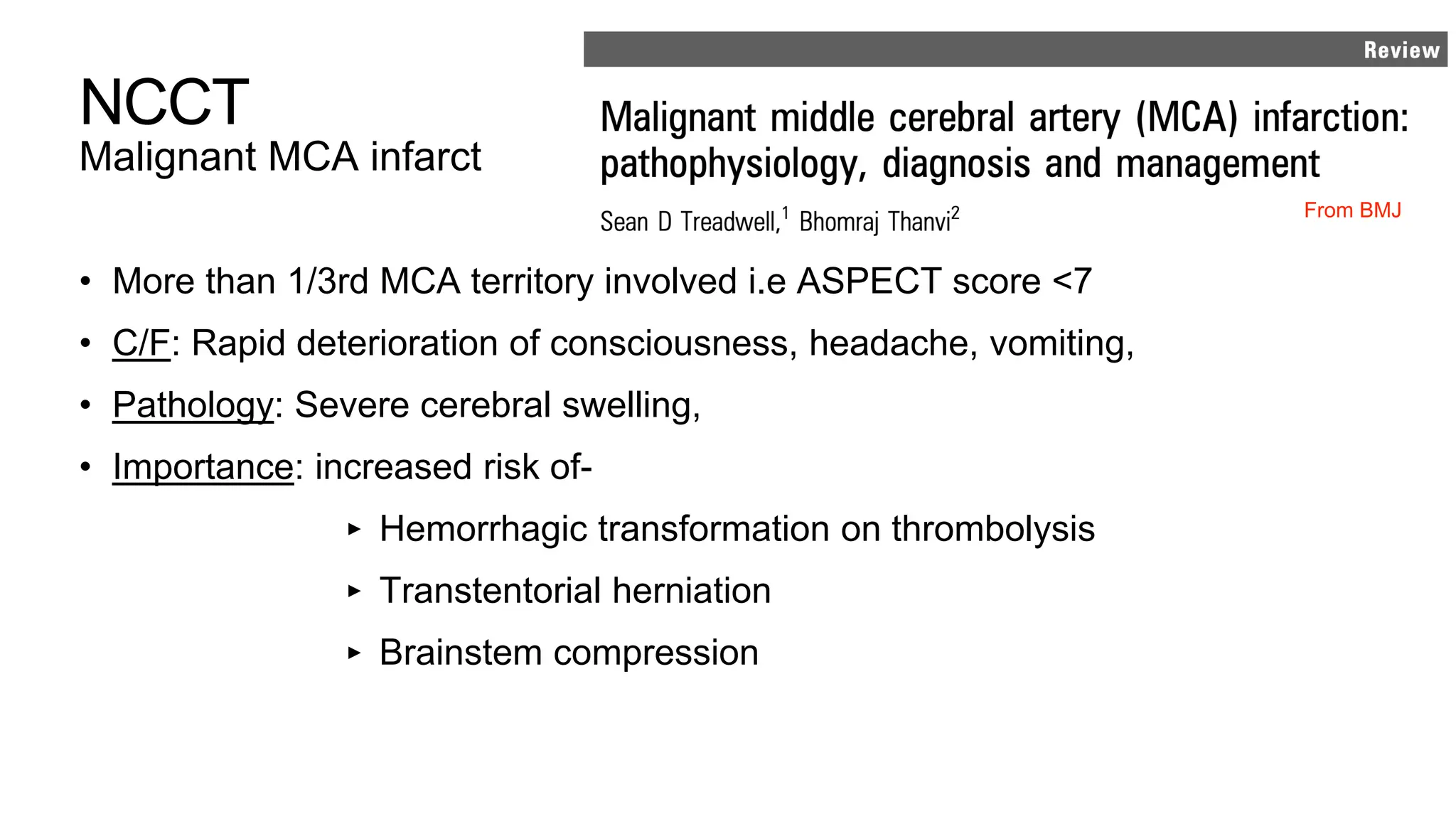
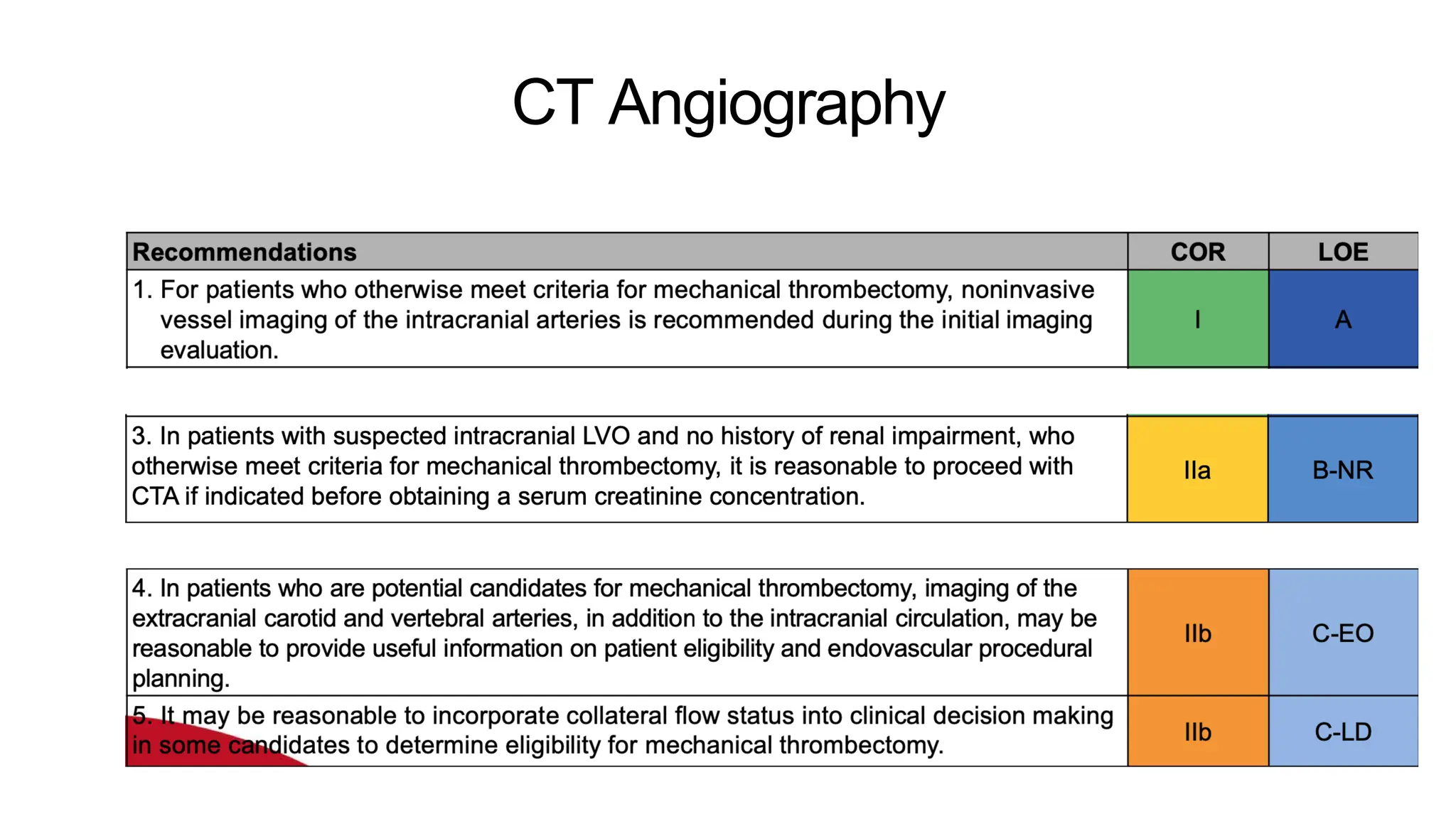
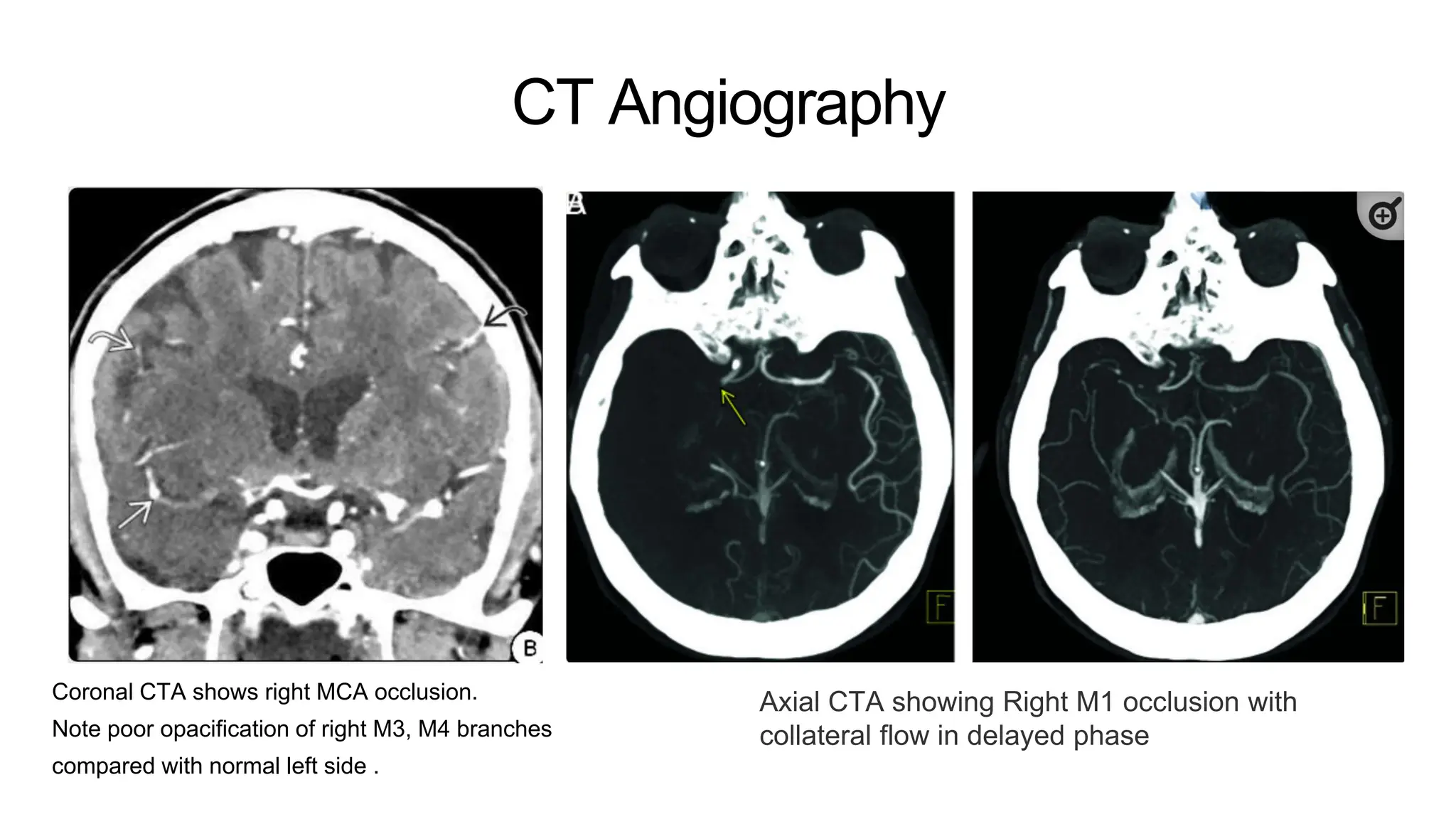
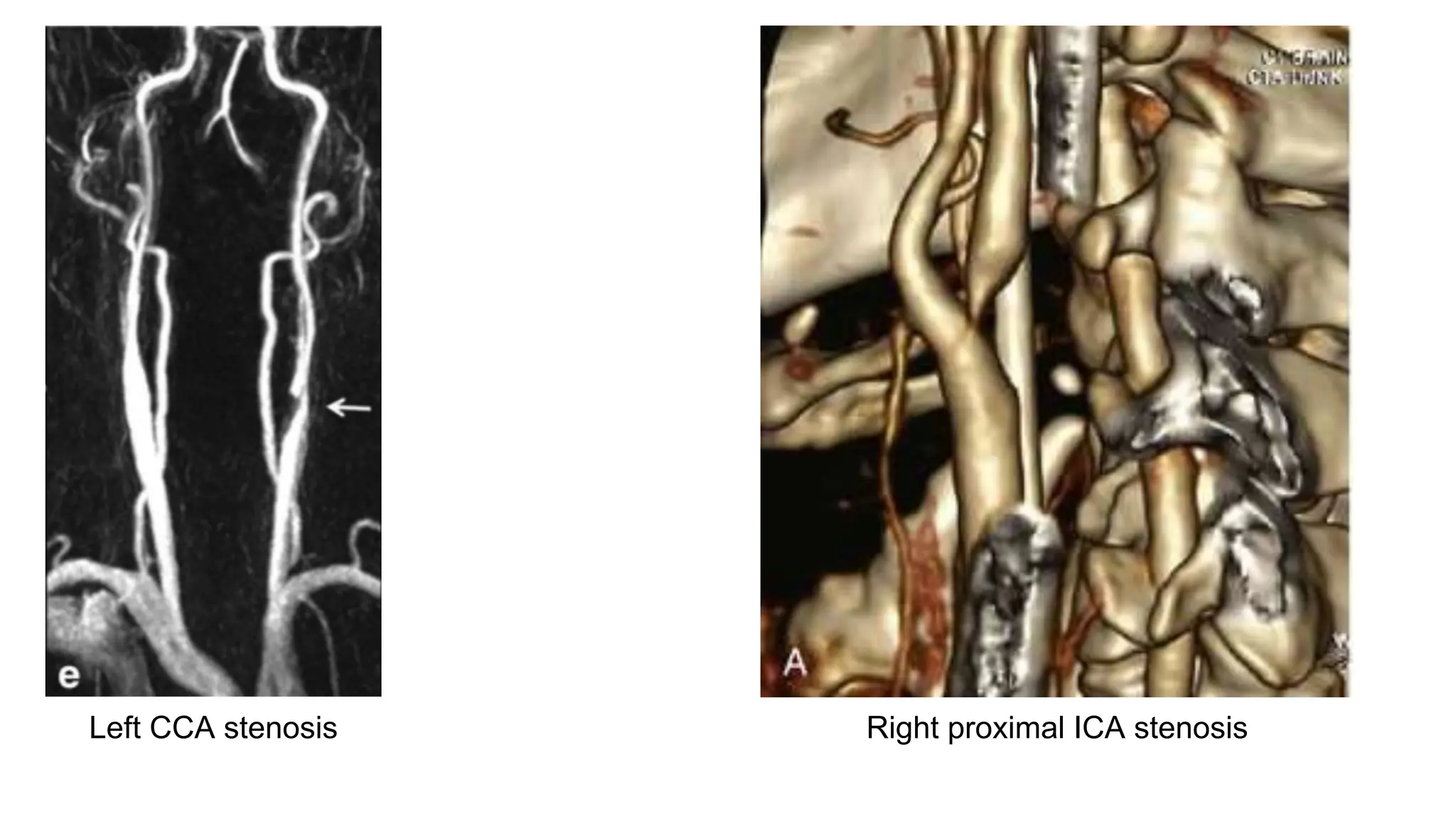
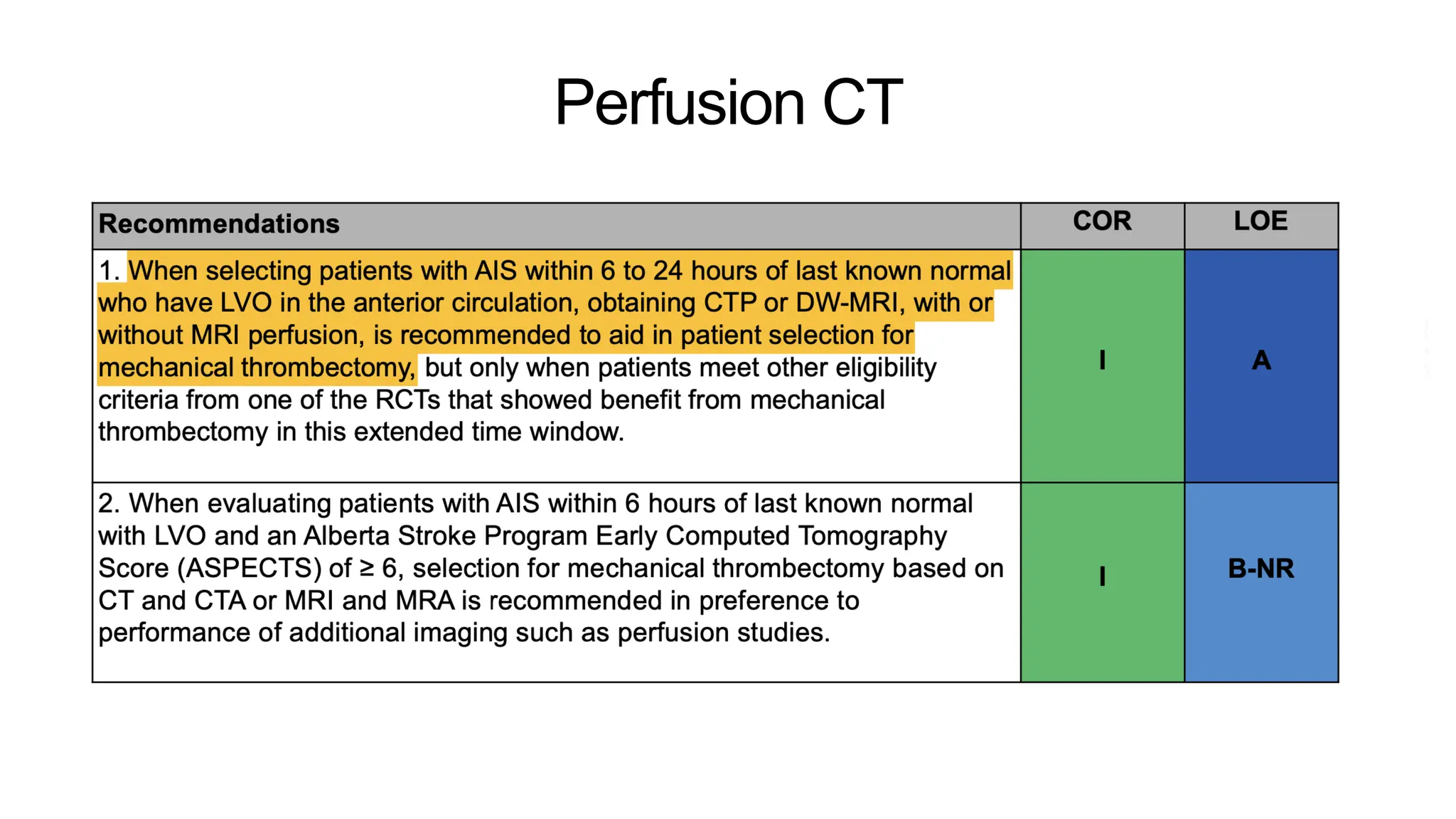
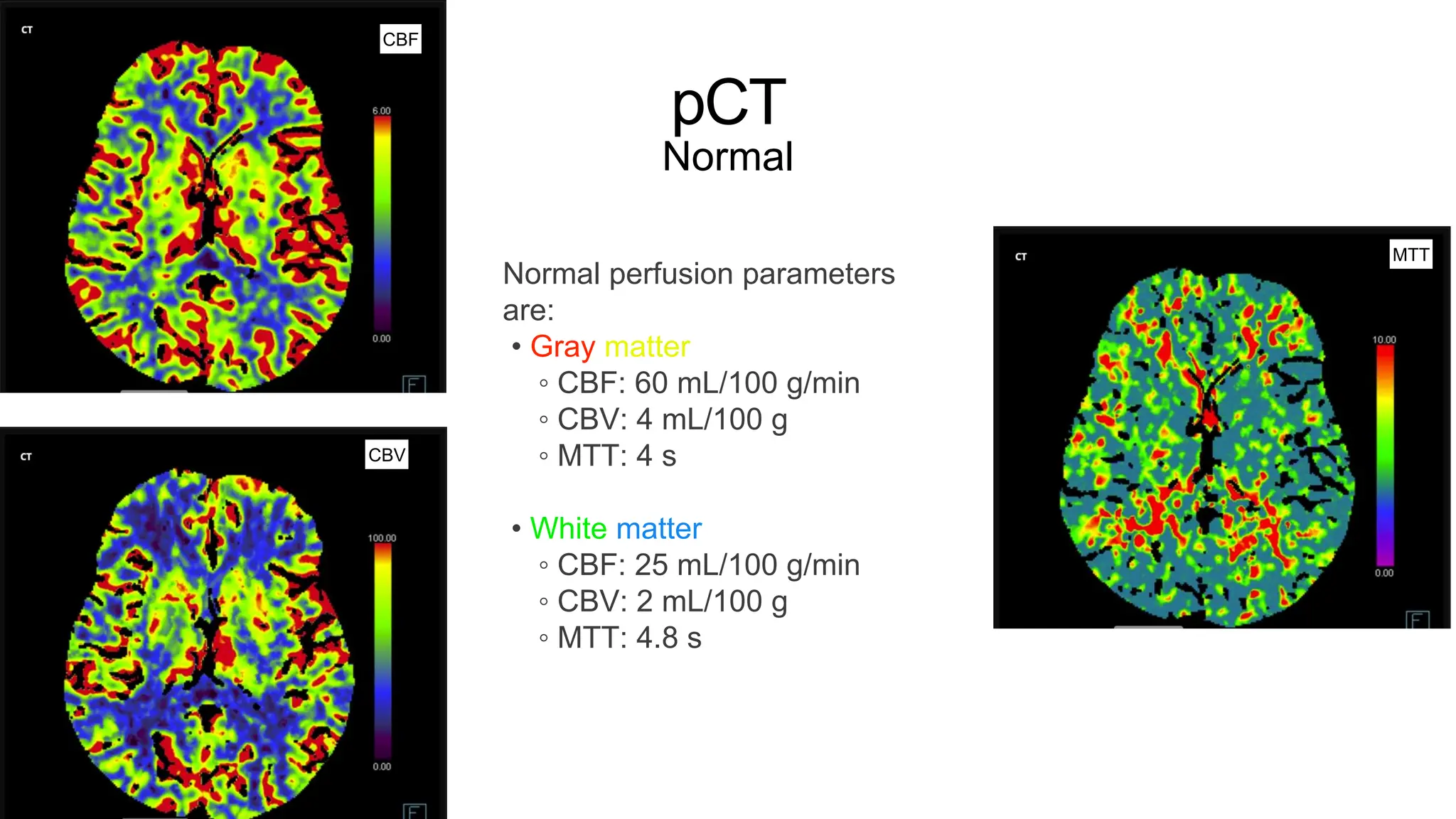
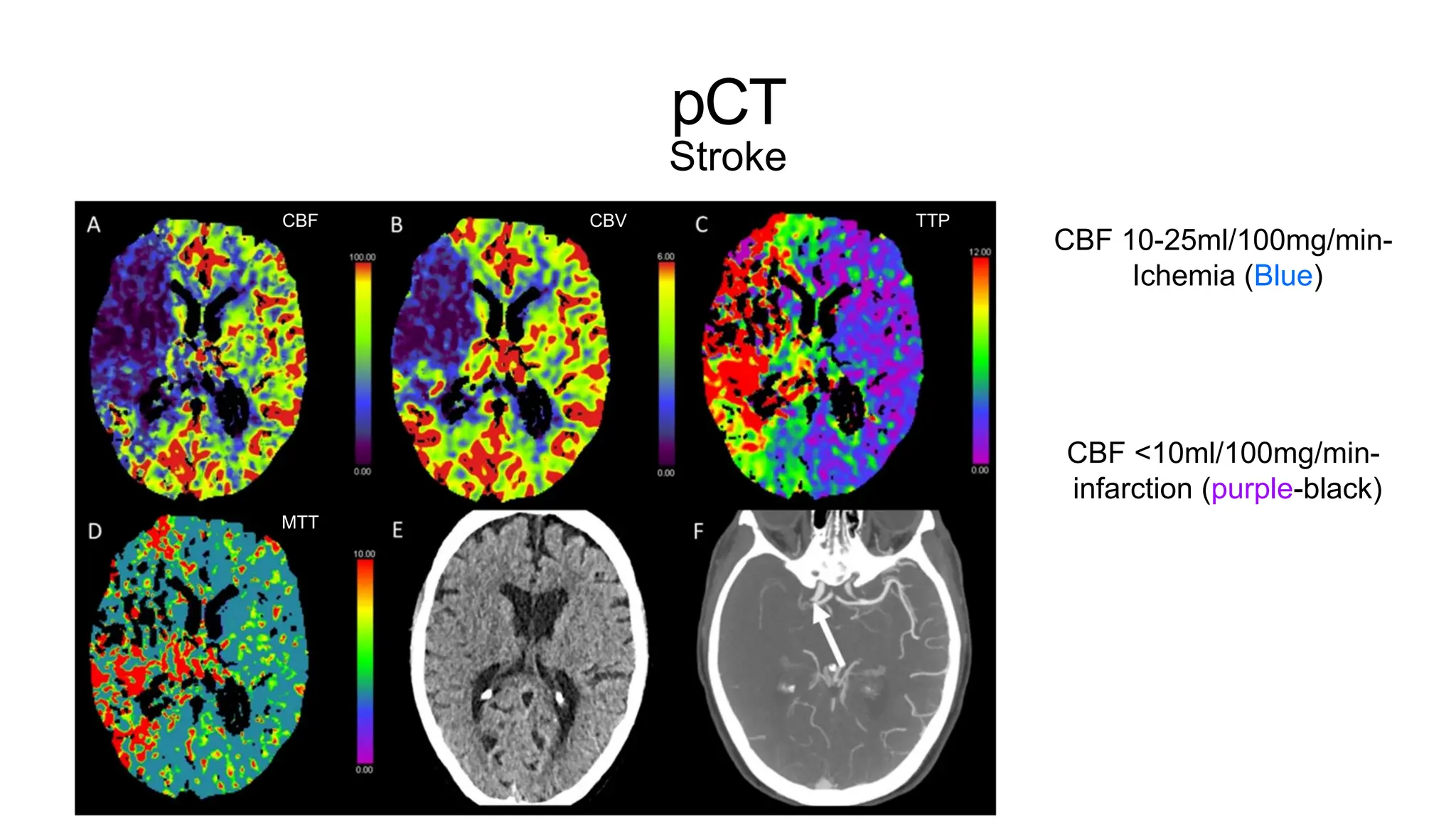
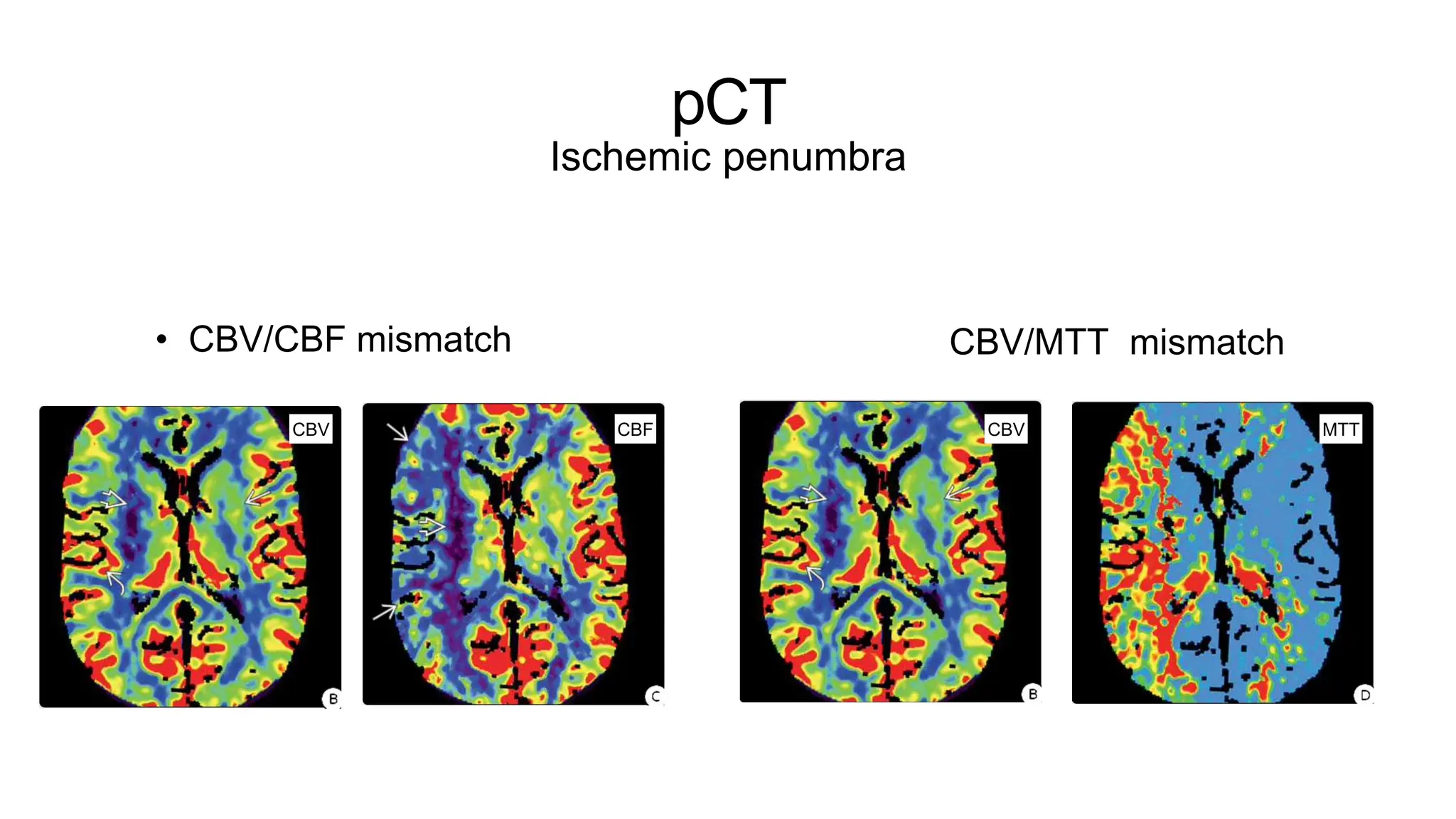
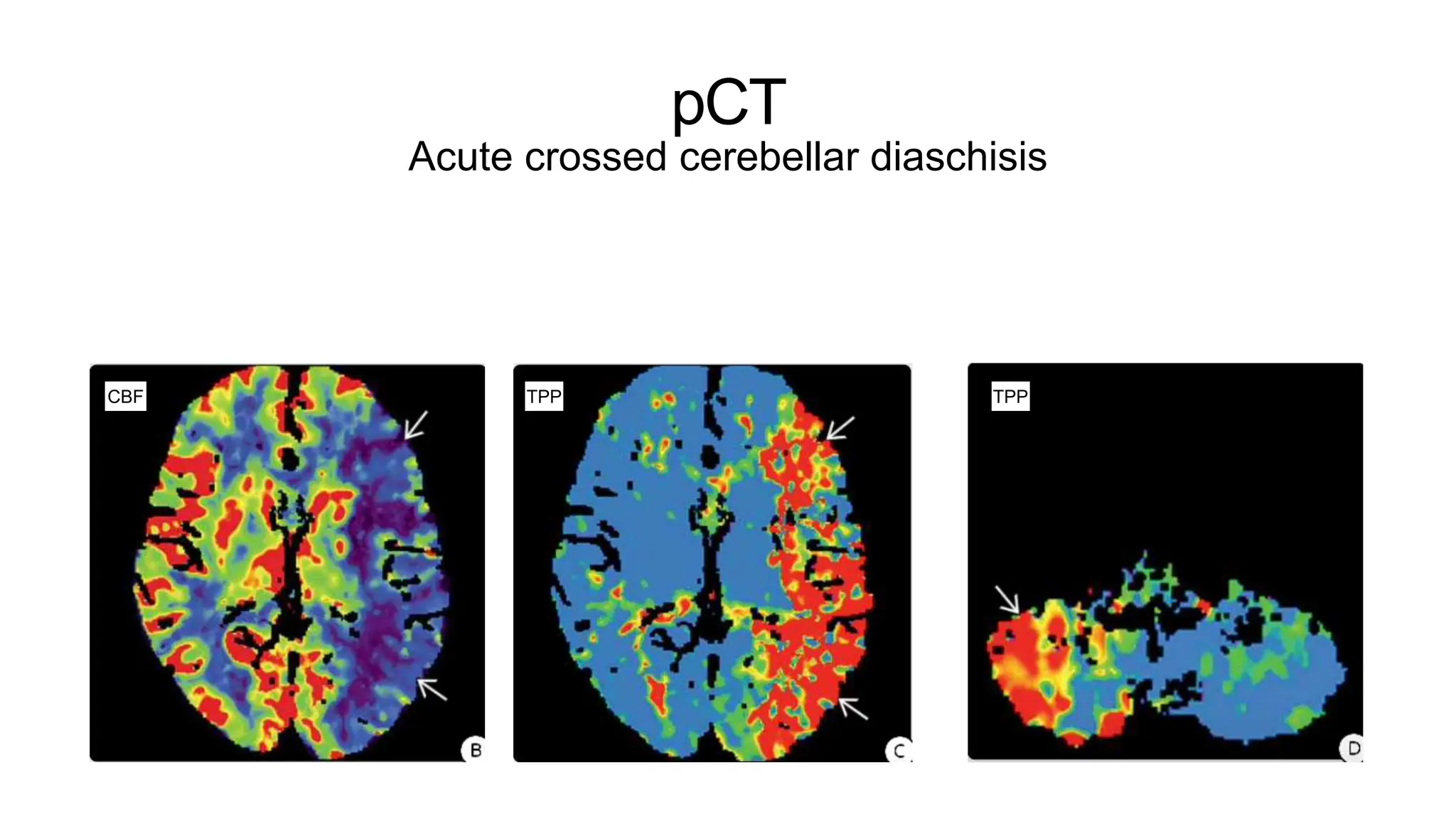
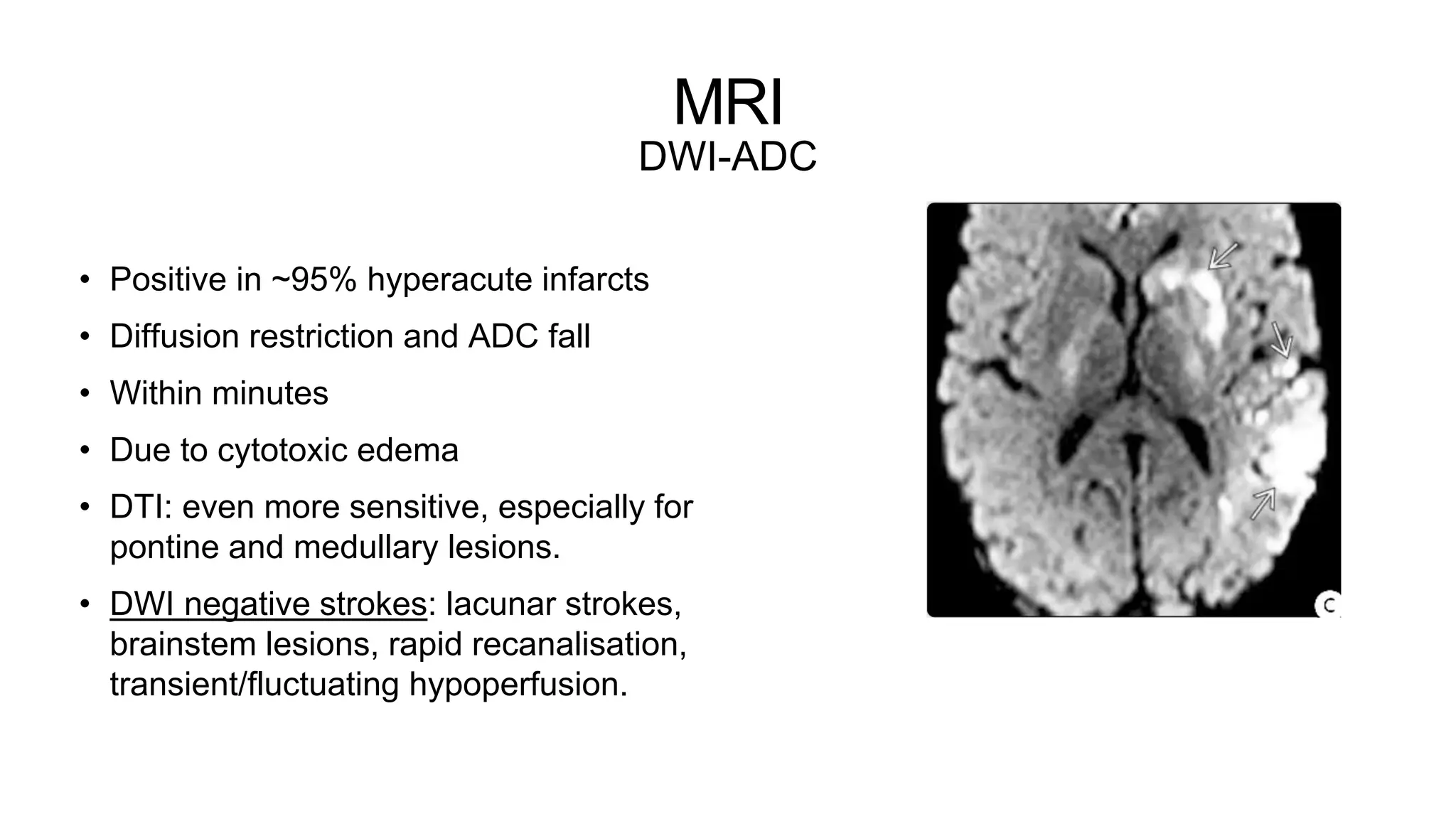
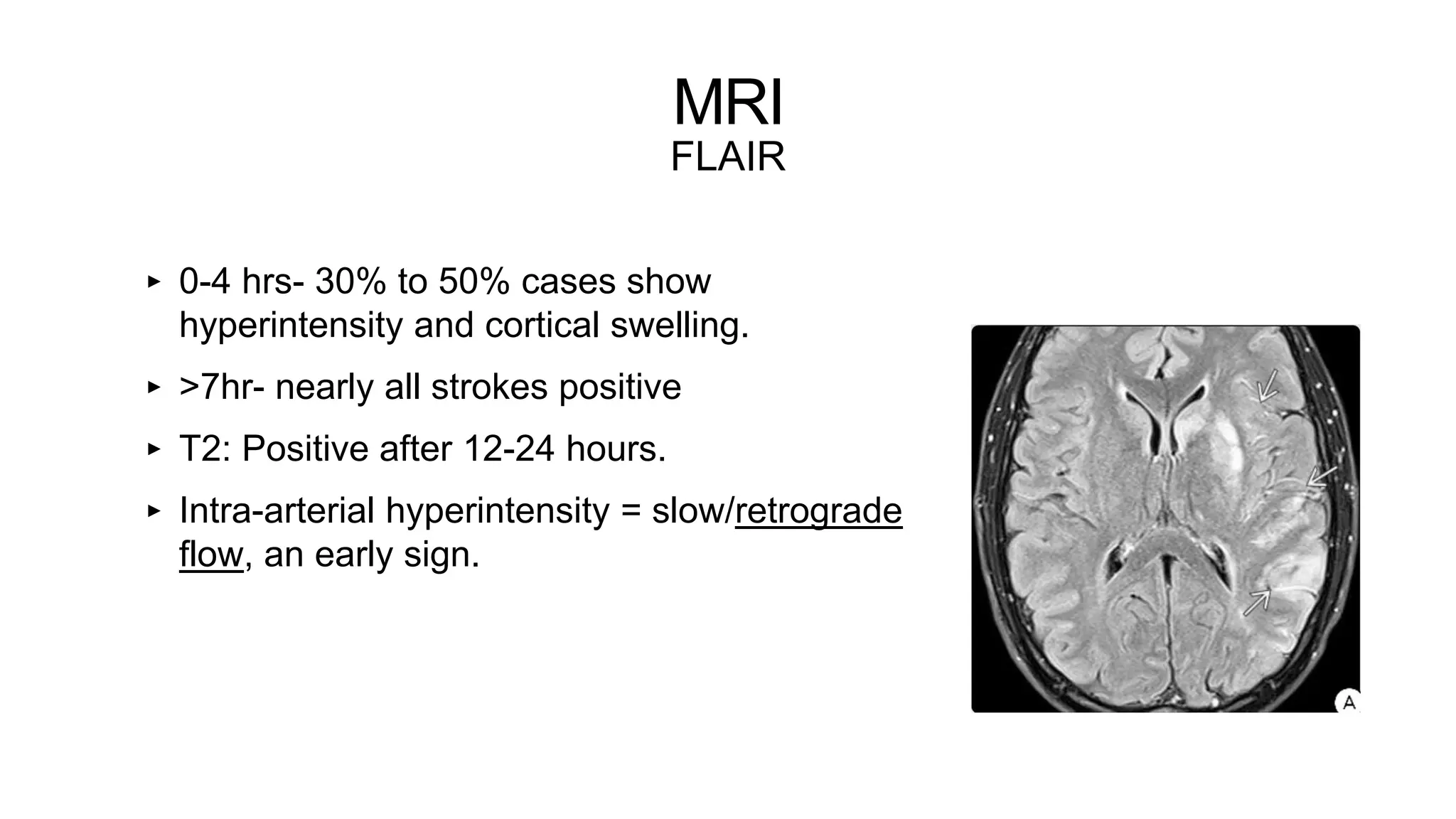
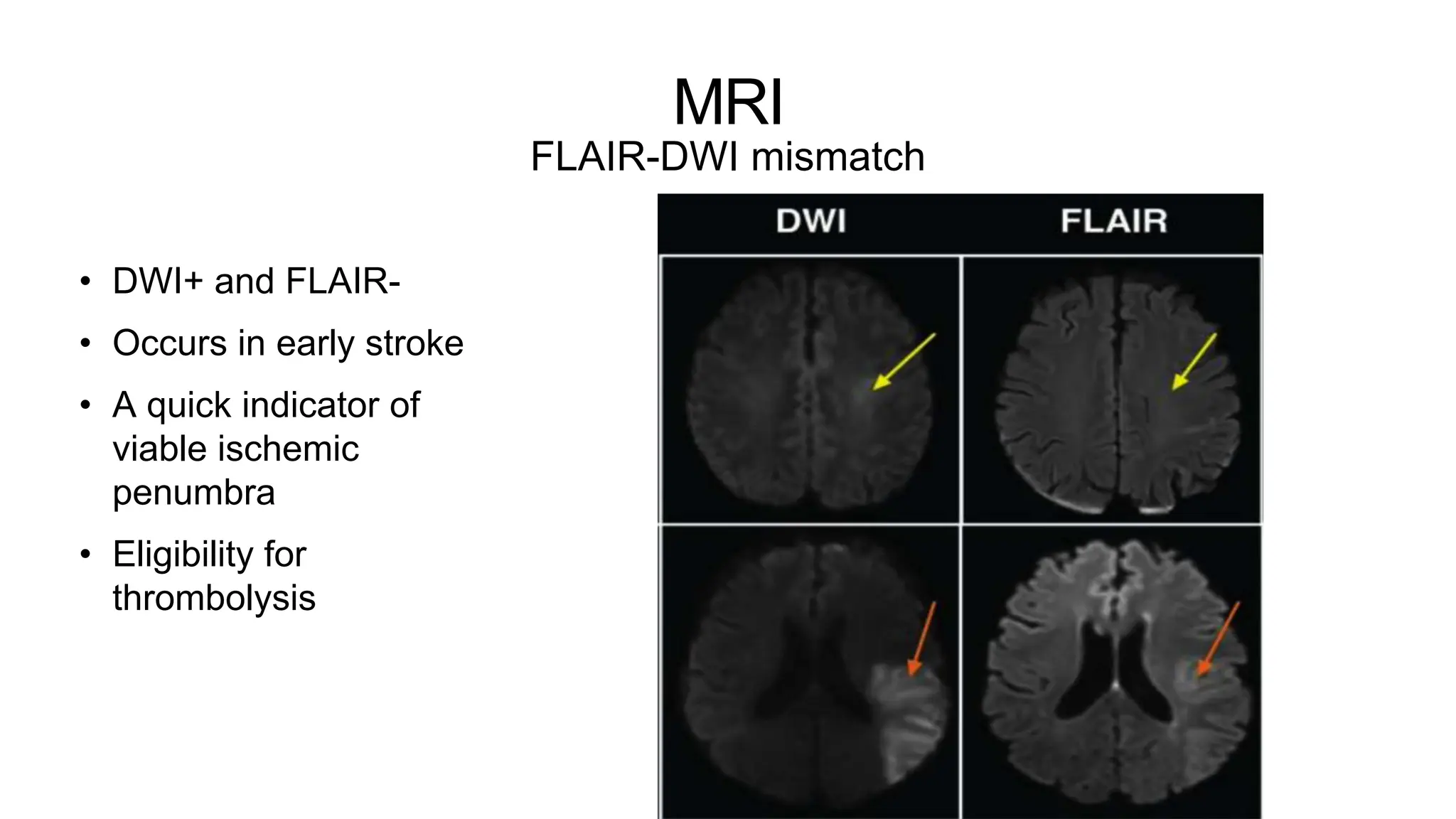
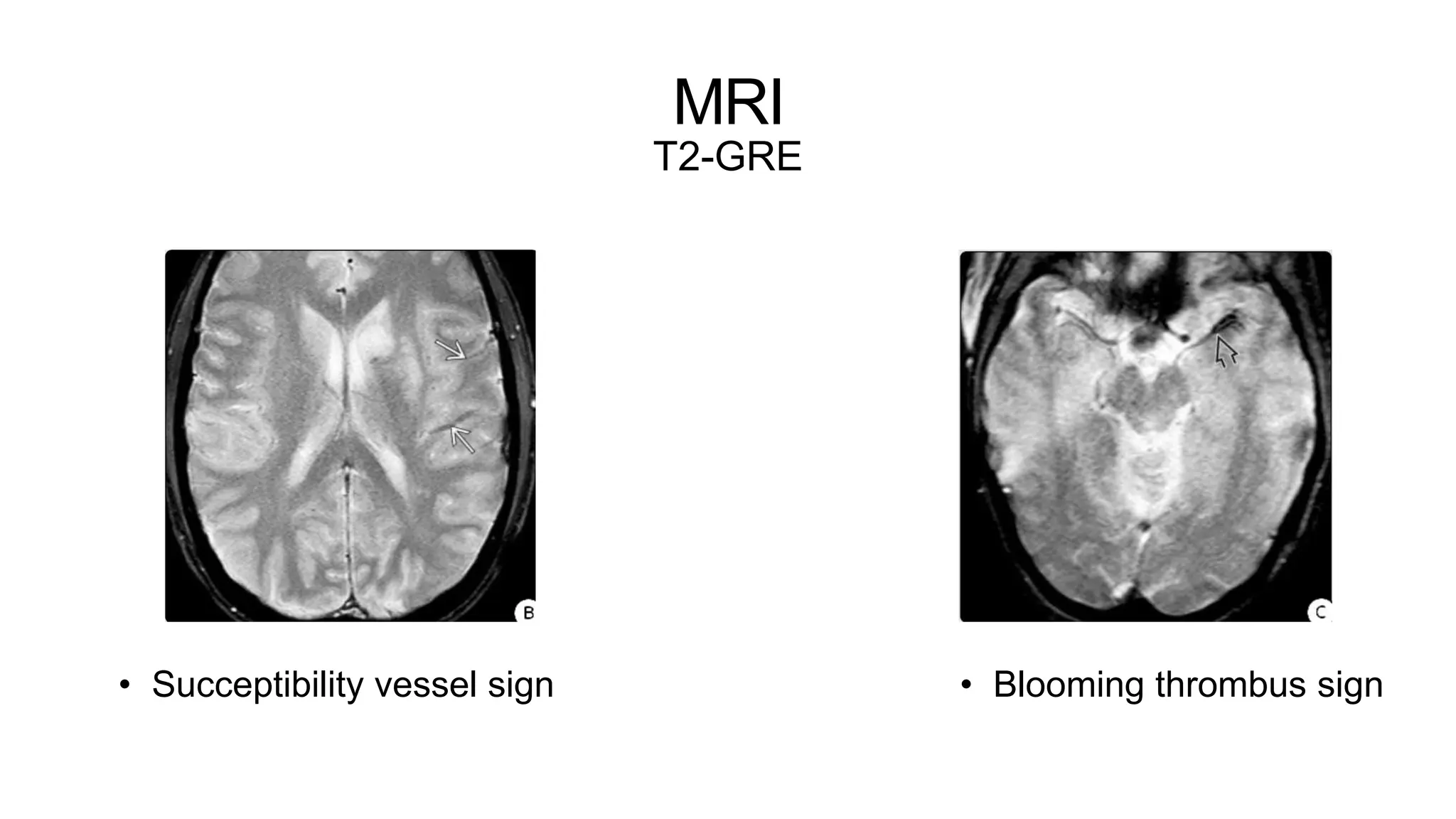
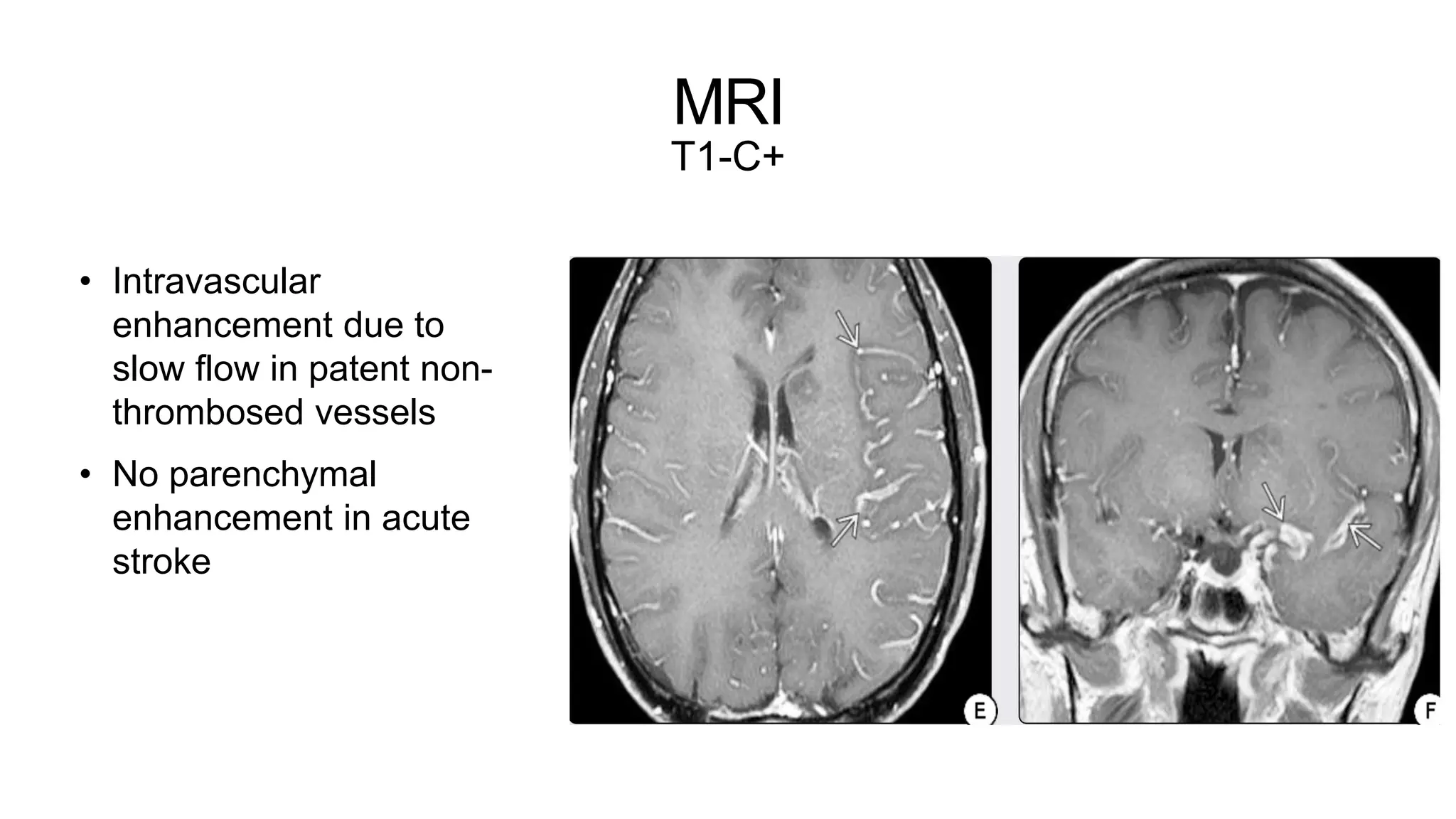
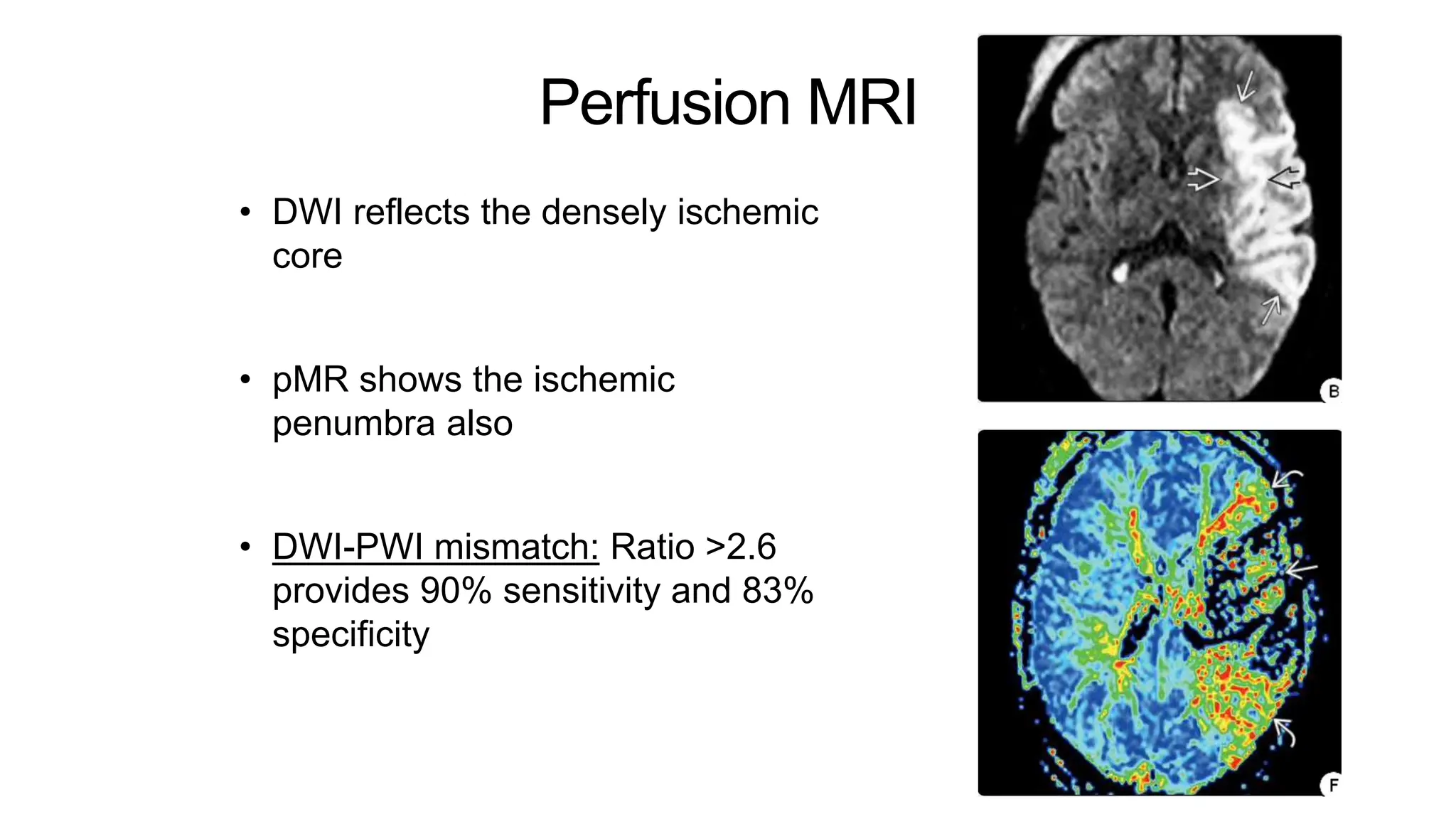
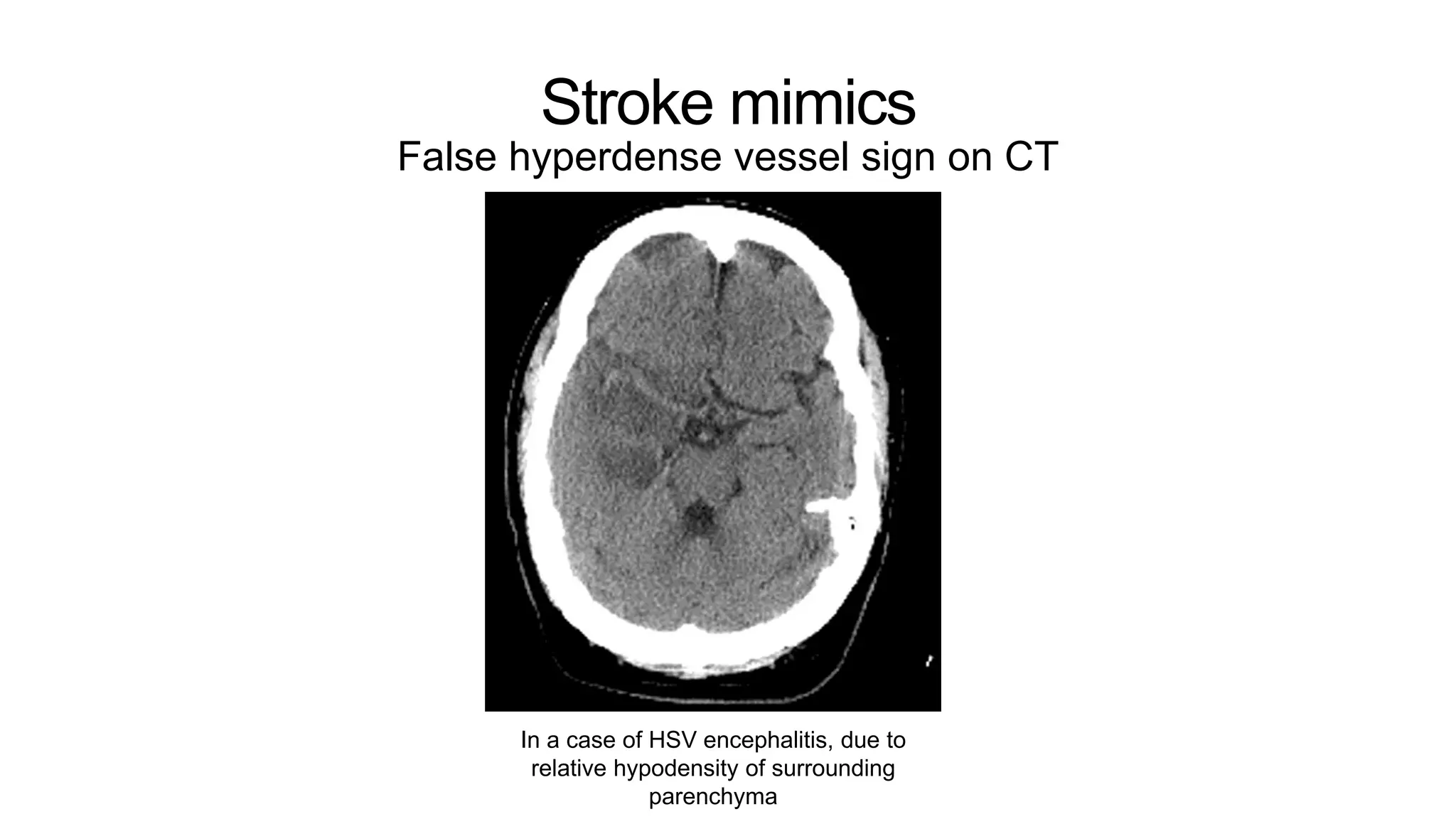
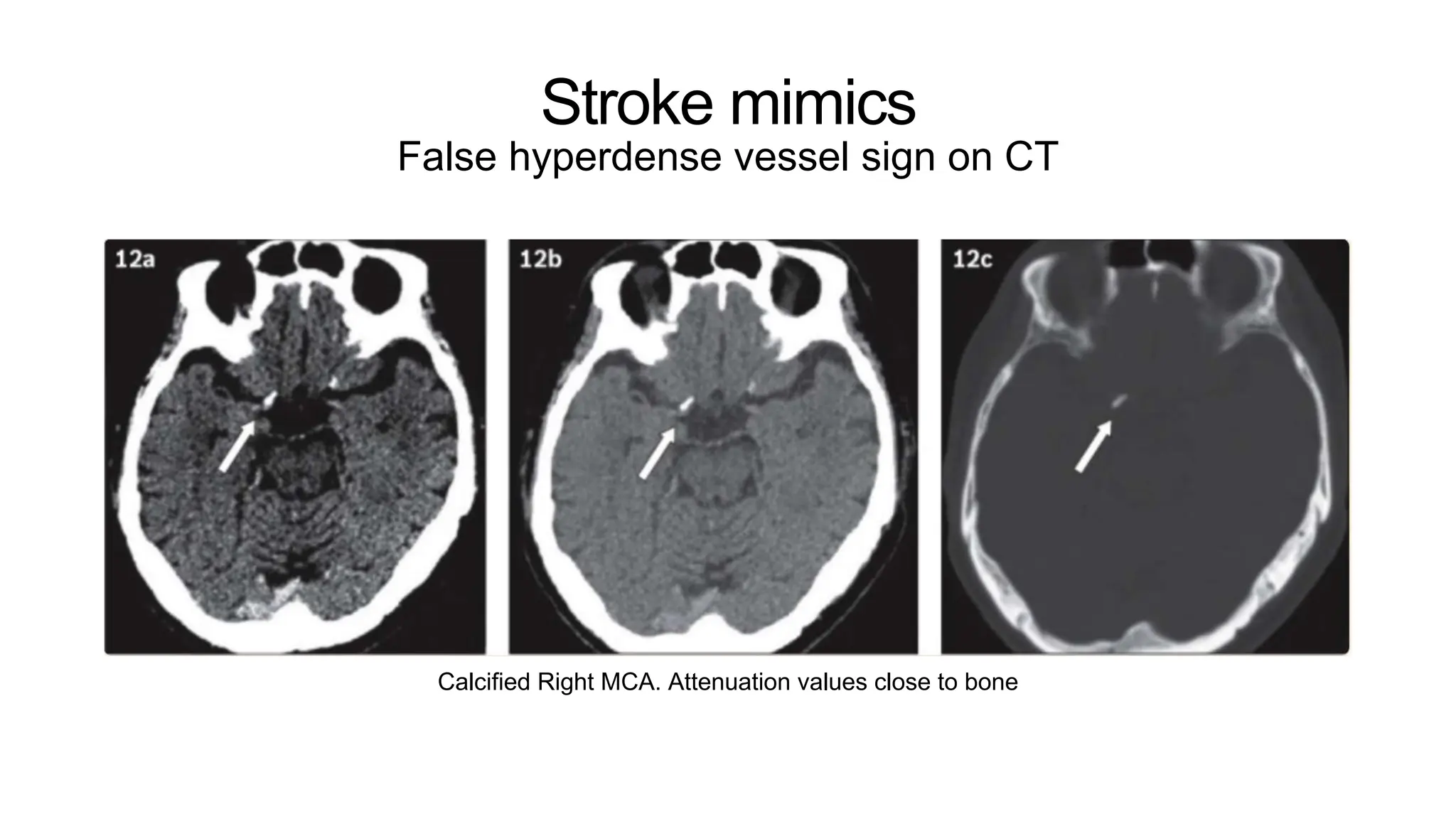
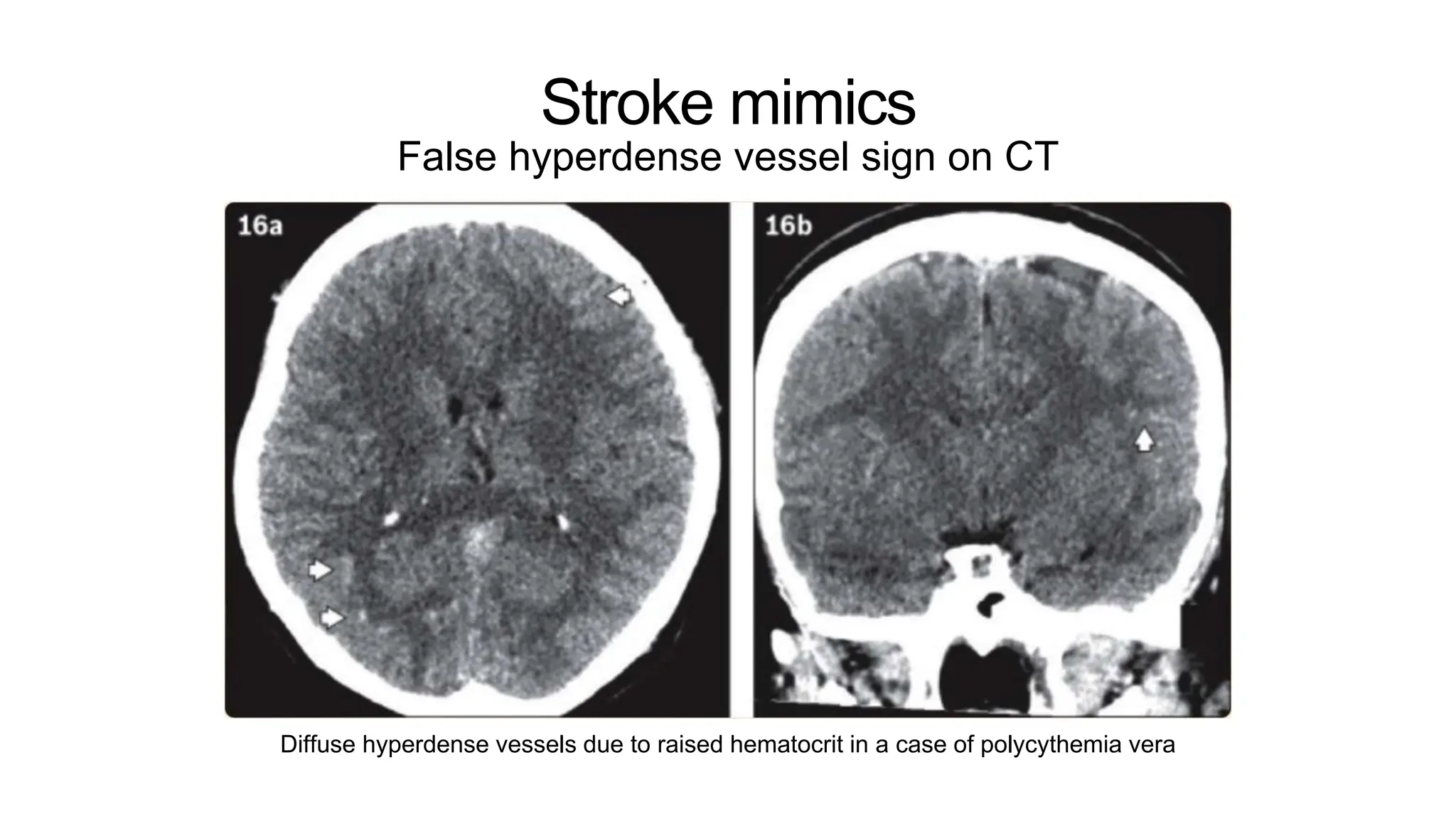
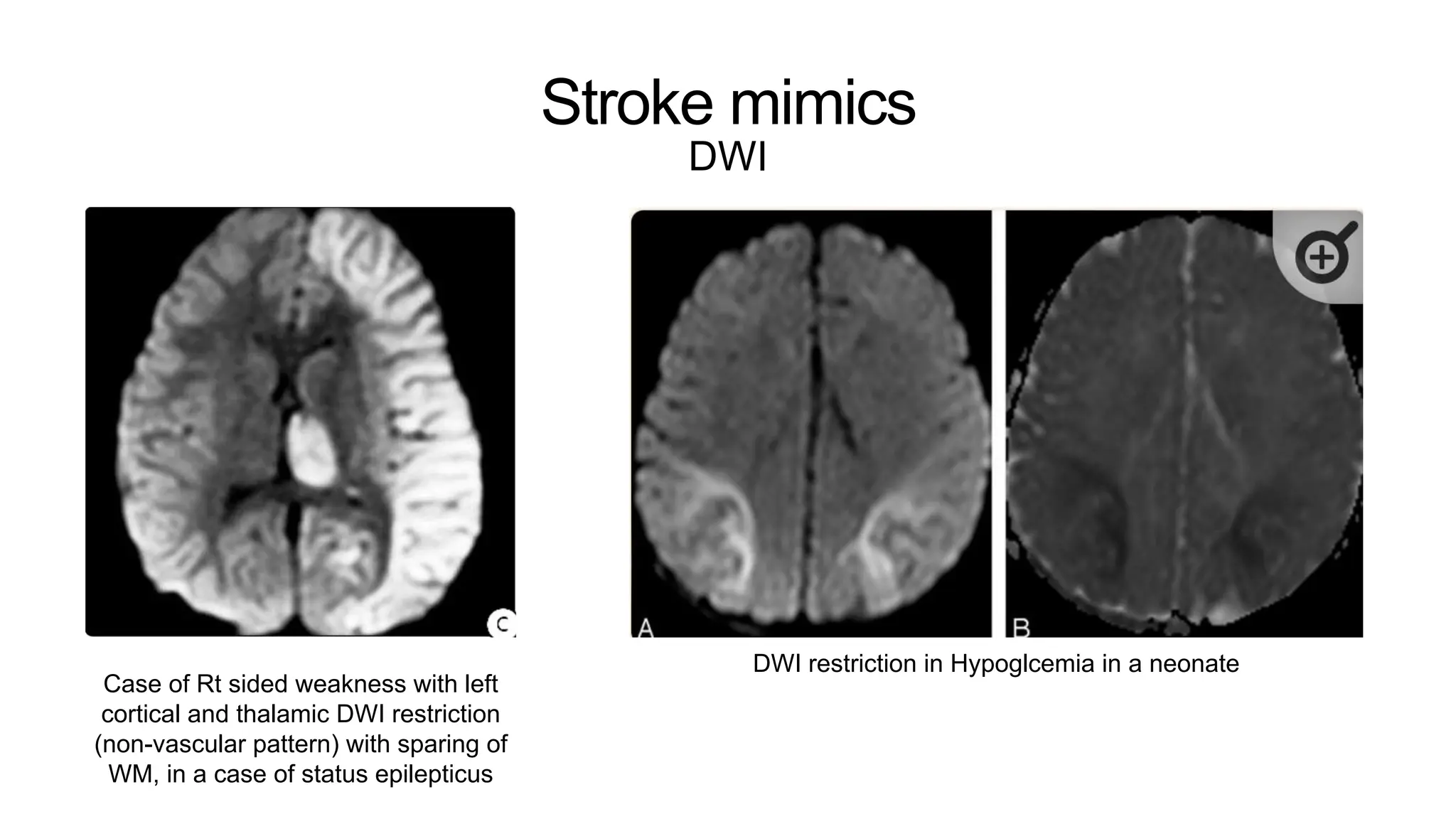
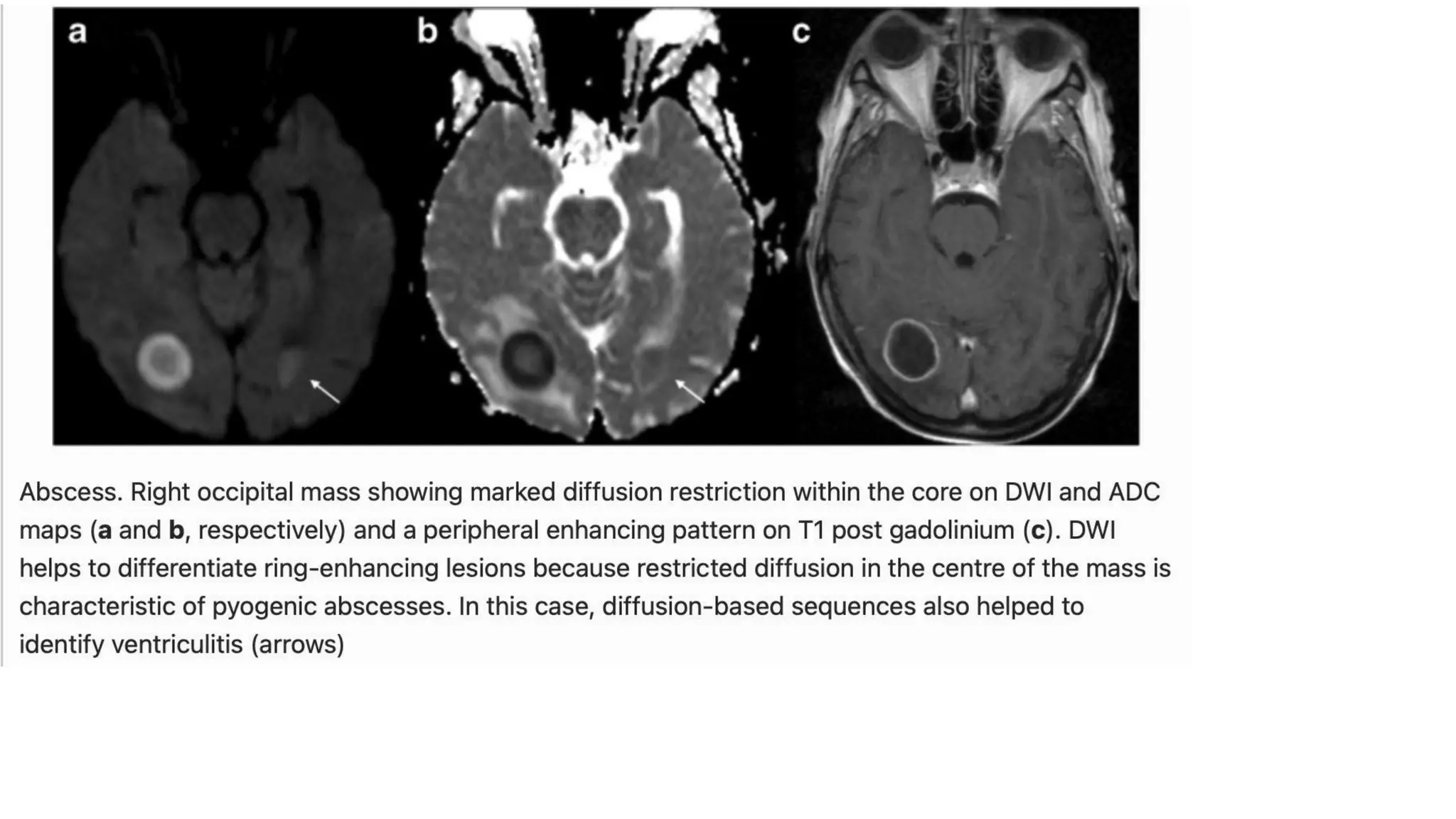
The document outlines key aspects of acute stroke diagnosis using imaging techniques, emphasizing the importance of a multimodal CT protocol which includes NCCT, CT angiography, and perfusion CT. It discusses the Alberta Stroke Program Early CT Score (ASPECTS) for assessing infarct volume and highlights critical signs indicating malignancy in MCA infarctions. Additionally, it compares the efficacy of MRI in detecting strokes, especially in differentiating between ischemic penumbra and core infarcts.