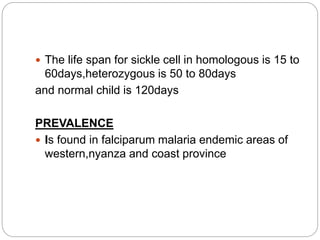
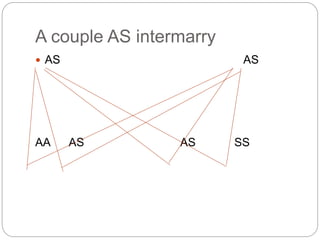
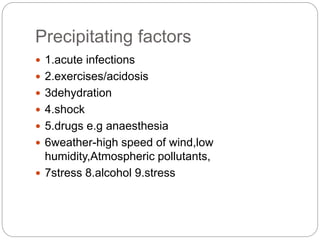
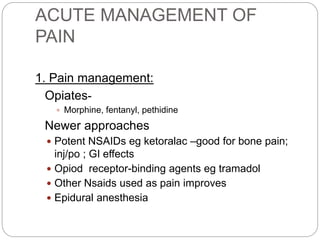
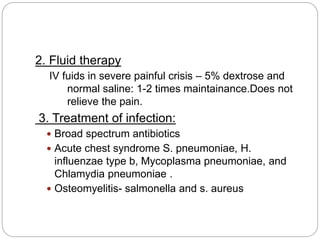
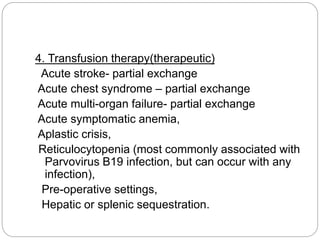
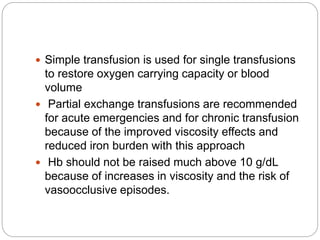
Sickle cell disease is a hereditary blood disorder caused by a mutation in the beta globin chain of hemoglobin. It results in abnormal sickle-shaped red blood cells that can cause pain, organ damage, and early death. Common complications include painful vaso-occlusive crises, acute chest syndrome, and stroke. Treatment involves pain management, antibiotics for infection, transfusions in emergencies, prophylactic penicillin in children, and hydroxyurea or bone marrow transplant in severe cases.