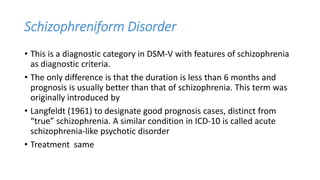
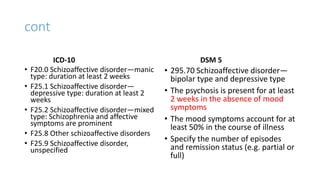
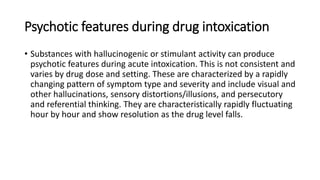
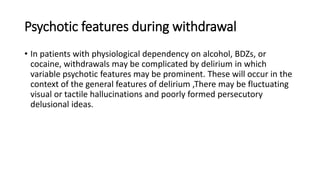
The document discusses various types of psychotic disorders including schizophrenia, schizoaffective disorder, brief psychotic disorder, drug induced psychosis, and reactive psychosis. It provides diagnostic criteria and descriptions for each disorder, including typical presentations, durations, treatments, and prognoses. It also discusses the relationship between substance use and psychosis, distinguishing between intoxication, withdrawal, and genuine comorbidity.