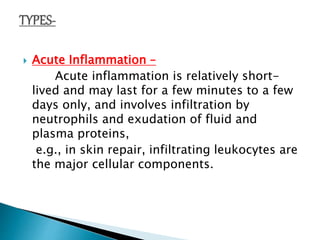
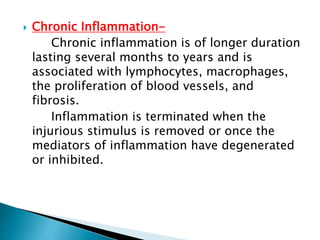
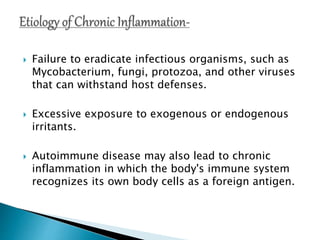
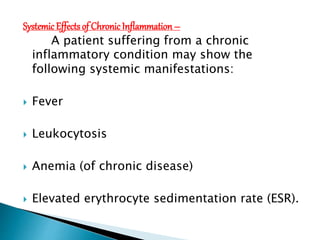
Inflammation can be either acute or chronic. Acute inflammation is short-lived, involving neutrophils and fluid/protein exudation to repair injured tissue. Chronic inflammation lasts months to years, associated with lymphocytes, macrophages, new blood vessel growth and fibrosis. Chronic inflammation occurs when an irritant persists and the acute response cannot resolve it, leading to long-term tissue damage and systemic effects like fever and anemia.