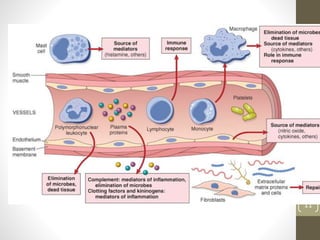
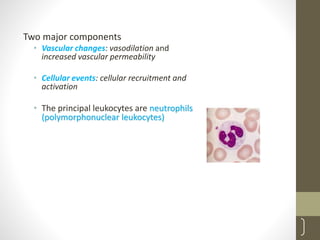
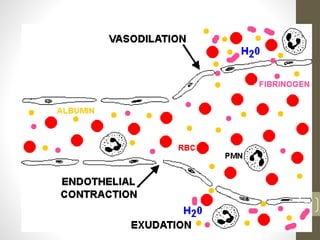
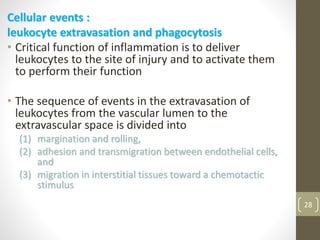
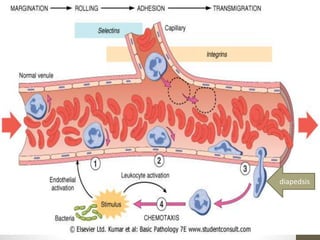
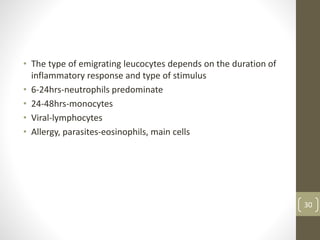
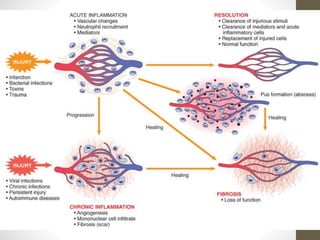
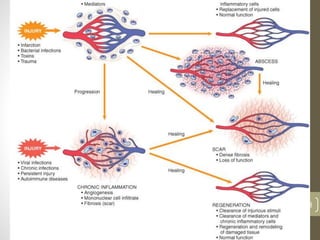
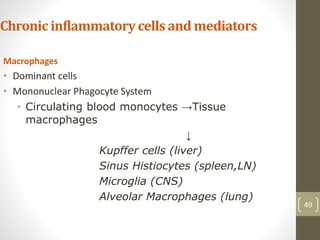
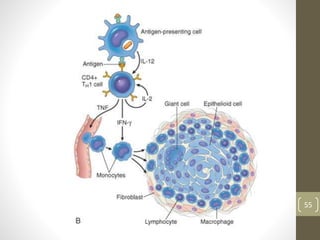
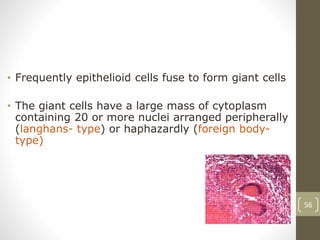
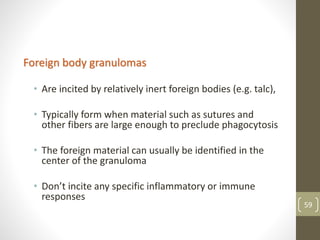
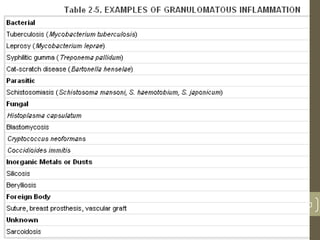
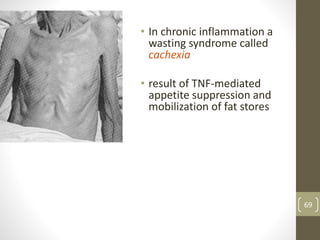
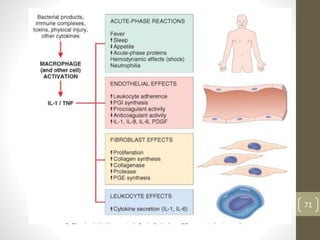
The document discusses the complex process of inflammation, highlighting its roles in protecting the body from injury and infections through vascular and cellular responses. It distinguishes between acute and chronic inflammation, detailing causes, cellular components, and outcomes such as resolution or progression to chronic conditions. Additionally, it outlines systemic effects and signs of inflammation, such as fever and leukocytosis, reinforcing the importance of inflammation in tissue repair and defense mechanisms.