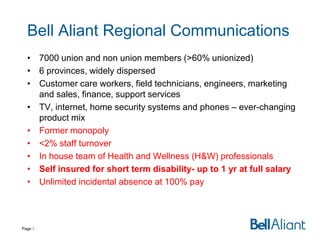
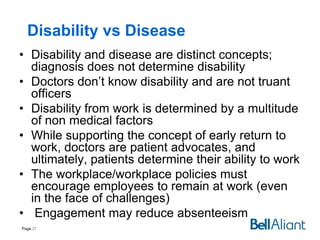
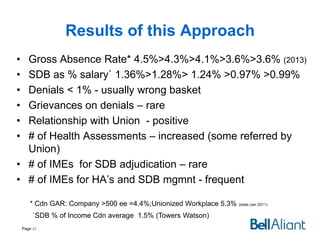
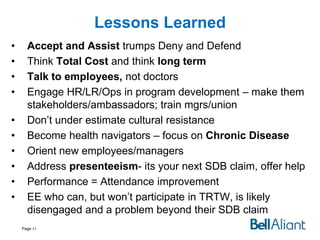
This document outlines Bell Aliant's approach to disability management. It discusses shifting from a medical model to a holistic approach that focuses on the total costs of disability, including indirect costs. Key points include:
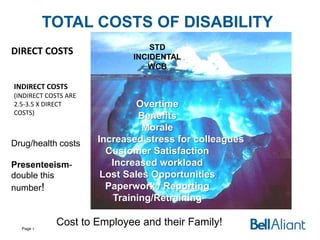
- Traditional disability management focused on direct medical costs but indirect costs are much higher.
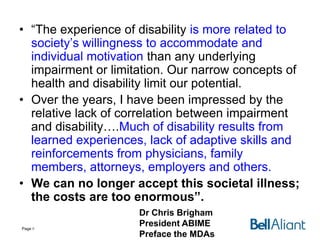
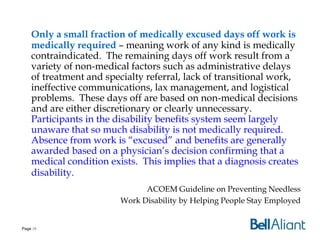
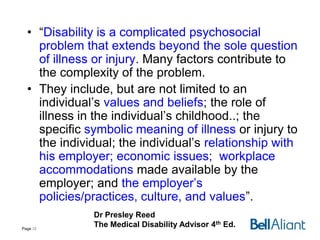
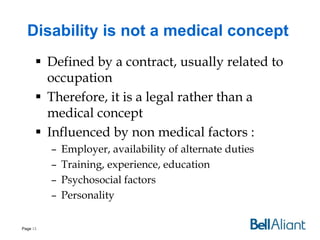
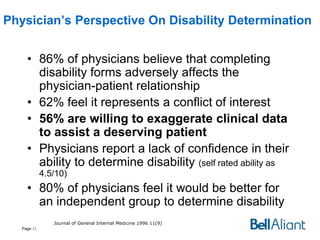
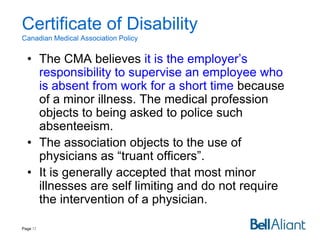
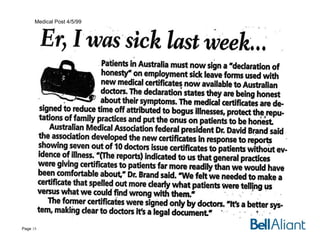
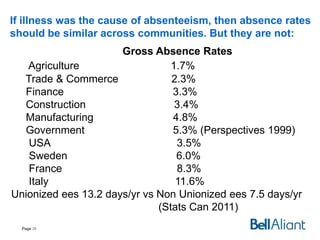
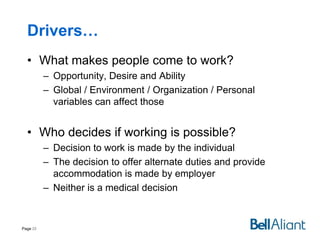
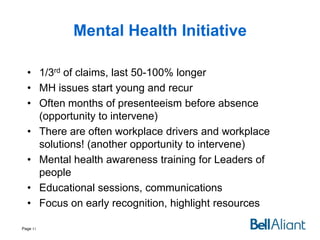
- Disability is influenced more by non-medical factors like workplace policies and individual motivation than underlying medical conditions.
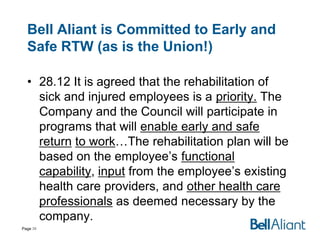
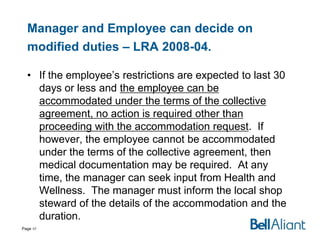
- The goal shifted to "Accept and Assist" employees rather than focus on medical diagnoses and time off work.
- This involves talking to employees, understanding barriers beyond medical issues, and supporting a long-term view of retaining engaged employees.