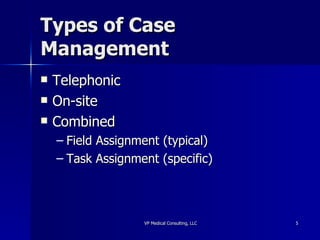
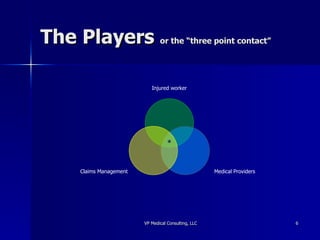
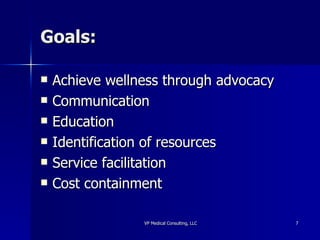
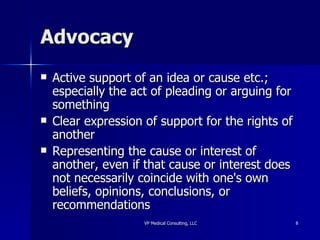
The document outlines the objectives and roles of case management, emphasizing a collaborative process focused on meeting individual health needs through advocacy and communication. It details various types of case management, methods for cost containment, and reasons for referrals, as well as the importance of returning to work and involving employees in the process. Additionally, it discusses resource identification, education, and facilitation as key components of effective case management.