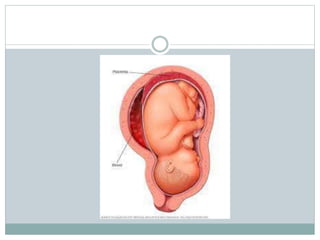
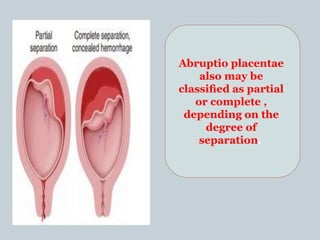
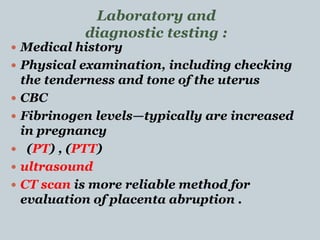
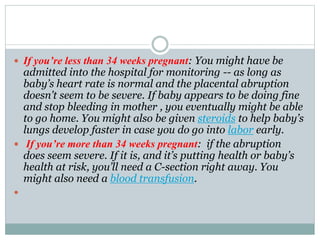
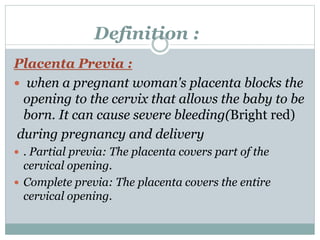
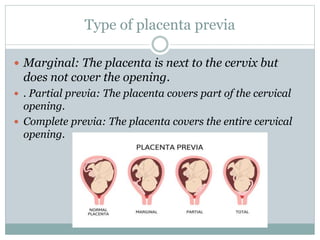
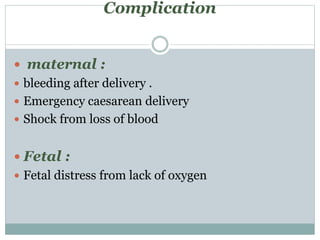
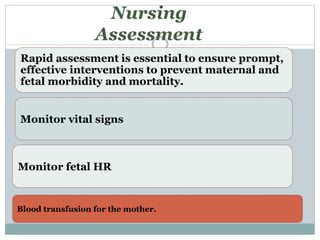
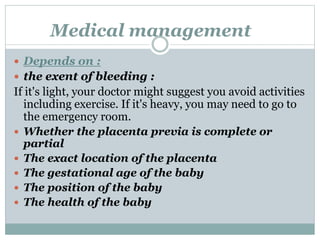
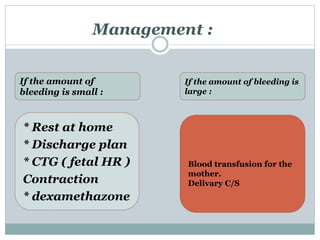
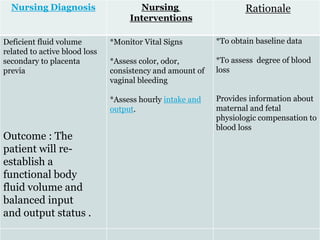
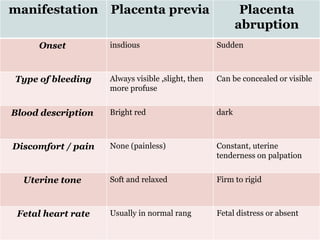
The placenta provides oxygen and nutrients to the growing baby and removes waste from the baby's blood. Placental abruption occurs when the placenta separates from the uterus before delivery, which can decrease the baby's oxygen and cause heavy bleeding in the mother. Placenta previa is when the placenta blocks the cervix, which can cause severe bleeding during pregnancy and childbirth. Both conditions require close monitoring and may necessitate early delivery to prevent complications for the mother and baby.