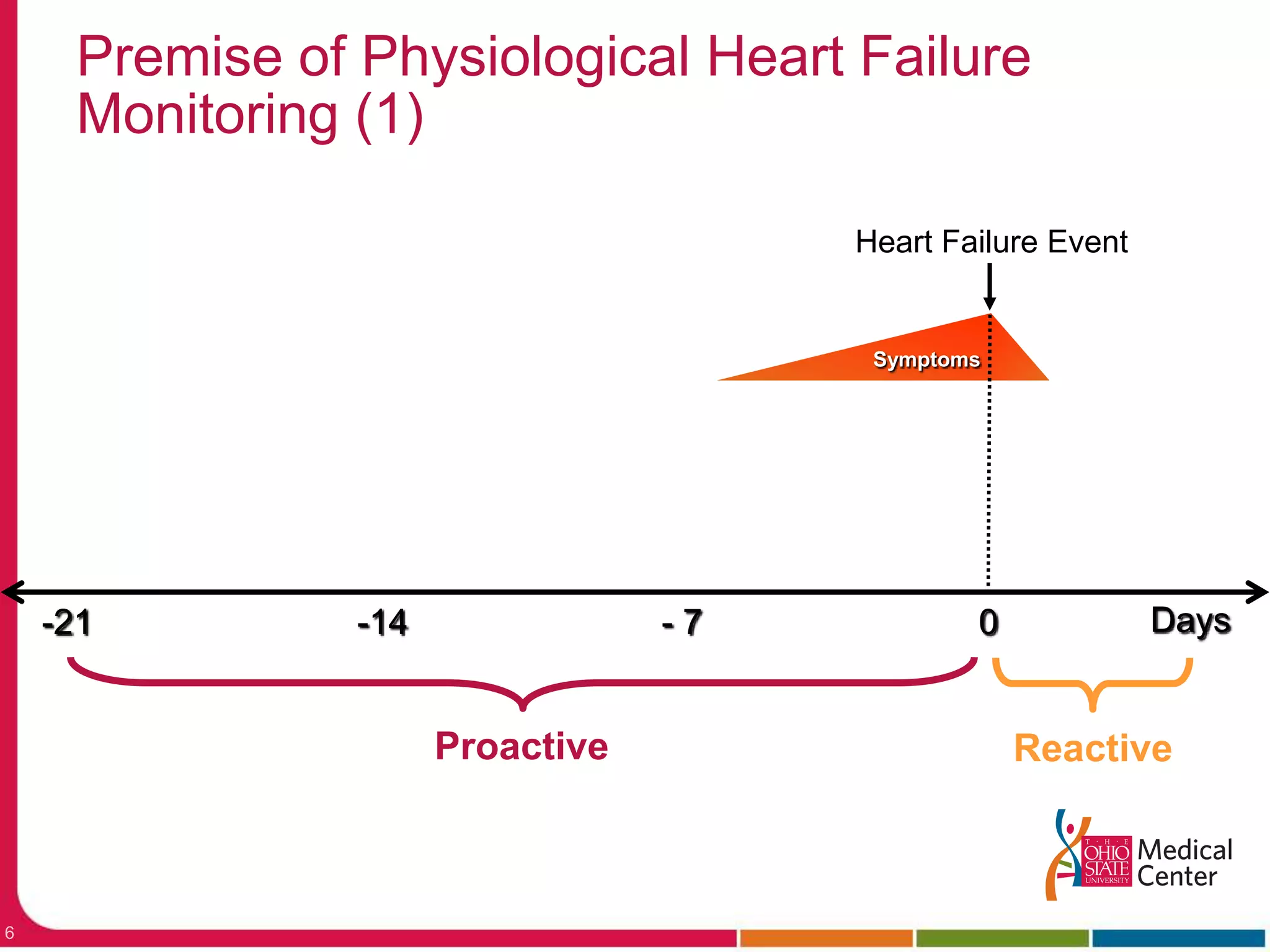
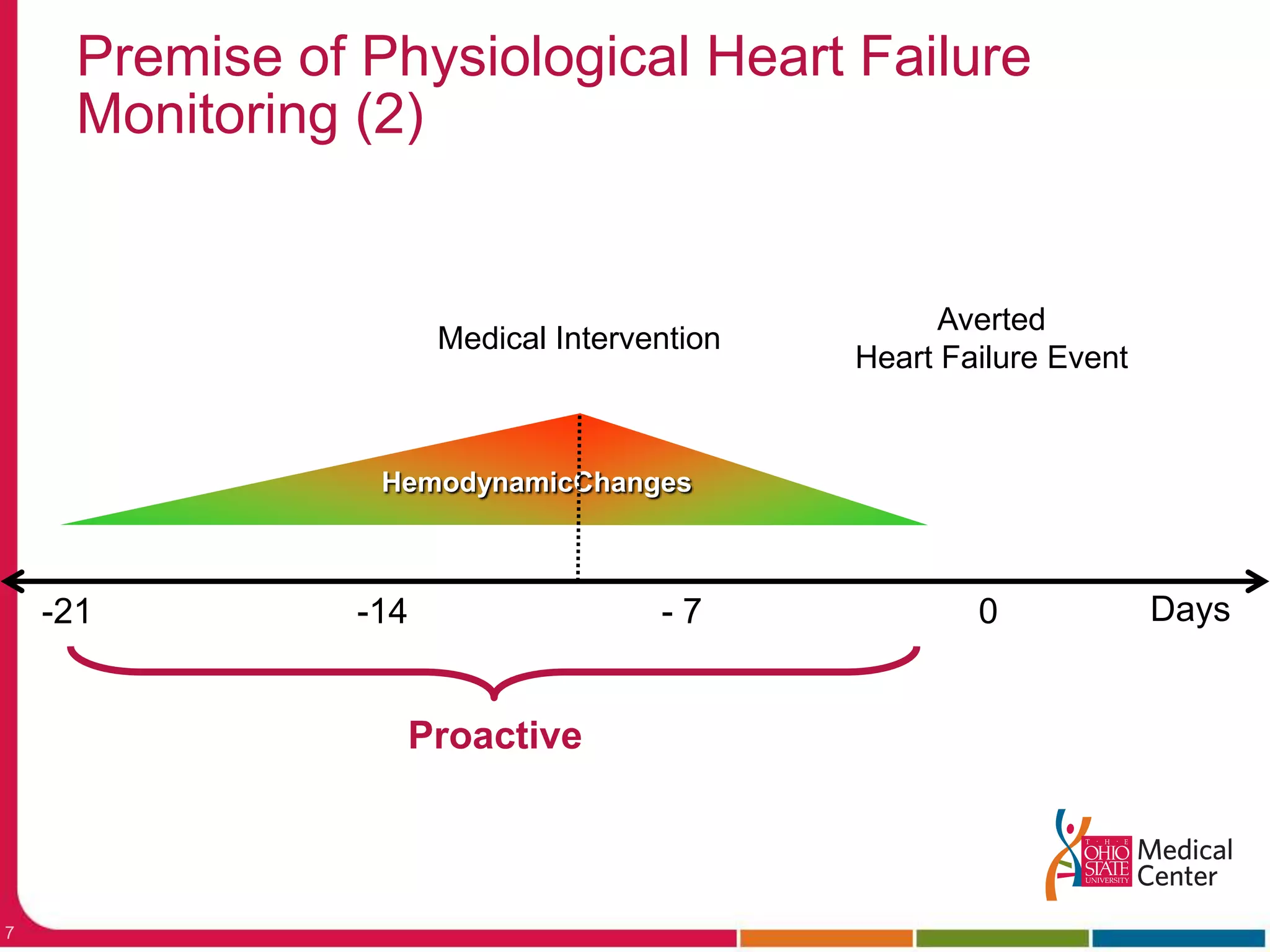
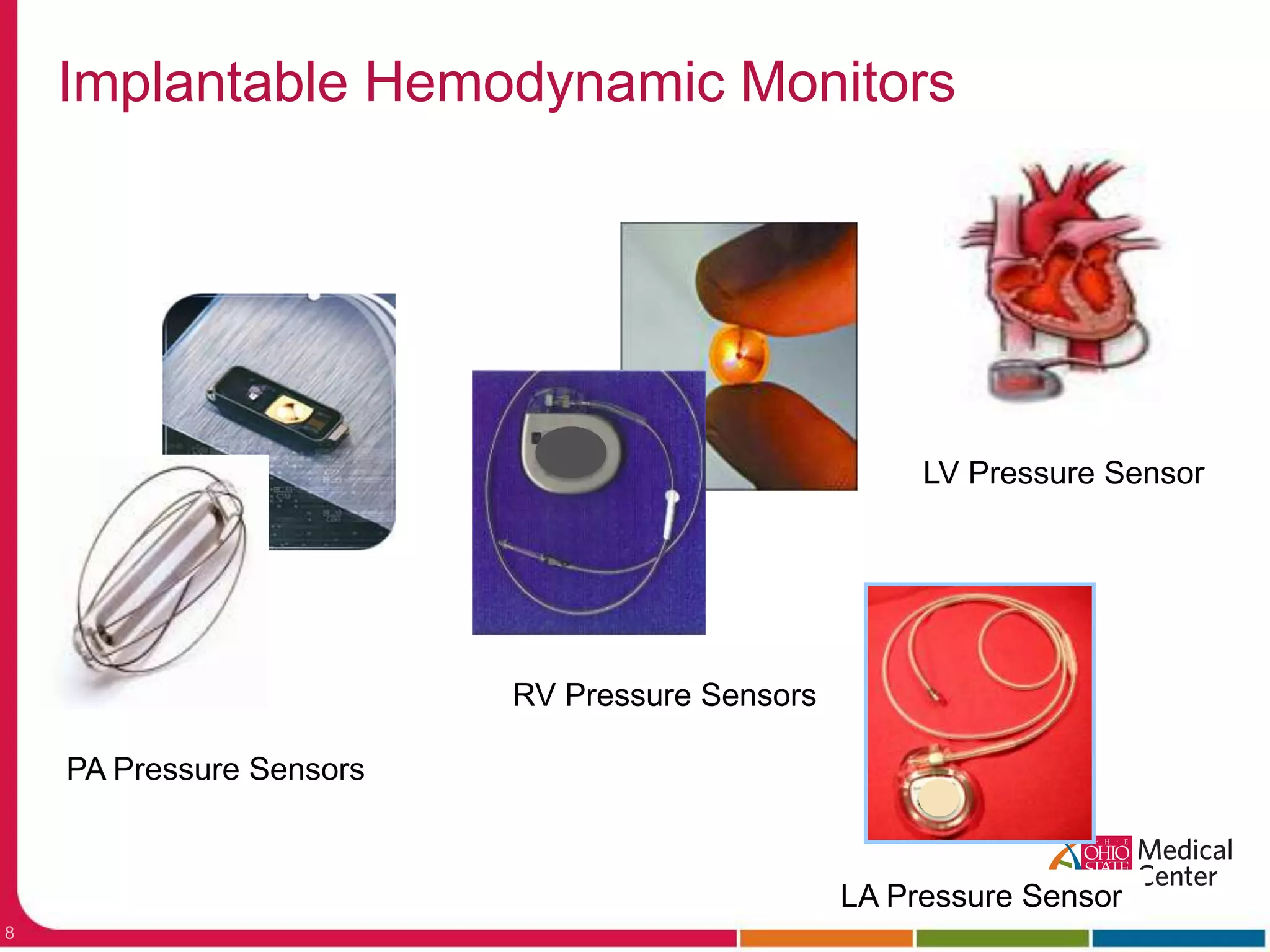
This document discusses new approaches to monitoring heart failure patients using implantable sensors to continuously measure pulmonary artery or left atrial pressures.
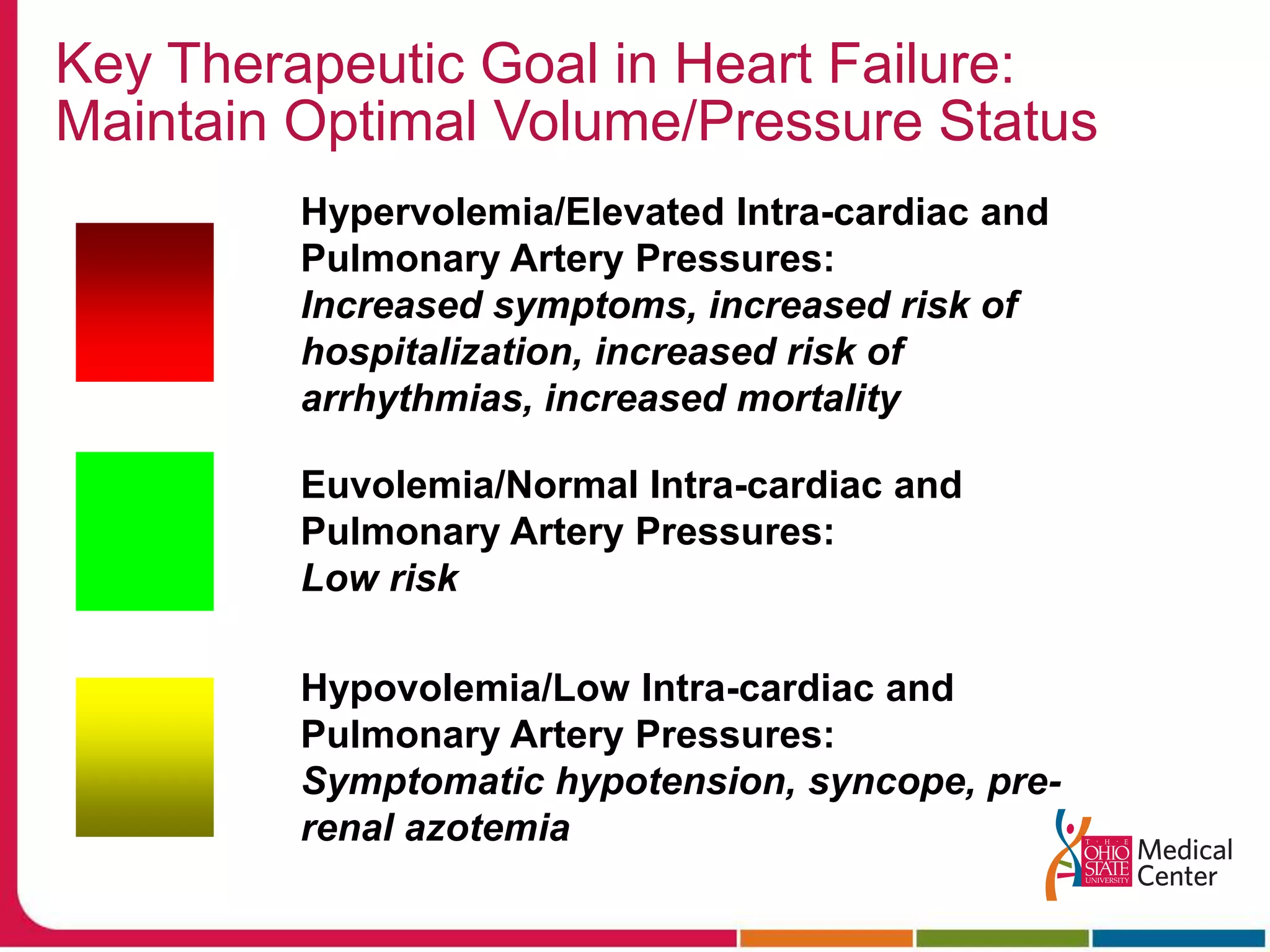
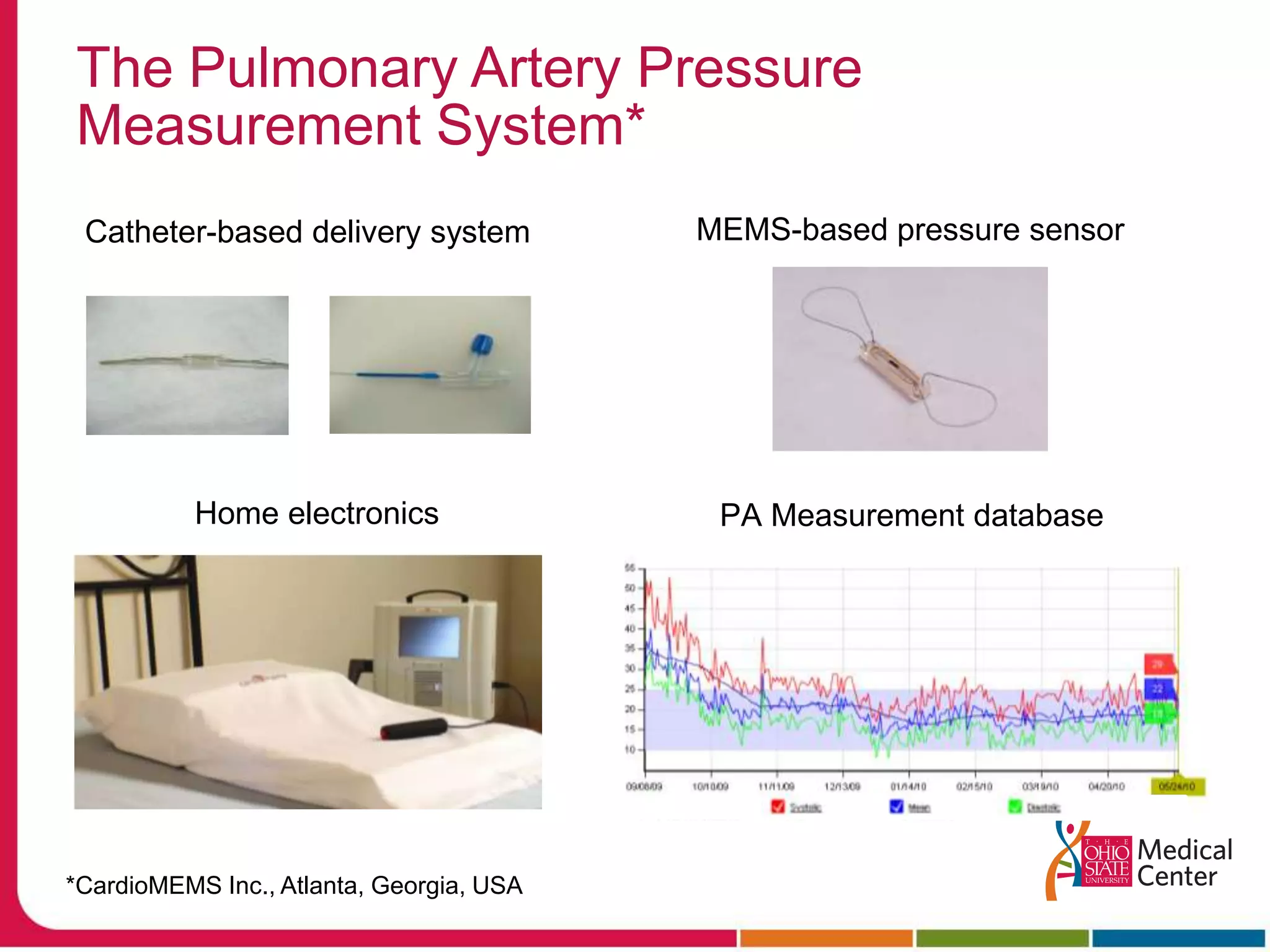
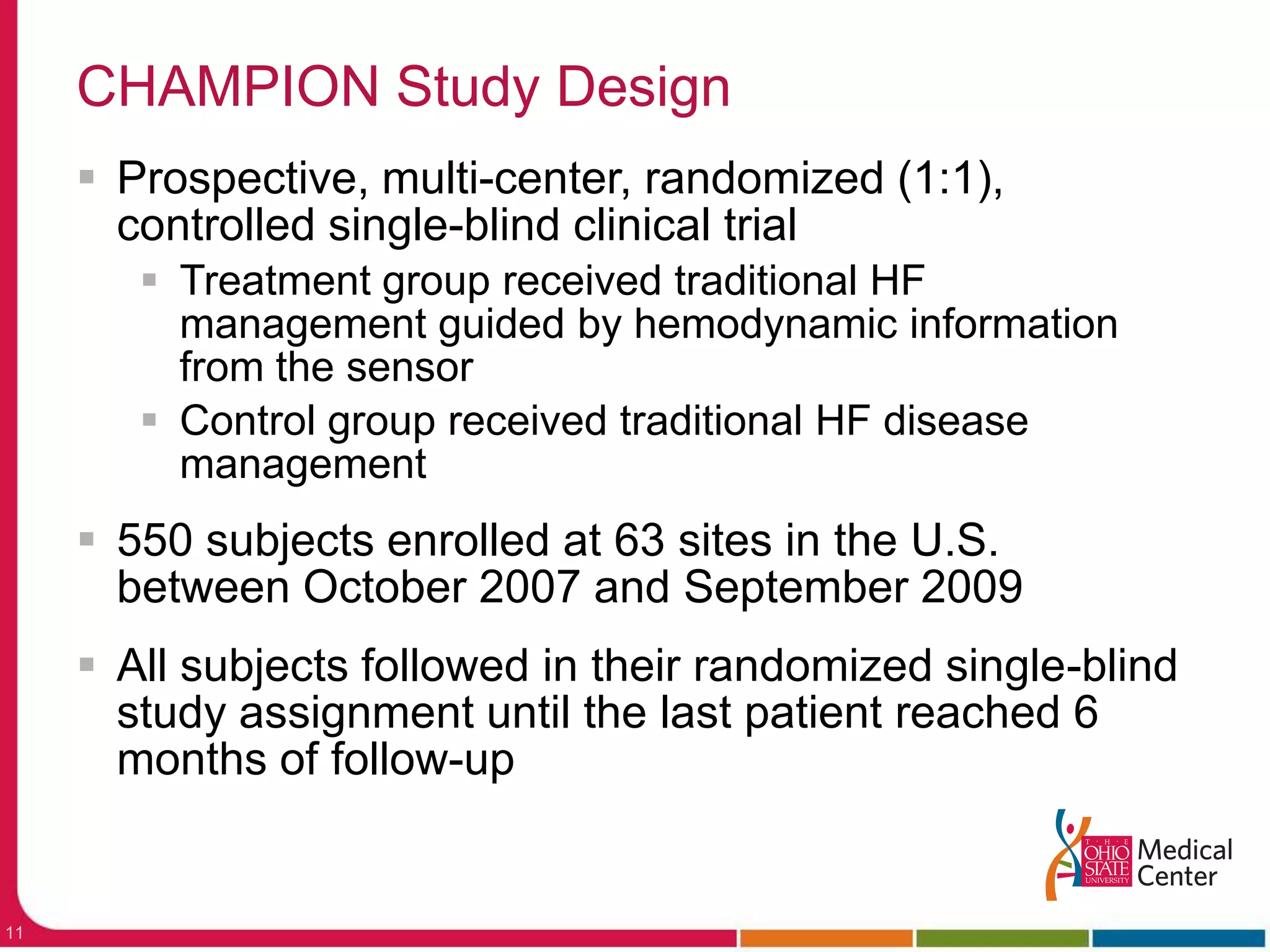
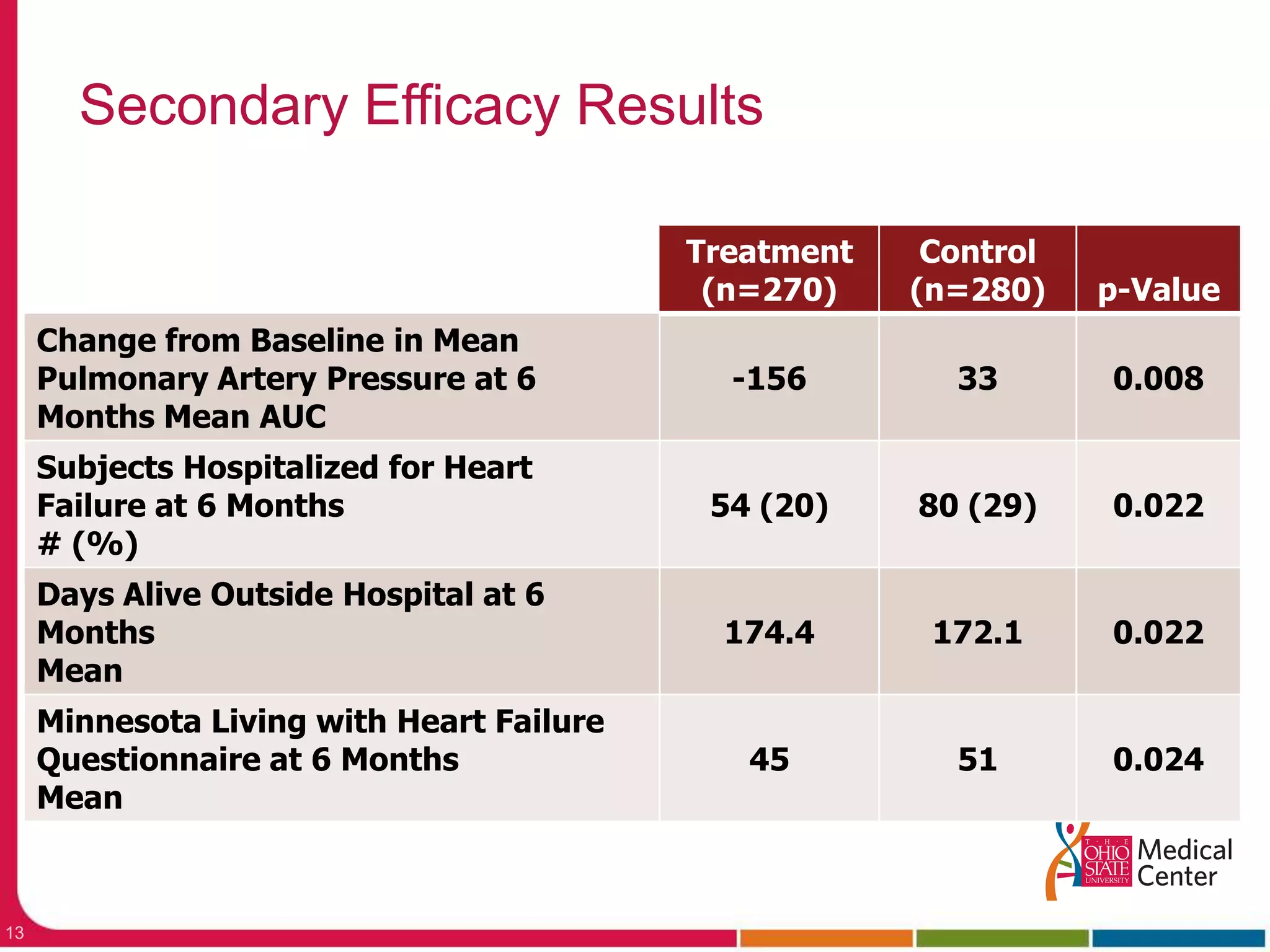
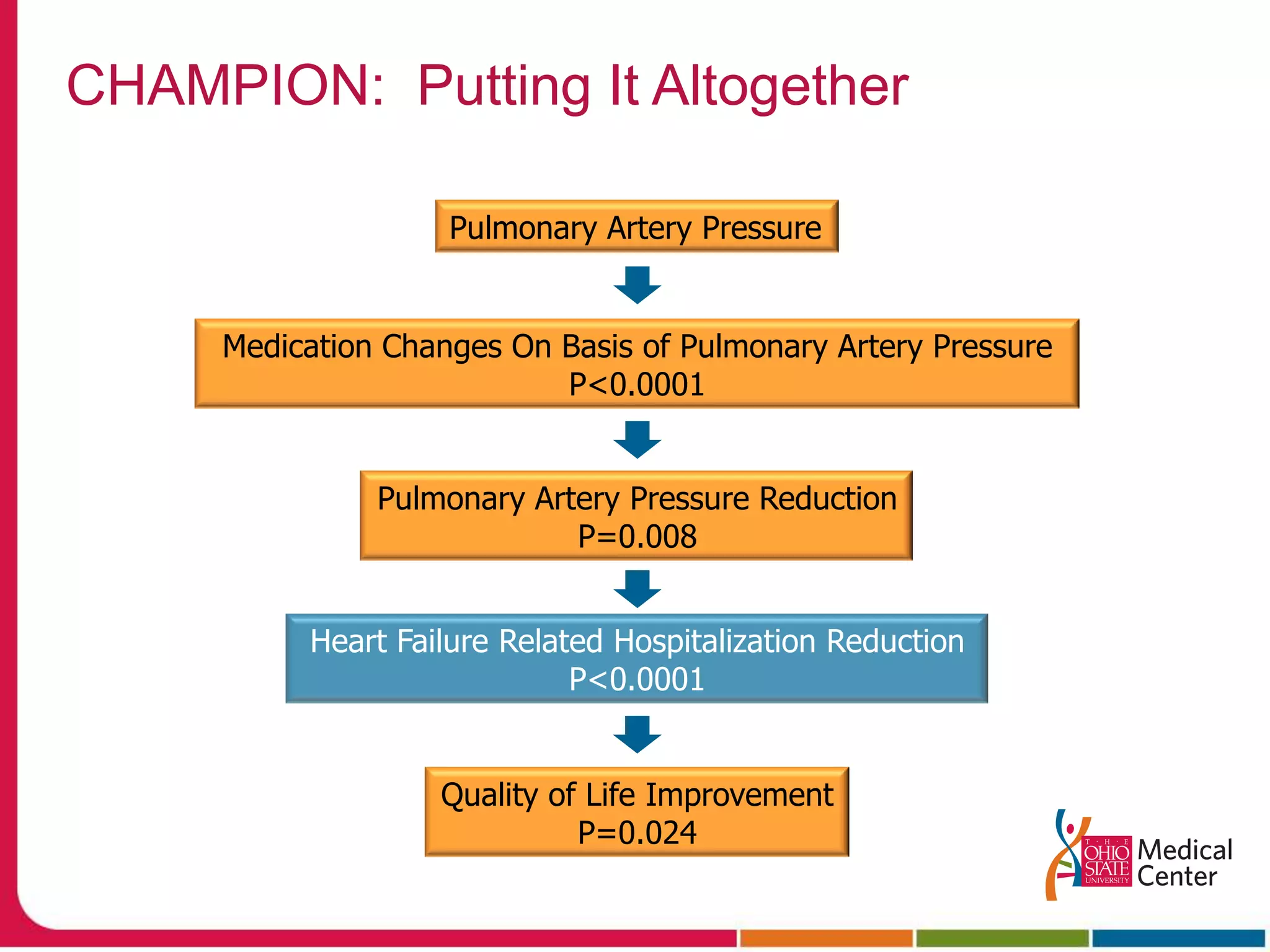
It describes a clinical trial that found implanting a pulmonary artery pressure sensor and using the pressure readings to guide medication adjustments significantly reduced heart failure hospitalizations compared to usual care.
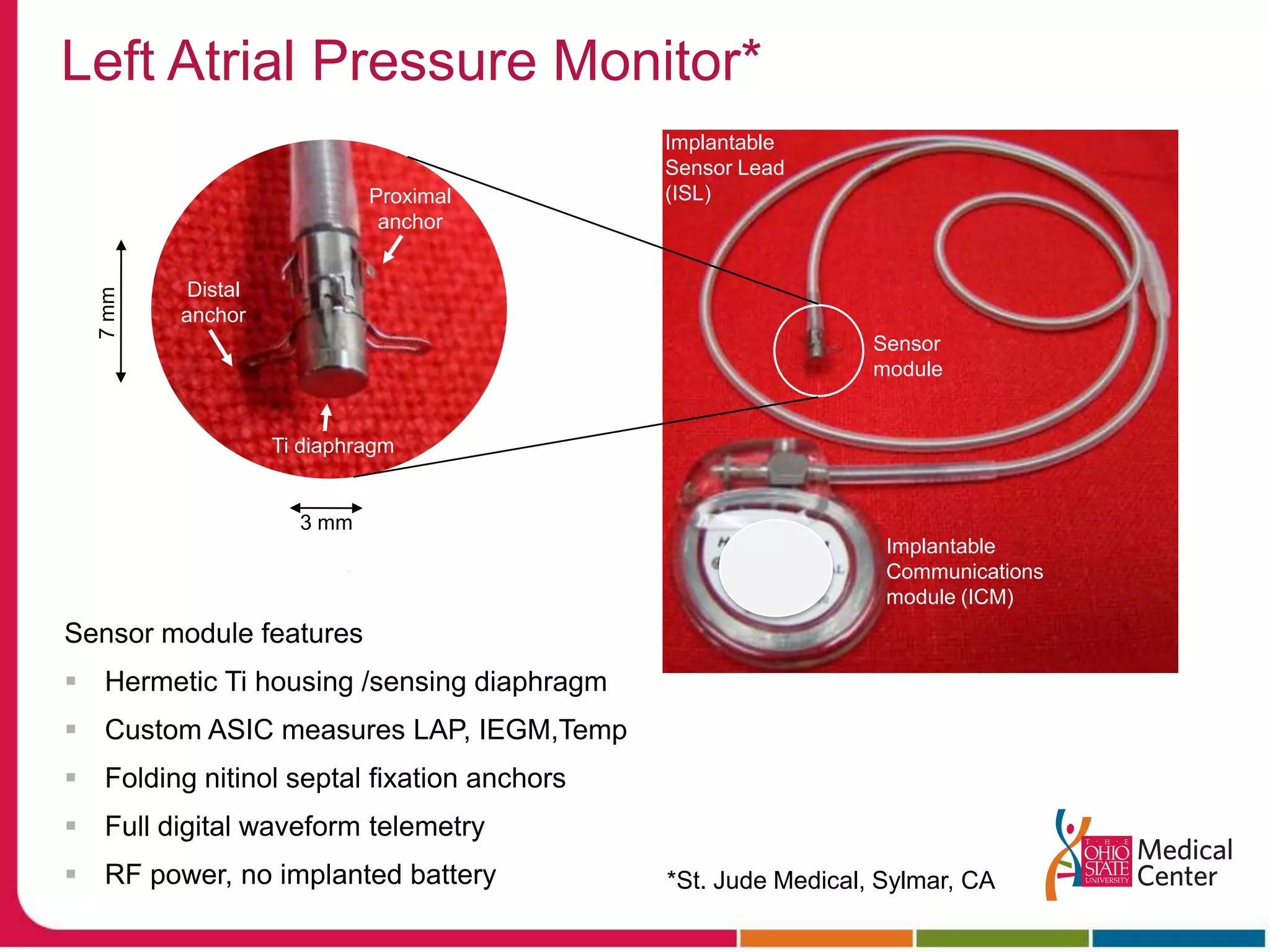
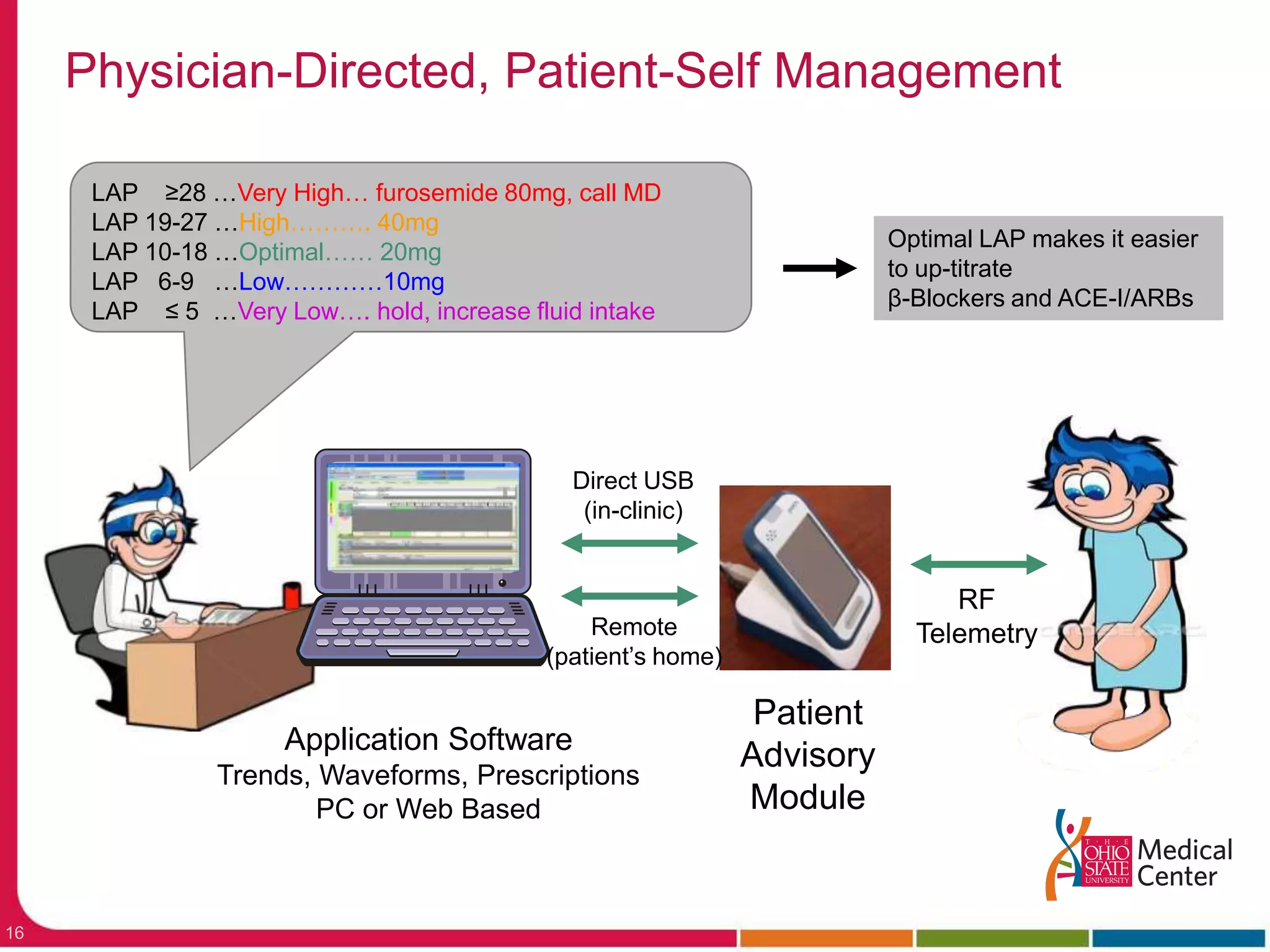
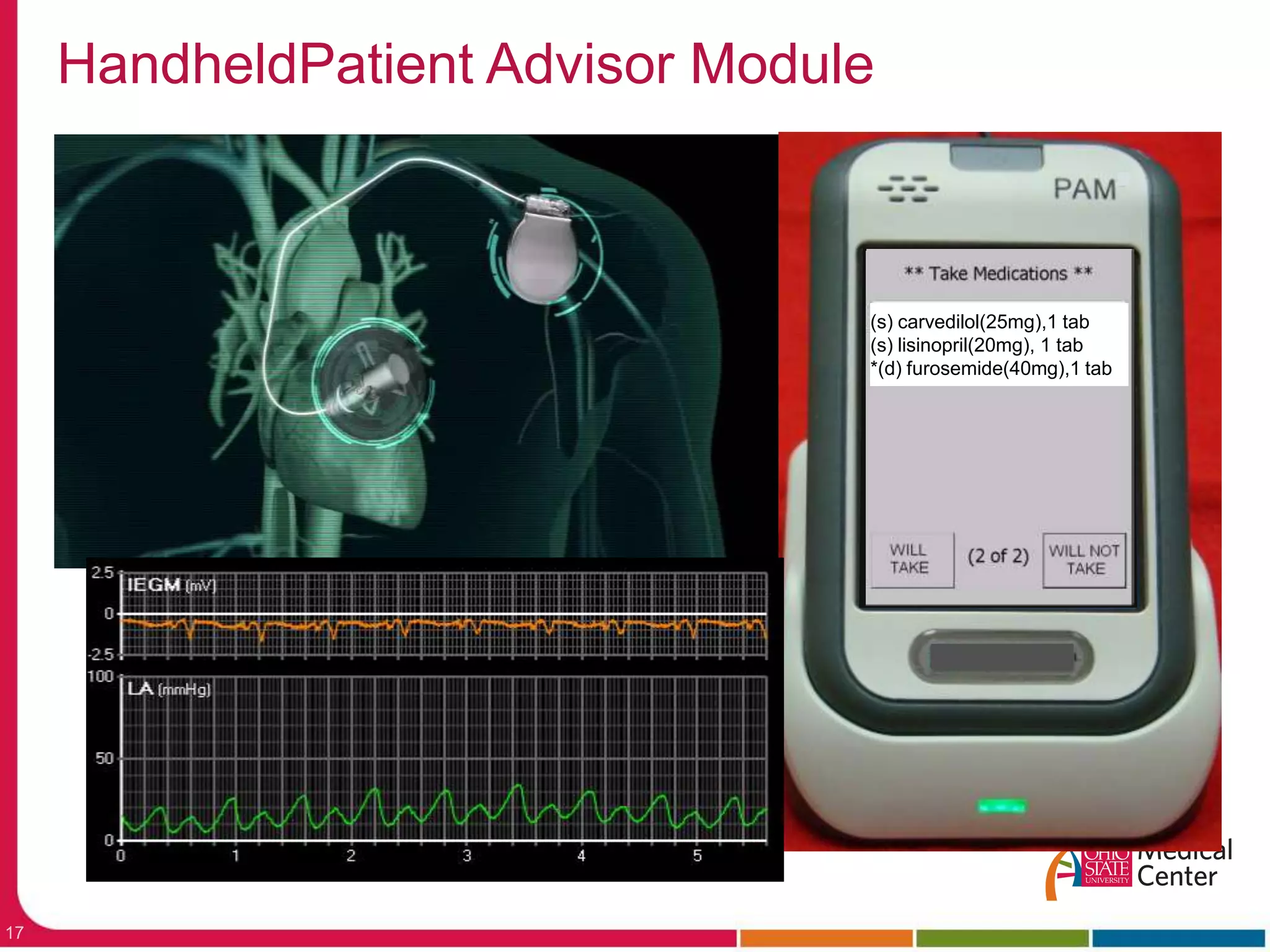
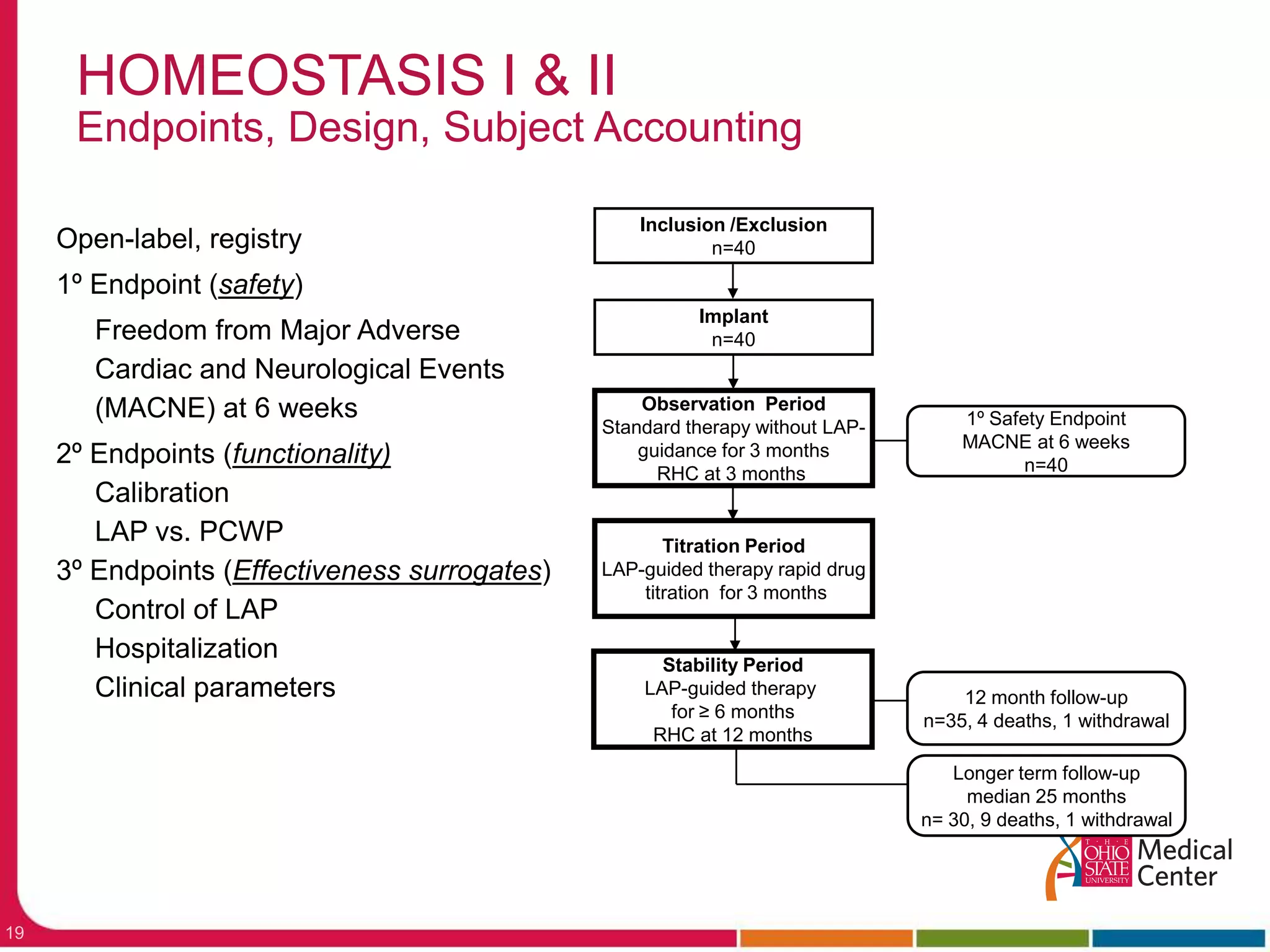
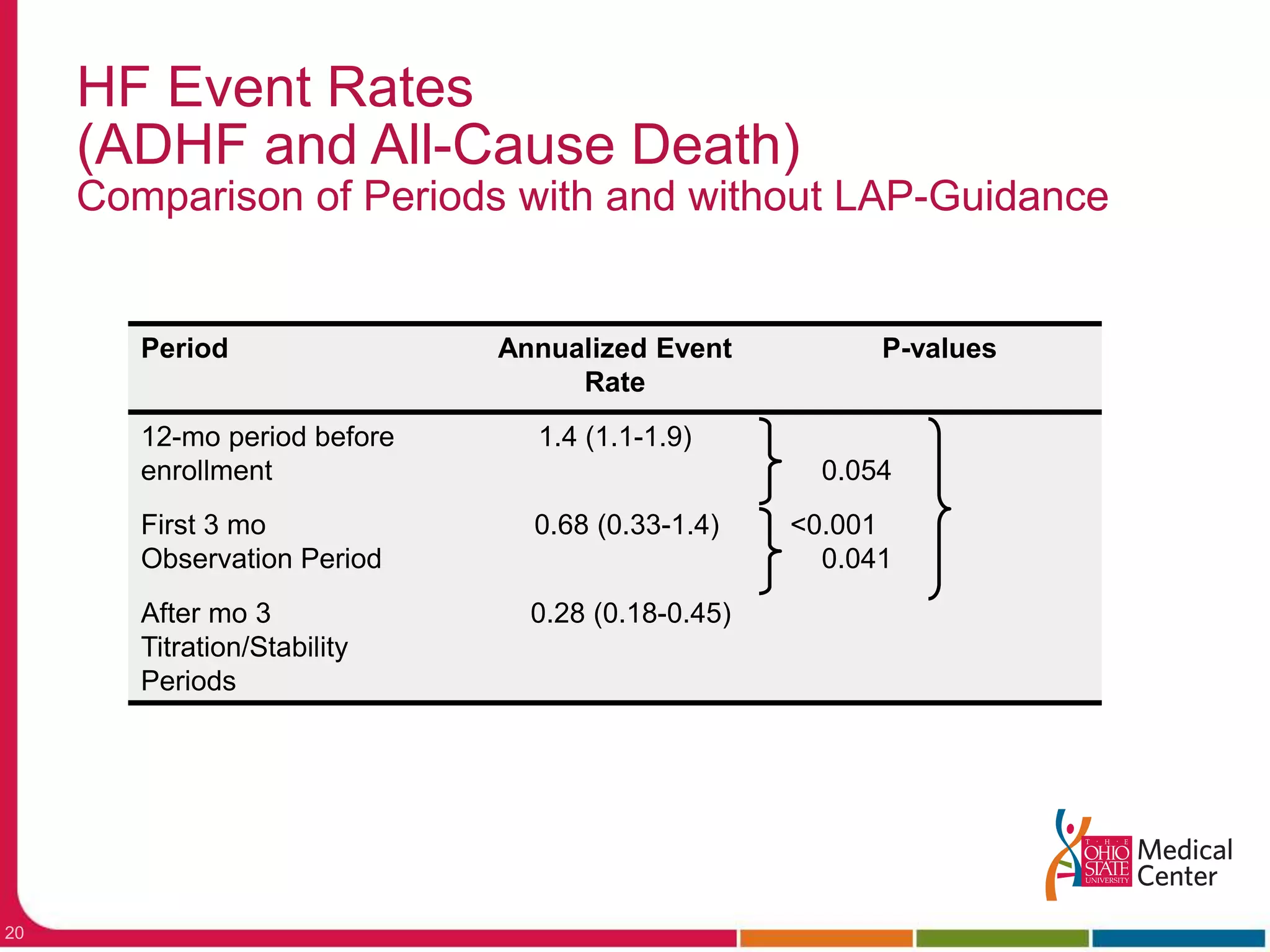
A separate study implanted a left atrial pressure sensor and developed an algorithm to guide diuretic dosing based on pressure levels. Initial results found the sensor remained calibrated over time and the system was able to control left atrial pressures.