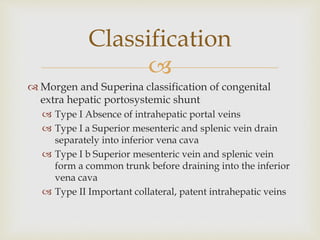
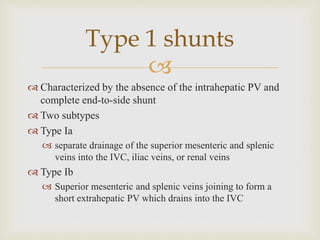
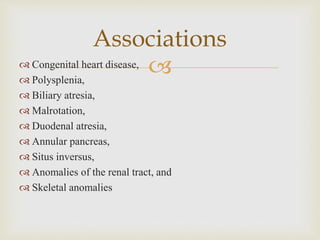
Abernethy malformation is a congenital condition where portal blood is diverted away from the liver, classified into two main types: type I, with absent intrahepatic portal veins, and type II, with patent intrahepatic veins. Symptoms can include hepatic encephalopathy and pulmonary complications, with diagnostic options including ultrasound, CT, and MRI. Management differs between types, with type I requiring monitoring and potential liver transplantation and type II allowing for shunt occlusion in symptomatic cases.