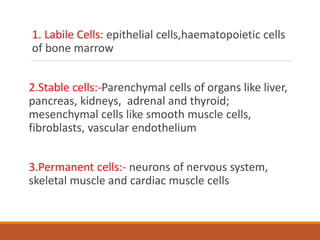
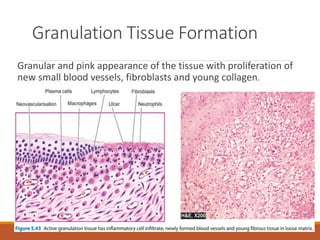
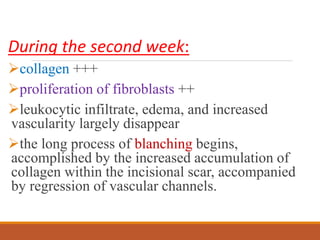
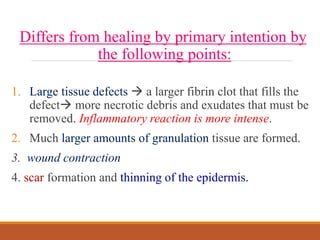
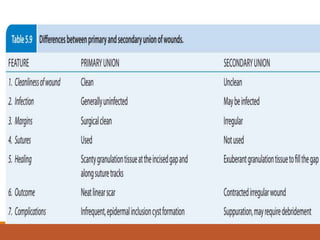
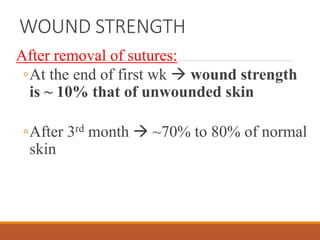
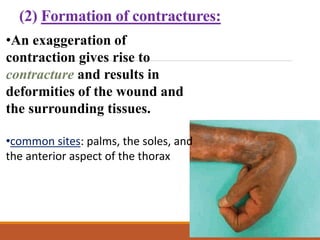
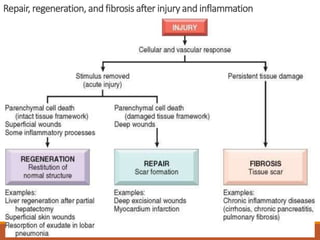
This document discusses tissue repair and wound healing. It begins by defining key terms like repair, regeneration, and healing. It then describes the phases of wound healing as inflammation, granulation tissue formation, and remodeling. The two main types of wound healing are primary intention for clean surgical wounds and secondary intention for wounds with more tissue loss. The process of each is described, involving inflammation, new blood vessel formation, collagen deposition, and epithelialization. Factors that influence healing like nutrition, infection, and wound size are also outlined. Complications can include dehiscence, contractures, and excessive scar formation.