More Related Content Similar to 4 subacute and chronic meningitis (1)
Similar to 4 subacute and chronic meningitis (1) (20) 1. SUBACUTE AND
CHRONIC MENINGITIS
Larry E. Davis
ABSTRACT
Subacute and chronic meningitis represent only about 10% of all infections of
the central nervous system (CNS), but with a growing population of immuno-
compromised patients their frequency is increasing. The number of recognized
etiologies that cause chronic meningitis is also increasing, making it more difficult
to establish the diagnosis. In broad terms, chronic meningitis can be divided into
infectious causes, which include viruses, bacteria, Rickettsia, fungi, and parasites;
and noninfectious causes, which include neoplastic meningitis, CNS vasculitis, and
chemical meningitis. This chapter describes an efficient approach to patients with
chronic meningitis. The steps involved are: (1) Obtain a careful history with
attention to country of origin, recent travel history, other acquaintances
with similar symptoms, exposure to unusual animals, and patient’s immune
status. (2) A careful general physical examination should search for body areas,
including lungs, liver, joints, and skin that may be involved, suggesting a systemic
illness. (3) The neurological examination should look for signs of cranial nerve
palsies, papilledema, and lumbosacral nerve root involvement that give clues as to
the areas of CNS involvement. (4) Cerebrospinal fluid should be examined for the
type of pleocytosis present, cultured for infectious agents, assayed for infectious
agents by polymerase chain reaction, tested for specific antigens, assayed for
presence of specific immunoglobulin M (IgM) antibodies, and examined
cytologically for malignant cells. (5) Neuroimaging, usually magnetic resonance
imaging with gadolinium, should be performed, looking for foci of meningeal
enhancement, parenchymal masses, and hydrocephalus. Suspicious body sites that
could be infected with the systemic infection, especially lungs and joints, should
also be imaged. (6) A tissue biopsy should be considered, especially if a suspicious
skin, lung, liver, or kidney lesion is identified. If neuroimaging identifies an
enhancing meningeal site, biopsy of the arachnoid and pia mater followed by
histological examination may yield the diagnosis.
INTRODUCTION
Meningitis is defined as inflammation
involving the meninges. The meninges
consist of two membranes, the pia and
arachnoid mater, which surround the
brain and spinal cord. These mem-
branes create the subarachnoid space,
which is filled with cerebrospinal fluid
(CSF). Meningitis is classified arbi-
trarily as acute, subacute, and chronic,
depending on the duration of the
inflammation. Acute meningitis has a
rapid onset of symptoms (hours to a
few days) and is usually caused by
etiologies that are different from those
that produce subacute and chronic
meningitis. Subacute meningitis has
an onset that is slower, evolving typi-
cally over days to a few weeks. Chronic
meningitis is defined as a syndrome
of persistent signs and symptoms last-
ing at least 4 weeks without clinical
improvement and coupled with con-
tinued CSF inflammation.
Today, most patients seek medi-
cal attention before 1 month for
27
KEY POINT:
A Chronic
meningitis
is defined as
a syndrome
of persistent
signs and
symptoms
lasting at
least 4 weeks
without
clinical
improvement
and coupled
with continued
CSF
inflammation.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
2. symptoms of their meningitis, making
it initially difficult to determine wheth-
er the diagnosis is subacute or chronic
meningitis. Because both subacute
and chronic meningitis have similar
clinical features and etiologies, the
distinction is unimportant. According-
ly, this article will address both con-
ditions as one and will use the term
chronic meningitis. Several reviews of
chronic meningitis have been pub-
lished (Ellner and Bennett, 1976;
Hildebrand and Aoun, 2003; Tan, 2003;
Wilhelm and Ellner, 1986; Wilhelm and
Marra, 1992), but few published case
series exist.
Because so many causes of chronic
meningitis exist, this article will focus on
how to efficiently establish the diagno-
sis. The reader is referred to cited re-
view articles regarding detailed manage-
ment of the specific diseases presented.
Historically, tuberculosis was the
most common cause of chronic men-
ingitis. While tuberculous meningitis
remains a common cause, its inci-
dence in the United States is far less
than the 40% that often was reported
in earlier series from other countries
(Anderson and Willoughby, 1987).
Several reasons account for the chang-
ing pattern of causes: (1) The preva-
lence of tuberculosis has fallen sharply
in developed countries. (2) An increas-
ing number of immunocompromised
patients develop unusual opportunis-
tic meningeal infections. (3) More
opportunistic infections and noninfec-
tious etiologies, especially leptome-
ningeal metastases and vasculitis, are
being recognized. Consequently, the
list of possible causes of chronic
meningitis is continually expanding.
Unfortunately, still no etiology can
be identified in 15% to 25% of cases
of chronic meningitis (Ellner and
Bennett, 1976).
As the list of possible causes
expands, the cost of a workup is
becoming expensive. For several rea-
sons, it is difficult to reduce costs by
sequencing the ordering of tests based
on their prevalence because many
patients clinically worsen if appropri-
ate treatment is delayed. In addition,
most of the infectious etiologies grow
slowly in culture (up to 3 to 6 weeks
for Mycobacterium tuberculosis) so
one cannot wait for negative results
before expanding the workup. The
current workup of a patient with
undiagnosed chronic meningitis often
includes: (1) imaging of the head; (2)
several CSF examinations with exten-
sive cultures, polymerase chain re-
action (PCR) assays, and multiple
serological tests; (3) imaging, biopsies,
and cultures of other body sites; (4)
serological tests for causes of vasculitis
and other autoimmune diseases; and
(5) cytological CSF examinations for
malignant cells. The cost of an exten-
sive workup including neuroimaging
and laboratory tests often runs into
many thousands of dollars. If brain
biopsy is required, the cost increases
again.
To better organize the many causes
of chronic meningitis, the etiologies
may be classified in several different
ways. The most straightforward is to
divide the causes into common and
uncommon (Table 2-1). The second
is to divide the causes into infectious
and noninfectious, each with appro-
priate subcategories (Table 2-1). The
third method is to categorize the
etiologies by the predominant CSF
cell type (Table 2-2).
The fourth method is to divide the
etiologies of chronic meningitis by
their severity (Table 2-3). The chronic
meningitis in some patients is intense
and causes severe illness. These
patients usually have markedly elevat-
ed CSF white blood cell (WBC) counts
(100 cells/mm3
to 1000 cells/mm3
) (or
neoplastic cells) and markedly elevat-
ed CSF protein levels (100 mg/dL
to greater than 1000 mg/dL). CSF
28
KEY POINT:
A While
tuberculous
meningitis
remains a
common cause
of chronic
meningitis, its
incidence in
the United
States is far
less than the
40% that often
was reported
in earlier series
from other
countries.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
3. 29
TABLE 2-1 Causes of Chronic Meningitis
Infectious Causes Noninfectious Causes
" Viruses " Vasculitis
Human immunodeficiency virus* Giant cell arteritis*
Enteroviruses in
agammaglobulinemia
Primary central nervous
system angiitis
Cytomegalovirus Amphetamine and cocaine abuse*
Herpes simplex type 2 Benign angiitis of central
nervous system
Lymphocytic choriomeningitis
Churg-Strauss syndrome
Mumps
Cogan’s syndrome
Varicella-zoster
Cryoglobulinemia
" Bacteria
Hypersensitivity vasculitis
Treponema pallidum (neurosyphilis)*
Kawasaki’s disease
Borrelia burgdorferi (Lyme disease)*
Polyarteritis nodosa
Mycobacterium tuberculosis*
Takayasu’s arteritis
Actinomyces species
Wegener granulomatosis
Bartonella henselae
(catscratch disease) Paraneoplastic central nervous
system vasculitis
Brucella species (brucellosis)
" Connective Tissue Diseases
Chlamydia pneumoniae
and trachomatis Systemic lupus erythematosus*
Coxiella burnetii (Q fever) Dermatomyositis
Francisella tularensis (tularemia) Mixed connective-tissue disease
Infectious endocarditis Rheumatoid arthritis
Leptospira species (leptospirosis) Sjo¨ gren syndrome
Listeria monocytogenes " Chemical Meningitis
Nocardia asteroides Endogenous
Staphylococcus epidermidis Dermoid cyst*
Staphylococcus aureus Craniopharyngioma
Streptococcus species Embryonal tumors
Tropheryma whipplei
(Whipple’s disease)
Epidermoid cyst
" Rickettsia
Malignant glioma
Ehrlichia chaffeensis
Teratoma
(human monocytic ehrlichiosis)*
Exogenous
Anaplasma phagocytophila
(human granulocytic ehrlichiosis)
Trimethoprim-sulfamethoxazole*
continued on next page
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
4. 30
TABLE 2-1 Continued
Infectious Causes Noninfectious Causes
Intravenous immunoglobulin*Babesia species
Craniotomy*Rickettsia typhi (endemic typhus)
Intrathecal anesthetic agentsRickettsia prowazekii
(epidemic typhus)
Isoniazid
Nonsteroidal anti-inflammatory
agents
Rickettsia rickettsii (Rocky
Mountain spotted fever)
Monoclonal antibodies
(muromonab-CD3 [OKT3])
" Fungi
Carbamazepine
Coccidioides immitis*
Intrathecal drug administration
Cryptococcus neoformans*
Amphotericin B
Histoplasma capsulatum*
Corticosteroids
Blastomyces dermatitidis*
Metrizamide myelography
Aspergillus species*
Pantopaque myelography
Candida species*
Neurosurgical procedures
Cladosporium
Reflux of lumbar-gallbladder
shunt
Paracoccidioides brasiliensis
" Leptomeningeal Metastasis
Phialophora species
(chromoblastomycosis)
Primary brain tumors
Pseudoallescheria boydii
Angiocentric lymphoma
Sporothrix schenckii
Meningioma
Trichosporon beigelii
Craniopharyngioma cyst
Zygomycetes species
Medulloblastoma
" Parasites
Glioma
Taenia solium
Systemic tumors, especially
(neurocysticercosis)*
Breast*
Acanthamoeba (granulomatous
amebic meningoencephalitis)
Lung*
Leukemia*
Angiostrongylus cantonensis
Melanoma*
(eosinophilic meningitis)
Gastrointestinal
Baylisascaris procyonis
Lymphoma
Coenurus cerebralis
Hodgkin’s lymphoma
Echinococcus species
Entamoeba histolytica
Fasciola hepatica
Gnathostoma spinigerum
Naegleria fowleri
Atrial myxoma
continued on next page
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
5. hypoglycorrhachia may be present.
Untreated, these meningitides may
cause cranial nerve palsies, marked
meningeal vasculitis with secondary
subarachnoid hemorrhages and infarc-
tions, and/or blockage of CSF pathways
causing hydrocephalus. There is a
greater sense of urgency to establish
the diagnosis and appropriately treat
the patient as the illness progresses
fairly rapidly. In other patients with
chronic meningitis, the inflammation
is less intense. These patients have
modest elevations in CSF WBC count
(less than 100 cells/mm3
) and only
mild elevation of protein level (less
than 100 mg/dL). Less intense forms
of meningitis uncommonly progress
to arachnoiditis, cause obstructive hy-
drocephalus, or create a vasculitis
sufficient to produce subarachnoid
hemorrhages or brain infarctions. Any
given etiology may begin as low
grade and advance to high grade, and,
conversely, etiologies that usually
cause high-grade meningitis may in
some individuals first appear as low
grade. It should also be noted that
in patients who are immunocompro-
mised, the CSF profile may appear
benign, but the neurological disease
can rapidly progress.
The challenge for the clinician is to
narrow this large list of causes. Fortu-
nately, following the strategies given
below can shorten the list of possible
diagnoses. Nevertheless, it must be
recognized that in 15% to 25% of
patients with chronic meningitis, no
diagnosis is established.
31
TABLE 2-1 Continued
Infectious Causes Noninfectious Causes
Paragonimus westermani " Subarachnoid Hemorrhage
Schistosoma species Leaky aneurysm
Strongyloides stercoralis
Toxocara canis
Toxoplasma gondii
Trichinella spiralis (trichinosis)
Trypanosoma cruzi
Trypanosoma brucei complex
" Suspected to Be Infectious
Neurosarcoidosis*
Hypertrophic pachymeningitis
Behc¸et’s disease
Chronic benign lymphocytic meningitis
Parameningeal infections
Persistent neutrophilic meningitis
Vogt–Koyanagi-Harada syndrome
Mollaret’s meningitis
*More common causes in the United States.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
6. 32
TABLE 2-2 Causes of Chronic Meningitis Frequently With Atypical
Cerebrospinal Fluid Pleocytosis
Neutrophil Cerebrospinal
Fluid Predominance
Greater Than 10% Eosinophils
in Cerebrospinal Fluid
Bacteria
Mycobacterium tuberculosis (early)
Brucella species
Actinomyces species
Nocardia asteroides
Fungi
Aspergillus species Coccidioides immitis
Blastomyces dermatitidis
Candida species
Coccidioides immitis
Histoplasma capsulatum
Pseudallescheria boydii
Zygomycetes species
Parasites
Angiostrongylus cantonensis
Baylisascaris procyonis
Echinococcus species
Fasciola hepatica
Gnathostoma spinigerum
Paragonimus westermani
Schistosoma species
Taenia solium
Toxocariasis species
Trichinella spiralis
Noninfectious Causes
Chemical- or drug-induced meningitis Hodgkin’s lymphoma
Craniotomy Lymphoma/leukemia
Behc¸et’s syndrome Medulloblastoma with meningeal
spread
Parameningeal infection Glial tumors with meningeal spread
Vasculitides Systemic lupus erythematosus
The other etiologies listed in Table 2-1 have a lymphocytic predominance in cerebrospinal
fluid.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
7. HISTORY
The first step is to distinguish between
acute and chronic meningitis because
the causes differ. While acute menin-
gitis has an abrupt onset over hours to
a few days, chronic meningitis has a
slower course with symptoms devel-
oping over many days to weeks.
Although the intensity of the symp-
toms in chronic meningitis may fluc-
tuate slightly, the collection of symp-
toms does not completely disappear
as it does in recurrent meningitis.
In taking the history, several areas
often yield helpful clues in narrowing
the differential diagnosis (Table 2-4):
o Place of origin and recent
travel. Infectious agents are not
equally distributed in the world,
and knowledge of where the
individual lives or has recently
traveled may give clues.
o Past history and review of
symptoms. Since some causes of
chronic meningitis are contagious,
one should inquire whether
family, relatives, and work or
neighborhood friends have a
similar illness. Knowledge that
the patient had specific diseases in
the past, has used intravenous
recreational drugs, or has had
a positive tuberculin skin test
may be helpful. Many causes
of chronic meningitis affect
organs outside the nervous system.
Knowledge of what other organs
are affected can help focus the
workup (Table 2-5).
o Animal exposures. Some causes
of chronic meningitis are
zoonoses, and knowledge of
specific animal exposures may
be helpful.
o Immune status. Individuals
who have defects in their cellular
or humoral immunity are at
considerably higher risk for
developing chronic meningitis
from opportunistic infections
(organisms that normally do not
cause disease in healthy
individuals).
In addition, the spectrum of oppor-
tunistic infections differs in some spe-
cific types of immunosuppression (see
Marra, 2004, for spectrum of infections
associated with human immunodefi-
ciency virus [HIV] infection and chap-
ter, Infections of the Central Nervous
System in Patients Infected With
Human Immunodeficiency Virus in this
issue for infections associated with
transplant infections).
33
TABLE 2-3 Common
Etiologies of Severe
Chronic Meningitis*
" Bacterial Meningitis
Mycobacterium tuberculosis
" Fungal Meningitis
Coccidioides immitis
Histoplasma capsulatum
Cryptococcus neoformans
Blastomyces dermatides
Paracoccidioides brasiliensis
" Parasitic Meningitis
Naegleria fowleri
Acanthamoeba
Entamoeba histolytica
Taenia solium (meningeal
and ventricular cysts)
Schistosoma species
" Other Causes
Hypertrophic pachymeningitis
Leptomeningeal metastasis
Systemic vasculitis involving
the central nervous system
*See text for definition of intense men-
ingitis.
KEY POINT:
A The first step
is to distinguish
between acute
and chronic
meningitis
because the
causes differ.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
8. 34
TABLE 2-4 Diagnostic Clues Found in History
History Unique Factor
Etiology of Chronic Meningitis Associated
With Unique Risk Factor
Living location
or recent travel
Southwest United States Coccidioides immitis
Midwest Histoplasma capsulatum, Blastomyces dermatitidis,
Ehrlichia chaffeensis
Northeast, upper Midwest,
Northwest
Borrelia burgdorferi, Ehrlichia phagocytophila,
Babesia species
East Coast Neurosarcoidosis, Rickettsia rickettsii
Immigration from Mexico,
Central or South America
Taenia solium, Trypanosoma cruzi, Paracoccidioides
brasiliensis
Asia Angiostrongylus cantonensis, Paragonimus
westermani
Mediterranean region Brucella species
Africa Trypanosom brucei species
Past or current
history of systemic
disease
Cancer Leptomeningeal metastases, opportunistic infections
Lung disease Mycobacterium tuberculosis, Coccidioides immitis,
Histoplasma capsulatum, Blastomyces dermatitidis,
Nocardia asteroides, neurosarcoidosis, lung tumor
Skin rash or infection Coccidioides immitis, Blastomyces dermatitidis,
Borrelia burgdorferi, Treponema pallidum, collagen
vascular disease, systemic vasculitis
Sinus infection Zygomycetes species (mucormycosis), parameningeal
infection, Wegner granulomatosis
Joint swelling Rheumatoid arthritis, Coccidioides immitis, Borrelia
burgdorferi
Iritis, uveitis Behc¸et’s syndrome, Vogt-Koyanagi-Harada
syndrome, Treponema pallidum
Animal exposure Goats or unpasteurized milk Brucella species, Listeria monocytogenes
Cat scratches Bartonella henselae
Pigs Leptospira species
Rabbits, squirrels, muskrats Francisella tularensis
Human
immunodeficiency
virus infection
Low T4 white blood
cell count
Cryptococcus neoformans, Toxoplasma gondii,
Mycobacterium tuberculosis, and all other infections
in Tables 2-1 and 2-2
Immune deficiency Agammaglobulinemia Enterovirus
Granulocyte deficiency Aspergillus species
Corticosteroids Mycobacterium tuberculosis, Candida species,
Cryptococcus neoformans
Pregnancy Coccidioides immitis
Diabetes mellitus Zygomycetes species (mucormycosis)
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
9. PHYSICAL EXAMINATION
Seldom does the physical examination
yield a specific diagnosis. However,
knowledge of what other parts of the
body are involved can narrow the
differential diagnosis (Table 2-5). Of-
ten an affected site outside the CNS
can be biopsied for culture and
35
TABLE 2-5 Diagnostic Clues Found in the Physical Examination
Organ Clinical Finding
Etiology of Chronic Meningitis
Associated With Clinical Findings
Eye Iritis or uveitis Behc¸et’s syndrome, Sjo¨ gren syndrome,
sarcoidosis
Retinitis or retinal
lesions
Cytomegalovirus, Histoplasma capsulatum,
Treponema pallidum
Ear and
nasal
sinuses
Lesions in ear canal or
nose; tender sinusitis
of frontal, sphenoid,
or mastoid sinuses
Chronic bacterial infections or fungal
infections with Aspergillus species, or
mucormycosis, Wegner granulomatosis
Mouth Lip or mouth ulcers Behc¸et’s syndrome, Vogt-Koyanagi-Harada
syndrome, Histoplasma capsulatum
Tongue lesions Candida species
Heart Heart murmur Infectious endocarditis, atrial myxoma
Cardiomegaly Trypanosoma cruzi
Lungs Cough, rales,
hemoptysis
Mycobacterium tuberculosis, Coccidioides
immitis, Histoplasma capsulatum,
Cryptococcus neoformans, Blastomyces
dermatitidis, Paracoccidioides. brasiliensis,
Paragonimus westermani, Nocardia
asteroides, neurosarcoidosis, lung tumor,
vasculitis such as Wegner granulomatosis
Abdomen Gastrointestinal tract Tropheryma whippelii, Strongyloides
stercoralis
Hepatomegaly Trypanosoma brucei species, systemic cancer
Splenomegaly Trypanosoma brucei species
Muscle Localized pain or
swelling
Trichinella spiralis, Taenia solium
cysticercus, systemic vasculitis
Genitalia Lesions on genitalia Herpes simplex type 2, Behc¸et’s syndrome
Joints Joint swelling,
redness, pain
Coccidioides immitis, Brucella species,
Borrelia burgdorferi, rheumatoid arthritis
Skin Rash Borrelia burgdorferi, varicella-zoster,
vasculitis, drug reaction, collagen vascular
disease
Focal lesion or nodule Sporothrix schenckii, Coccidioides immitis
Lymph
nodes
Adenopathy Brucella species, neurosarcoidosis, systemic
cancer
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
10. histological examination. It is not
infrequent that the final diagnosis of
chronic meningitis comes from identi-
fication of the infection at another
body site (Case 2-1). The lungs, joints,
and skin are particularly important
areas to examine. Any identified un-
usual skin lesion or nodule should be
biopsied. Swollen, warm joints should
be x-rayed and aspirated. Patients with
pulmonary illness should undergo
diagnostic bronchoscopy or even nee-
dle biopsy of focal lesions.
NEUROLOGICAL EXAMINATION
Many, but not all, patients with chronic
meningitis will have a stiff neck of
varying severity. Meningeal signs are
less prominent in patients with mild
meningeal inflammation and lower
CSF pleocytosis. Typically, early in
the clinical course, patients will lack
focal neurological signs. However,
when present, specific focal signs may
suggest certain etiologies (Table 2-6).
Cranial nerve palsies usually develop
from a basilar meningeal exudate
entrapping the cranial nerve or pro-
ducing vasculitis and ischemia to the
nerve’s blood supply. The sixth cranial
nerve is most often involved, followed
by cranial nerves VII, II, III, and IV. A
lateral rectus palsy may also signal
obstructive hydrocephalus with in-
creased intracranial pressure. Basilar
meningeal exudate or arachnoiditis
implies more intense localized inflam-
mation often seen in tubercular, Lyme,
fungal, and parasitic meningitis; neuro-
sarcoidosis; hypertrophic pachymenin-
gitis; neoplastic meningitis; and some
forms of CNS vasculitis. Viral meningi-
tis and chemical- or drug-induced
meningitis seldom cause cranial nerve
palsies.
Focal neurological signs such as
hemiparesis, aphasia, or visual field
defects often point to damage to
one or more areas of the cerebral
cortex. The cerebral damage may de-
velop from: (1) CNS masses such as
tuberculomas, brain abscesses, or neo-
plasms; (2) ischemic infarctions sec-
ondary to vasculitis and inflammation
of meningeal vessels; or (3) intracra-
nial hemorrhage from vessel rup-
ture secondary to mycotic or vasculitic
aneurysms.
Ophthalmological examination may
demonstrate papilledema, implying
marked increase in intracranial pres-
sure. The papilledema may stem from
intracranial masses such as a tumor,
abscesses, strokes, intracranial or ex-
tracranial hemorrhages, or obstructive
hydrocephalus. If papilledema is pres-
ent, the lumbar puncture should be
delayed until neuroimaging is ob-
tained to determine the risk of brain
herniation following the lumbar punc-
ture. If retinitis or focal retinal lesions
are seen on funduscopic examination,
the risk of disseminated Cytomegalo-
virus or histoplasmosis is increased
(Table 2-5). The presence of iritis or
uveitis is suggestive of Behc¸et’s dis-
ease, sarcoidosis, syphilis, or Sjo¨gren
syndrome. Poliosis (whitening of eye-
brows and eyelashes with vitiligo)
suggests Vogt-Koyanagi-Harada syn-
drome. Muscle pain and localized
muscle edema suggest trichinosis,
cysticercosis, or possibly systemic vas-
culitis.
CEREBROSPINAL FLUID AND
BLOOD EXAMINATIONS
CSF examination is key to establishing
the diagnosis of chronic meningitis
and to determining its etiology. One
should expect to find a pleocytosis,
elevated protein level, and often de-
pressed glucose level in CSF. The CSF
pleocytosis most often is lymphocytic
but at times may have a predominance
of neutrophils or greater than 10%
eosinophils (Table 2-2). Unfortunately,
simple CSF tests seldom yield the
etiology, and more complex tests must
be ordered.
36
KEY POINTS:
A It is not
infrequent that
the final
diagnosis of
chronic
meningitis
comes from
identification of
the infection at
another body
site.
A Basilar meningeal
exudate or
arachnoiditis
implies more
intense
localized
inflammation
often seen in
tubercular,
Lyme, fungal,
and parasitic
meningitis;
neurosarcoidosis;
hypertrophic
pachymeningitis;
neoplastic
meningitis; and
some forms of
CNS vasculitis.
A CSF examination
is key to
establishing the
diagnosis of
chronic
meningitis and
to determining
its etiology.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
11. 37
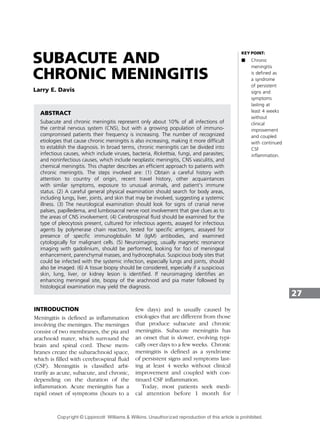
Case 2-1
A 52-year-old Native American man from rural New Mexico presents
with a 3-week history of progressive fevers, headaches, confusion, and
lethargy. He has non–insulin-dependent diabetes mellitus. A grandmother
previously had pulmonary tuberculosis. He has never traveled outside of
New Mexico and Arizona. His temperature is 39.88
C. He is lethargic with a
stiff neck, bilateral leg spasticity, hyperactive deep tendon reflexes, Babinski
signs, and a mild distal sensory neuropathy. A small nodular skin lesion is
noted over his right forearm, which is biopsied for histological examination.
A T1-weighted magnetic resonance imaging (MRI) scan with gadolinium
(Figure 2-1) is interpreted as showing meningeal enhancement and
obstructive hydrocephalus, and a ventriculoperitoneal shunt is placed.
Ventricular CSF
demonstrates 44
WBC/mm3
(60%
lymphocytes and
40% neutrophils),
70 mg/dL protein
and 40 mg/dL
glucose. Blood
glucose is 180
mg/dL. Gram’s stain
and acid-fast CSF
sediment stain
are negative.
CSF cultures for
M. tuberculosis,
fungi, and bacteria
are undertaken.
CSF is sent for
Cryptococcus neo-
formans antigen,
Coccidioides immitis antibody, M. tuberculosis PCR assay, and cytological
examination. Serum is sent for Echinococcus, Leptospira, and Brucella
antibodies.
A clinical diagnosis of tuberculous meningitis is made, and
antituberculosis therapy is started. Corticosteroids are not given because of
his diabetes mellitus. Over the next 4 days the patient worsens. He becomes
obtunded and paraparetic with leg strength 2/5 by muscle testing using
the Medical Research Council scale. Repeat MRI scan demonstrates that the
ventricles have not enlarged.
On the fourth day, the skin biopsy demonstrates spherules consistent
with C. immitis (Figure 2-2). On the fifth day the CSF C. immitis complement
fixation titer returns at 1:16. The CSF M. tuberculosis PCR assay is negative,
as are all other tests. Weeks later, CSF cultures for C. immitis and
M. tuberculosis are reported as sterile.
A confirmed diagnosis of coccidioidal meningitis is made. The patient
is given amphotericin B intravenously and intrathecally for 6 weeks and
then oral fluconazole 800 mL/d. Over several months his leg strength
returns, his mentation improves to near normal, and he returns
home on lifelong oral fluconazole at 400 mg/d.
continued on page 38
FIGURE 2-1 T1-weighted magnetic resonance imaging
scan with gadolinium demonstrating
meningeal enhancement and hydrocephalus
in patient with coccidioidal meningitis.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
12. Isolation or identification of an in-
fectious organism from CSF establishes
the diagnosis. While straightforward in
principle, in practice many infectious
organisms are difficult to culture for
several reasons. (1) The organism may
be present in CSF in low numbers. In
one US study of patients with tubercu-
lous meningitis, the mean colony
count for the patients in whom the
organism was cultured was only 6
colonies per total CSF sample (Davis
et al, 1993). This number contrasts
with colony counts of 105
to 107
per mL
typically seen in acute bacterial men-
ingitis. Low numbers of CSF organisms
are also common for many fungal,
rickettsial, parasitic, and viral infec-
tions. In addition, many organisms are
bound to meninges within granulomas
or exudates or within meningeal cells
and are not free to circulate within the
CSF. This is particularly true in tuber-
culous and fungal meningitis.
(2) Many opportunistic infectious
organisms are fastidious and difficult
to isolate in standard culture media.
For example, Borrelia burgdorferi
(Lyme disease), Rickettsia, and Ehrli-
chia require special culture media that
are seldom available in the standard
microbiology laboratory. Since some
bacteria require up to 15 days of
incubation before growth is detected,
it is important to communicate with
the microbiology laboratory so they
can hold the cultures longer before
discarding. Finally, some fastidious
organisms may degenerate during the
time from lumbar puncture to pro-
cessing by the microbiology laborato-
ry, especially if the CSF is refrigerated.
If amebic meningoencephalitis is con-
sidered, a wet preparation of fresh CSF
may demonstrate mobile ameba,
which is important diagnostically since
culture of ameba is difficult.
Because of these difficulties, in-
creasingly the diagnosis is being ascer-
tained by identification of specific
nucleic acid or proteins within the CSF
that identify the infectious organism.
38
Continued from page 37
Comment. The clinical presentation of a
Native American with known childhood
exposure to pulmonary tuberculosis plus
the presence of intense meningitis with
obstructive hydrocephalus is highly
suspicious for tuberculous meningitis and
drove the decision to begin treatment
rapidly with antituberculous drugs.
However, it is important that other causes
of a high-grade meningitis also be sought.
In this case, the correct diagnosis came
from characteristic spherules seen on
the skin biopsy and a positive CSF
complement-fixing (this is an older antibody
test that detects both immunoglobulin M
(IgM) and immunoglobulin G (IgG)
antibodies) antibody test for C. immitis.
Since the patient lives in an area endemic
for Coccidioides infections, coccidioidal
meningitis was also high on the
differential. Because the patient lives on a ranch that had sheep, goats, and pigs, zoonotic diagnoses
of chronic meningitis (brucellosis, leptospirosis, and echinococcosis) were also considered.
FIGURE 2-2 Skin biopsy of skin nodule demonstrating
small granuloma on hematoxylin and eosin
stain (left) and spherules characteristic of
Coccidioides immitis seen on silver
stain (right).
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
13. PCR assays of CSF are becoming
available for an increasing number of
infectious agents. Unfortunately, they
still are not obtainable for many
uncommon or opportunistic infectious
agents, and PCR assays for many
tropical infectious agents and fungi
often are available only in research
laboratories. The sensitivity of PCR
assays is variable. CSF-PCR assays for
herpes simplex and enterovirus have
become the standard method for
diagnosing these viruses because of
their high sensitivity and specificity.
However, most recent studies evaluat-
ing the M. tuberculosis PCR assay to
diagnose tubercular meningitis have
reported its sensitivity to be no better
than the method of CSF culture (Pai
et al, 2003).
A note of caution is also needed
regarding interpretation of multiplex
PCR viral assays (single PCR assay that
can detect multiple different viruses)
on CSF. It has been discovered recent-
ly that patients with acute meningitis
may have a second virus, usually be-
longing to the herpes family, detected
in CSF. This second virus appears to
have nothing to do with the acute
clinical illness (Davies et al, 2005).
Because the herpes family of vi-
ruses may become latent in neurons
and possibly other cells, latent viruses
may potentially break latency during
acute CNS illnesses and be present
39
TABLE 2-6 Presenting Neurological Symptoms and Signs in
Chronic Meningitis
Frequency Symptoms Signs
Common Headaches Low-grade fevers
Lethargy Weight loss
Malaise Intermittent vomiting
Confusion Obtundation
Nausea Meningismus
Neck stiffness
Less common Delirium Stupor
Blurred vision Cranial nerve palsies
Radicular pain and
paresthesias
Papilledema
Seizures
Hemiparesis
Aphasia
Loss of vision in one eye
Visual field defects
Uveitis, iritis, retinitis
Leg weakness
Bladder and bowel dysfunction
Babinski sign
Coma
KEY POINT:
A Because of
difficulties in
culturing the
infectious
agent,
increasingly the
diagnosis is
being
ascertained by
identification of
specific nucleic
acid or proteins
within the CSF
that identify the
infectious
organism.
Polymerase
chain reaction
assays of CSF
are becoming
available for an
increasing
number of
infectious
agents.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
14. asymptomatically in CSF. This appears
to be of particular concern for the
Epstein-Barr virus, especially if the
patient is immunosuppressed (Weinberg
et al, 2005). It is predicted that similar
relapses of latent viruses may occur
in chronic meningitis. Thus, while PCR
is a powerful tool to detect minute
amounts of infectious agent nucleic
acid, a need still exists to improve the
methodology, better understand the
assay’s limitations, and make assays for
less common infectious agents more
widely available.
The detection of serum IgM
antibody against an infectious organ-
ism often establishes a recent infec-
tion. Detection of the same IgM
antibody in CSF usually means the
meningitis is due to that agent. The
basis for this observation is that IgM is
such a large molecule that it poorly
crosses the blood-CSF barrier, even
when the meningitis partially breaks
the barrier. Thus, the presence of IgM
antibody to a specific infectious agent
implies that immune B and plasma
cells have migrated from blood into
the meninges in response to recogni-
tion of foreign antigen and are pro-
ducing IgM antibody locally. Thus,
identification of IgM antibody to C.
immitis in CSF has become the
standard method of diagnosing cocci-
dioidal meningitis (Smith et al, 1956).
Table 2-7 lists helpful serological tests
that can be performed in CSF or
serum. Approximately 1 mL of CSF or
serum is needed for each serological
test ordered.
The incidence of leptomeningeal
metastasis as a cause of chronic
meningitis is increasing, particularly
in the elderly. The diagnosis is usually
made by cytological examination of
10 mL to 20 mL of fresh CSF. It is wise
to notify the cytological laboratory be-
fore collecting the CSF so the neces-
sary equipment can be set up and the
CSF can be processed promptly for
preservation of maximal histological
cellular detail. Flow cytometry can
be performed on CSF when leukemic
or lymphomatous meningitis is sus-
pected and may be more sensitive
than conventional cytology.
OTHER LABORATORY TESTS
A variety of serological tests are avail-
able to help make the diagnosis of
unusual infectious agents (Table 2-7).
If the serum test is mildly positive or
equivocal, the serological test can be
repeated on CSF to increase specificity.
Serum tests also are available to
help establish noninfectious causes
(Table 2-7).
NEUROIMAGING
Information gained from cranial CT
with contrast or MRI with gadolinium
may help establish the etiology of
chronic meningitis (Zimmerman et al,
2004). MRI appears to be the more sen-
sitive test. Meningeal enhancement,
particularly of the basal meninges,
suggests an intense meningitis as com-
monly seen in tuberculous or fungal
meningitis. Hydrocephalus suggests
that the meningitis has obstructed
CSF pathways at outlets of the fourth
ventricle (foramina of Magendie and
Luschka), at tentorial incisura, around
the sylvian fissures, at the arachnoid
granulations over the convexity of the
brain, or at the aqueduct of Sylvius.
Blockage of ventricular pathways can
be due to tumor or cysts such as ven-
tricular cysticercosis. The hydrocepha-
lusmaybesevereenoughtonecessitate
ventricular shunting to prevent brain
herniation. Focal areas of meningeal
enhancement often suggest granulo-
mas (as in fungal or tuberculous menin-
gitis), hypertrophic pachymeningitis,
neurosarcoidosis, or deposits of lepto-
meningeal metastasis (DeAngelis and
Boutros, 2005; Zimmerman et al, 2004).
40
KEY POINTS:
A The detection of
serum IgM
antibody
against an
infectious
organism often
establishes a
recent
infection, and
detection of the
same IgM
antibody in CSF
usually means
the meningitis
is due to that
agent.
A Information
gained from
cranial
computed
tomography
with contrast or
magnetic
resonance
imaging with
gadolinium
may help
establish the
etiology of
chronic
meningitis.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
15. 41
TABLE 2-7 Helpful Blood and Cerebrospinal Fluid Laboratory Tests in Chronic
Meningitis
Disease Category
Infectious Agent
or Diagnosis Comment
Infectious agents
Antibody tests Bartonella species IgM serum antibody supports recent infection
Borrelia burgdorferi Serological tests difficult to interpret in late
Lyme disease
Brucella species IgG and IgM serum antibody is most sensitive
and specific, but agglutination test is widely
available
Leptospira species IgM serum antibody suggests recent infection
Francisella tularensis High serum antibody titer suggests active
infection, but test may cross-react with
brucellosis
Treponema pallidum CSF Venereal Disease Research Laboratory
(VDRL) is specific but not highly sensitive
Coxiella burnetii Serum antibodies to phase II predominate in
acute disease and those to phase I in chronic
disease
Babesia species IgM serum antibody supports recent infection
Ehrlichia chaffeensis High serum IgG titer or fourfold increase in
titer supportive of recent infection
Rickettsia rickettsii IgM serum antibody supports recent infection
Rickettsia typhi IgM serum antibody supports recent infection
with typhus fever group
Coccidioides immitis CF or EIA CSF antibody titer is diagnostic
Histoplasma capsulatum High serum titer suggests active infection
Blastomyces dermatitidis High serum antibody titer suggests active
infection, but active disease may not have
antibody. Test may cross-react with
histoplasmosis or coccidioidomycosis
Aspergillus species CF and immunodiffusion of serum
Sporothrix schenckii Antibodies in CSF very helpful
Entamoeba histolytica Elevated IgG antibody supports active infection
Echinococcus granulosis IgG antibodies cross-react with cysticercosis
and schistosomiasis
Strongyloides stercoralis IgG serum antibody supports infection, but test
may cross-react with other parasitic infections
Taenia solium Cysticercosis IgG CSF immunoblot antibody is
diagnostic
continued on next page
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
16. 42
TABLE 2-7 Continued
Disease Category
Infectious Agent
or Diagnosis Comment
Toxocara canis Serum antibody titer confirms infection
Trichinella spiralis Serum antibody confirms recent or prior
infection
Antigen tests Cryptococcus neoformans Latex agglutination and EIA of CSF is
diagnostic
Histoplasma capsulatum EIA in CSF diagnostic, urine or blood
EIA suggestive
Aspergillus species CSF Platelia aspergillus or galactomannan
antigen EIA suggestive
Candida species Mannan antigen EIA or latex agglutination
of CSF suggestive
Polymerase chain
reaction assays of
cerebrospinal fluid
Enterovirus Sensitive and specific for enteroviruses
except poliovirus
Human immunodeficiency virus Sensitive, specific, and can be quantitated
Herpes simplex Sensitive and specific; types 1 and 2 can
be distinguished
Cytomegalovirus Sensitive and specific
Varicella-zoster Sensitive and specific
Epstein-Barr See note in text for specificity
Borrelia burgdorferi Unknown sensitivity
Mycobacterium tuberculosis About same sensitivity as mycobacterial
culture
Treponema pallidum Not widely available but can be obtained
Tropheryma whippelii Not widely available but can be obtained
E. chaffeensis Not widely available but can be obtained
Collagen vascular
disease and vasculitis
Rheumatoid arthritis Strongly positive serum rheumatoid factor
suggestive
Sjo¨ gren syndrome Serum Sjo¨ gren syndrome antigens A and
B suggestive
Sarcoidosis Serum angiotensin-converting enzyme level
suggestive of systemic sarcoidosis
Systemic lupus erythematosus Serum high titer antinuclear antibody test
suggestive of systemic lupus erythematosus
Wegener granulomatosis Serum antineutrophil cytoplasmic antibody
helpful
IgM = immunoglobulin M; IgG = immunoglobulin G; CSF = cerebrospinal fluid; PCR = polymerase chain reaction; CF =
complement fixation; EIA = enzyme immune assay (also known as ELISA).
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
17. Identification of parenchymal masses
is helpful as their characteristics may
suggest neurocysticercosis with both
parenchymal and meningeal cysts,
tuberculoma, primary or metastatic
cancer, or abscess. Subarachnoid blood
or intracerebral hemorrhage may be
due to ruptured mycotic and vasculitic
aneurysms or to infectious agents that
destroy blood vessel walls (as in asper-
gillosis or mucormycosis). Cerebral in-
farctions suggest occlusion of cerebral
arteries from meningeal or cerebral
vasculitis or from emboli. Sites of para-
meningealinfectioninsinuses,mastoid,
sella,calvarium,epiduralspace,subdur-
al space, or vertebrae may be identified.
Cerebral arteriography or magnetic
resonance angiography (MRA) may
detect evidence of vasculitis, aneu-
rysms, or occlusions, suggesting vas-
culitis or fungal wall invasion as the
cause (Wynne et al, 1997). However, a
negative MRA or cerebral arteriogram
does not completely eliminate vascu-
litis since the inflammatory process
may affect only small cerebral vessels,
which are difficult to identify by neuro-
imaging. Cerebral catheter venography
or magnetic resonance venography may
identify venous thrombosis. Septic ve-
nous thrombosis may be detected by
magnetic resonance venogram.
IMAGING OTHER BODY SITES
Since many causes of chronic meningi-
tis also have systemic involvement,
imaging other involved sites often
yields diagnostic clues. Chest x-ray
and often CT of the chest will yield
evidence of active pulmonary infec-
tion, enlarged lymph nodes, or system-
ic vasculitis. Depending on the history
and examination, one may consider
imaging, including joints, long bones,
pelvis, and abdomen. Sites of infection
identified outside the brain can be
biopsied for culture and histological
examination and may yield the etiology
of the chronic meningitis.
BRAIN BIOPSY
At times, a meningeal biopsy is re-
quired to establish the diagnosis. The
yield of the biopsy is up to 80% if the
MRI scan with gadolinium demon-
strates focal areas of meningeal en-
hancement but is only 10% if no MRI
enhancement is seen (Cheng et al,
1994). The biopsy may be performed
either openly or stereotaxically, de-
pending on circumstances. The yield
of the biopsy is slightly higher when
taken from the posterior fossa than
from the cerebral cortex. When possi-
ble, the biopsy should include both the
meninges and underlying brain. Com-
mon diagnoses from biopsies include
neurosarcoidosis, hypertrophic pachy-
meningitis, leptomeningeal metastasis,
vasculitis, and infections with agents
such as Candida, Aspergillus, Zygomy-
cetes, and Acanthamoeba. Occasion-
ally M. tuberculosis, Histoplasma cap-
sulatum, Blastomyces dermatitidis or
C. immitis organisms are seen. De-
pending on the clinical suspicions, part
of the biopsy should not be fixed in
formalin but should be cultured or
assayed by PCR for fungi, tuberculosis,
and uncommon bacteria. The major
portion of the biopsy should be fixed
and processed for histological staining
that includes special stains for myco-
bacteria and fungi.
MAJOR CAUSES OF CHRONIC
MENINGITIS
Tuberculous Meningitis
It is estimated that about one third
of the world’s population has been
infected with M. tuberculosis. Al-
though the incidence of tuberculous
meningitis is unknown, the world esti-
mate is up to 70,000 cases per year.
Studies of chronic meningitis from de-
veloping countries always list tubercu-
lous meningitis as the most prevalent.
In the United States, it has become a
less common cause with the majority of
43
KEY POINTS:
A Since many
causes of
chronic
meningitis also
have systemic
involvement,
imaging other
involved sites
often yields
diagnostic
clues.
A The diagnostic
yield of a brain
biopsy is up to
80% if the MRI
scan with
gadolinium
demonstrates
focal areas of
meningeal
enhancement
but is only 10%
if no MRI
enhancement is
seen.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
18. cases occurring in adults who devel-
oped a pulmonary infection decades
earlier in life (Davis et al, 1993).
Individuals who are debilitated or are
immunosuppressed as in acquired im-
munodeficiency syndrome (AIDS) are
also at a higher risk. Establishing the
diagnosis is often difficult since a
history of prior active pulmonary tu-
berculosis is unusual as is a history of
recent exposure to individuals with
active pulmonary tuberculosis (Davis,
2000; Thwaites and Tran, 2005). More
than half of the patients will have an
active infection with M. tuberculosis
only in the meninges without an active
pulmonary infection. The chest x-ray
may show old Ghon complexes (calci-
fied mediastinal lymph nodes) but
seldom has pulmonary infiltrates. A
tuberculin skin test is positive in only
half of the patients. The CSF shows
the classic findings of chronic men-
ingitis but lacks unique features in
the cell count or protein changes.
Table 2-8 gives some suggestions for
improving the success of M. tuberculosis
isolation in CSF. Table 2-9 demonstrates
the CSF diagnostic tests available for the
diagnosis of tuberculous meningitis and
their sensitivity. As noted earlier, a CSF-
PCR assay is available, but its sensitivity
is no higher than mycobacterial culture of
a large-volume CSF. A recent meta-
analysis calculated the sensitivity of the
commercial CSF M. tuberculosis PCR
assays to be 56%, but the specificity was
98% (Paietal,2003).Thevalueofapositive
PCRassayisthatthediagnosiscanbemade
within a few days instead of waiting for up
to 3 to 6 weeks for mycobacterial cultures
to turn positive.
Unfortunately, a positive CSF-PCR
assay does not give any information
about antibiotic sensitivity. We have
now entered the period where many
cases of pulmonary tuberculosis have
some antibiotic resistance. While it is
still unusual for M. tuberculosis iso-
lated from CSF to possess antibiotic
resistance (because the initial infec-
tion occurred decades earlier), CSF iso-
lates showing resistance are appearing
(Thwaites and Tran, 2005). Accordingly,
the need to isolate the CSF organism
and determine its sensitivity pattern is
becoming more important in order to
direct appropriate treatment.
A newly US Food and Drug
Administration–approved test (Quanti-
FERON1
-TB Gold) detects the re-
lease of interferon gamma in fresh
heparinized whole blood from sensi-
tized persons when it is incubated
with mixtures of synthetic peptides
representing two proteins present in
M. tuberculosis: early secretory anti-
gen target 6 (ESAT-6) and culture
filtrate protein 10 (CFP-10) (Mazurek
et al, 2005; Pai et al, 2004). Presently,
information regarding its role in the
diagnosis of tuberculous meningitis is
insufficient, but the test appears
more sensitive for prediction of
active tuberculosis than the tubercu-
lin skin test.
In summary, this author recom-
mends three high-volume lumbar
punctures be performed followed by
high-speed centrifugation of the CSF.
Most of the sediment should be cul-
tured for M. tuberculosis and other
fungi and bacteria as indicated. Be-
cause acid-fast staining of the sediment
has such a low yield, it is preferable
to send that portion of sediment for
M. tuberculosis PCR assay.
Fungi
Although CNS fungal infections remain
uncommon, their incidence has in-
creased primarily due to increased
prevalence of immunosuppression from
AIDS or following organ transplants,
corticosteroids, and chemotherapy.
Most of the more than 100,000 species
of fungi are nonpathogenic for healthy
humans or cause only a short-lived
infection. Only a handful regularly
causes CNS infections (Perfect, 2004).
44
KEY POINTS:
A In tuberculous
meningitis,
more than half
of the patients
will have an
active
infection with
Mycobacterium
tuberculosis
only in the
meninges
without an
active
pulmonary
infection.
A Although CNS
fungal
infections
remain an
uncommon
cause of
chronic
meningitis,
their incidence
has increased
primarily due to
increased
prevalence of
immuno-
suppression
from AIDS or
following organ
transplants,
corticosteroids,
and
chemotherapy.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
19. CNS fungal infections usually result
from a systemic fungal infection else-
where in the body, leading to a
fungemia that successfully invades
the meninges or brain parenchyma.
Most pathogenic fungi cause meningi-
tis, but some fungi cause meningoen-
cephalitis (meningitis with microab-
scesses) or localized brain abscesses.
The family Mucoraceae of Zygomycetes
species, Aspergillus species, and Can-
dida species invade cerebral blood
vessels, causing an arteritis that may
thrombose or rarely rupture.
Primary fungal pathogens are fun-
gi that occasionally cause disease
in healthy individuals. The most com-
mon primary pathogen, C. neofor-
mans, accounts for more than half
of all CNS fungal meningitis (Bicanic
and Harrison, 2004). Other important
primary pathogens include C. immitis
(Davis and Porter, 2005), H. capsu-
latum (Wheat et al, 2000), and B.
dermatitidis (Friedman et al, 2000).
In the setting of immunosuppression,
the incidence of primary CNS fungal
infections is markedly increased.
Secondary fungal pathogens are
opportunistic fungi that cause CNS
infection in the setting of obvious
immune dysfunction or anatomic ab-
normalities. Major secondary patho-
gens include Aspergillus species,
Zygomycetes species (mucormycosis)
and Candida species, but numerous
other species cause CNS infections in
rare instances.
Establishing the diagnosis of a CNS
fungal infection is difficult as the
clinical course, CSF findings, and
neuroimaging results for fungal men-
ingitis do not differ markedly from
many other causes of chronic menin-
45
TABLE 2-8 Optimizing Successful Isolation of Mycobacterium
Tuberculosis from Cerebrospinal Fluid
" Remove 20 mL to 40 mL of CSF from lumbar space.
Low colony counts in CSF require culture of large volumes of CSF. Removal
of greater than 30 mL of CSF should also remove CSF along base of brain
stem that has highest concentration of organisms.
" Concentrate organisms in CSF pellet.
Mycobacterium tuberculosis has high lipid concentration in the cell wall and
does not pellet easily with standard centrifugation as buoyant density is
close to that of CSF. High-speed centrifugation at 3000 times gravity for
30 minutes is needed. The bottom few mL should be used for culture and
polymerase chain reaction assay. This method may be considered for all
fungal cultures as well.
" When possible, culture concentrated CSF in special liquid media designed
for M. tuberculosis.
Incubation time to detect growth is shorter when using liquid media, such
as Bactec1
media, than when using solid media.
" Repeat large-volume lumbar puncture 2 times.
Mycobacteria can be cultured from CSF for up to 1 week after
antituberculosis therapy has been started. Three lumbar punctures increase
the isolation rate to 50% to 80%.
CSF = cerebrospinal fluid.
From Davis LE. Tuberculous meningitis. In: Davis LE, Kennedy PGE, eds. Infectious diseases of the nervous system.
Oxford: Butterworth-Heinemann, 2000:481–498. Modified with permission from Elsevier.
KEY POINT:
A Cryptococcus
neoformans
accounts for
more than half
of all CNS
fungal
meningitis.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
20. gitis. If CSF neutrophils predominate,
the risk of infection with Blastomyces,
Aspergillus, Zygomycetes, and others
increases (Table 2-2). If CSF eosino-
phils are present, the possibility of
coccidioidal meningitis increases. Fun-
gi are difficult to isolate or identify in
CSF. Culturing the fungus from CSF
occurs only 50% of the time for C.
immitis and H. capsulatum, 10% for
Candida, and less than 5% for Asper-
gillus and Zygomycetes. Cryptococcal
meningitis is the exception with C.
neoformans isolated from CSF more
than 75% of the time. CSF-PCR assays
for fungal nucleic acid currently are
neither particularly sensitive nor widely
available. Accordingly, the clinician
must utilize multiple strategies to
establish the diagnosis. As with other
causes of chronic meningitis, one
important approach is to search for
evidence of infection elsewhere in the
body. Common extrapulmonary sites
of fungal infection include skin, bone,
bone marrow, joints, sinuses, liver,
and genitourinary system. Identifica-
tion of the organism from one of these
other sites greatly improves the prob-
ability that the CNS infection is from
the same organism (Case 2-1). An
important exception to this rule is that
isolation of Candida from blood
rarely indicates a CNS infection. The
diagnosis of CNS Candida infection
usually requires direct evidence of the
fungus in CSF, meninges, or brain
(Pappas et al, 2004). A number of
fungal antibody and antigen tests
are available that may establish the
diagnosis (eg, C. neoformans and
C. immitis) or suggest a systemic
fungal infection (Table 2-7). The C.
neoformans antigen test of CSF has a
high sensitivity and specificity but
occasionally may be negative in immu-
nocompromised patients with very
low levels of CSF infection. In addi-
tion, in patients who are immunocom-
promised, antibody tests may not
always be positive.
OTHER CHRONIC MENINGEAL
INFECTIOUS AGENTS
Neurosyphilis occasionally presents
as low-grade chronic meningitis, par-
ticularly in secondary syphilis and in
the meningovascular phase of tertiary
syphilis (Holmes et al, 1984). Patients
may experience chronic headaches,
46
TABLE 2-9 Cerebrospinal Fluid Diagnostic Tests Available for
Mycobacterium Tuberculosis
Test
Sensitivity (Range of
Positive Tests)
Acid-fast staining of bacteria in sediment 5% to 25%
Tuberculostearic acid (not widely available) 50% to 75%
Mycobacterium tuberculosis isolation from
routine single lumbar puncture
20% to 40%
M. tuberculosis isolation from 3 high-volume
lumbar punctures
50% to 80%
Polymerase chain reaction assay detection of
M. tuberculosis nucleic acid
50% to 75%
Detection of antibody to M. tuberculosis 55%
From Davis LE. Tuberculous meningitis. In: Davis LE, Kennedy PGE, eds. Infectious diseases of the nervous system.
Oxford: Butterworth-Heinemann, 2000:481–498. Modified with permission from Elsevier.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
21. mild meningismus, and occasional
cranial nerve palsies and/or ischemic
strokes from a meningeal vasculitis. In
patients infected with HIV, uveitis or
iritis due to syphilis commonly accom-
panies the meningitis. A reactive CSF-
Venereal Disease Research Laboratory
(VDRL) test is the gold standard.
Unlike the serum rapid plasma reagin
test, false-positive tests are rare. How-
ever, the CSF-VDRL test may be absent
in early secondary syphilitic meningi-
tis. In this setting, the diagnosis is
made by a reactive serum syphilis
serological test plus a CSF lymphocytic
pleocytosis.
B. burgdorferi infection of the
meninges should also be considered
in patients living or traveling to
endemic areas. This spirochete com-
monly infects the heart, joints, and
nervous system. Typically, there is a
chronic lymphocytic meningitis that
may be accompanied by a facial palsy
or occasionally a painful neuritis.
Rarely, an encephalomyelitis develops.
The most sensitive diagnostic test is
demonstration of intrathecal produc-
tion of anti–B. burgdorferi antibody
(Halperin, 1998).
Viruses are a rare cause of chronic
meningitis, except for HIV. HIV often
causes a persistent meningitis, which
may be asymptomatic or cause chronic
headache (Marra, 2004). The CSF often
shows a low-grade lymphocytic pleocy-
tosis with normal or minimally elevated
protein. Neuroimaging is usually nor-
mal unless other opportunistic CNS
infections are also present. An HIV-PCR
assay usually is positive. Anti-HIV thera-
py may eliminate the meningitis.
In immunosuppressed individuals,
varicella-zoster virus can infect both
oligodendroglia and cells of cerebral
blood vessels causing a CNS chronic
meningovasculitis (Gilden et al, 2000).
The brain infection may, or may not,
be preceded by an episode of shingles.
Neuroimaging usually shows multiple
focal areas of white matter demyelin-
ation and brain infarctions. CSF pleo-
cytosis is common, and the varicella-
zoster CSF-PCR assay is positive.
Enteroviruses frequently cause acute
viral meningitis but rarely cause a per-
sistent CSF infection unless the pa-
tient has agammaglobulinemia or hypo-
gammaglobulinemia (McKinney et al,
1987). Diagnosis is made by detection
of enterovirus RNA in CSF by PCR.
Rickettsia may cause prolonged
meningitis, especially from Ehrlichia
chaffeensis (human monocytic ehrli-
chiosis), Anaplasma phagocytophilum
(human granulocytic ehrlichiosis) and
Babesia species (Davis, 2000). These
infectious agents are transmitted to
humans following a bite of an infected
tick. Meningeal signs occur in about
10% of infections. Human monocytic
ehrlichiosis is the most common with
the majority of cases occurring in the
southeastern and south central states
(especially Oklahoma, Missouri, Arkan-
sas, and Texas). Rickettsia infections
are often not diagnosed because they
are seldom considered in the differen-
tial diagnosis. Residence in endemic
areas and exposure to ticks should
raise suspicion. The diagnosis for most
Rickettsia is usually made through an
indirect serum immunofluorescent an-
tibody test showing either a single
high titer or a fourfold rise in antibody
titer between acute and convalescent
blood samples (Table 2-7).
Meningeal parasitic infections are
rare except for cysticercosis. Neuro-
cysticercosis is common in Mexico,
Central America, and South America,
and most cases seen in the United
States are found in individuals who
have emigrated from these countries
(Davis, 2005). Neurocysticercosis de-
velops from consumption of Taenia
solium ova shed in stools by humans
infected with the mature tapeworm.
After ingestion from contaminated
food or water, the ova develop into
47
KEY POINTS:
A Viruses are a rare
cause of
chronic
meningitis,
except for HIV,
that often
cause a
persistent
meningitis,
which may be
asymptomatic
or cause
chronic
headache.
A Meningeal
parasitic
infections are
rare except for
cysticercosis.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
22. oncospheres, pass through the intes-
tinal wall, and circulate in blood
to lodge preferentially in brain or
meningeal blood vessels. In about
10% of neurocysticercosis, parasites
lodge in the meninges or ventricle
choroid plexus to produce a chronic
meningitis or ventriculitis that can be
severe enough to produce hydroceph-
alus. Diagnosis is usually made by MRI
identification of parenchymal and men-
ingeal cysts, particularly if the scolex is
seen within the cyst wall or by detec-
tion of cysticercosis antibody in CSF. A
positive serum cysticercus antibody is
also helpful, but individuals from
countries with a high prevalence of
cysticercosis may have serum antibody
from a prior infection.
Neurosarcoidosis
Sarcoidosis occurs worldwide with
a peak incidence between 20 and
40 years. In the United States the
prevalence is tenfold higher in blacks.
Neurosarcoidosis develops in about 5%
to 15% of patients with systemic
sarcoidosis and is characterized by
noncaseating (non-necrotic) granulo-
ma in meninges and parenchyma (Gul-
lapalli and Phillips, 2002; Hoitsma et al,
2004). Granulomas are masses of acti-
vated macrophages and associated
epithelioid and giant cells. Neurosar-
coidosis is preceded by or combined
with infections of lung in 70% of
patients, skin in 30%, and lymph nodes
in 25%. However, in up to half the
patients, neurological symptoms may
be part of the initial presentation.
About 75% of patients with neuro-
sarcoidosis develop cranial nerve
palsies (mainly VII, II, IX, X, and
VIII) that are often multiple. Diabetes
insipidus from granuloma in the hypo-
thalamic-pituitary axis also commonly
occurs. The CSF of 80% of patients
shows a mild lymphocytic pleocytosis,
elevated protein, and occasionally mild
hypoglycorrhachia. Since no serologi-
cal test exists, the diagnosis may be
difficult. Eighty percent of patients with
neurosarcoidosis have abnormal chest
x-rays (hilar lymphadenopathy and/or
interstitial infiltrates). Forty percent
of patients have abnormal meningeal
findings on cranial MRI with gado-
linium, including focal areas of basilar
meningeal enhancement and thicken-
ing, and up to 50% have an elevated
CSF angiotensin-converting enzyme
level (Gullapalli and Phillips, 2002).
However, CSF angiotensin-converting
enzyme levels may occasionally be
elevated in other CSF infections. Ele-
vated serum angiotensin-converting
enzyme levels usually reflect active
systemic disease. The diagnosis is
established by identification of non-
caseating granuloma in tissue. Fre-
quently, biopsy of cervical lymph
nodes, lung, or conjunctiva confirms
the diagnosis of sarcoidosis and obvi-
ates the need for a brain biopsy.
Behc¸et’s syndrome and Vogt-
Koyanagi-Harada syndrome are rare
multiorgan granulomatous diseases
that can cause a lymphocytic menin-
goencephalitis and rarely an arach-
noiditis. The CNS manifestations are
not pathognomonic, and the diagnosis
is usually made by recognition of other
systemic features. Behc¸et’s syndrome
is most commonly seen in individuals
from the Middle East and is composed
of a constellation of oral aphthous
ulcers, gastrointestinal and genital ul-
cers, uveitis, iridocyclitis, optic neuri-
tis, keratitis, synovitis, and arthralgias
(Yurdakul et al, 2004). A meningoen-
cephalitis is seen in 10% of patients
but rarely is a presenting manifesta-
tion (Brazis et al, 2004). The CSF
shows a low-grade lymphocytic pleo-
cytosis, slightly elevated protein level,
and normal glucose level. Vogt-
Koyanagi-Harada syndrome, which
is likely an autoimmune disorder,
most commonly occurs in individuals
of Asian descent. The syndrome is
48
KEY POINT:
A Neurosarcoidosis
develops in
about 5% to
15% of
patients with
systemic
sarcoidosis and
is characterized
by noncaseating
(non-necrotic)
granuloma in
meninges and
parenchyma.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
23. characterized by anterior and pos-
terior uveitis, poliosis, alopecia, vitiligo,
and dysacusis (Read et al, 2000). A
meningoencephalitis develops in 60%,
often shortly after the occurrence of
other systemic signs.
Neoplastic Meningitis
Neoplastic meningitis (also called
carcinomatous meningitis, leptome-
ningeal metastases, or lymphomatous
meningitis) is an important category
to consider in patients with chronic
meningitis. About 5% of patients with
extraneural cancer have spread of
malignant cells to the meningeal
space. Even this small percentage
becomes quite relevant because over
1 million cases per year of cancer are
diagnosed in the United States. Most
often the leptomeningeal metastasis
develops late in the cancer course. In
5% to 10% of patients it is the first
clinical manifestation, and in 20% it
may develop after a prolonged disease-
free interval (Chamberlain, 2005).
Cancer cells reach the meninges by
several routes: (1) hematogenous
spread through the venous plexus of
Batson, choroid plexus, or meningeal
arteries; (2) direct extension from
contiguous tumor deposits; (3) inva-
sion along perineural or perivascular
spaces; and (4) following spillage of
malignant cells of a primary brain
tumor into the meninges, especially
after partial surgical resection (Kim and
Glantz, 2001). Once within the meninges,
the cells spread via CSF flow and
gravity. Thus, the most common sites
of pathological involvement are the
base of spine (basilar cisterns or poste-
rior fossa) and the lumbosacral (cauda
equina). Table 2-10 lists the more
common causes and their frequency
of neoplastic meningitis. Although breast
cancer has a low incidence of spread
to the meninges, its high prevalence
49
TABLE 2-10 Cancers That Cause Leptomeningeal Metastases and
Their Frequency
Tumor
Percentage That
Metastasize to
Leptomeninges
Breast 5 to 10
Lung, all types 10 to 25
Small cell at relapse 40
Malignant melanoma 15 to 25
Gastrointestinal 4 to 14
Non-Hodgkin’s lymphoma 5 to 10
Leukemia 30 to 70
Lymphoma 7 to 14
Carcinoma of unknown primary site 1 to 7
Primary brain tumor, especially medulloblastoma,
ependymoma, and cerebellar astrocytoma
1 to 5
Primary central nervous system lymphoma 40
Modified with permission from Demopoulos A. Leptomeningeal metastases. Curr Neurol Neurosci Rep
2004;4:196–204; and Kim L, Glantz MJ. Neoplastic meningitis. Curr Treat Options Oncol 2001;2:517–527.
Copyright # 2001, Current Medicine.
KEY POINT:
A Neoplastic
meningitis
(also called
carcinomatous
meningitis,
leptomeningeal
metastases, or
lymphomatous
meningitis) is
an important
category to
consider in
patients with
chronic
meningitis.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
24. makes the total number of cases consid-
erable. Statistically, the most common
cancer types seen in neoplastic menin-
gitis are breast, lung, melanoma, and
leukemia.
Clinical signs and symptoms depend
on the tumor location and whether the
metastases are causing hydrocephalus
that develops from obstruction of CSF
pathways at the level of the fourth
ventricle, basal cisterns and tentorial
opening, or cerebral convexities. Pos-
terior fossa metastases commonly
cause cranial nerve palsies and ataxia.
Cauda equina metastases cause leg
weakness, radicular pains and pares-
thesias, gait instability, and bladder and
bowel dysfunction. Hydrocephalus
commonly produces headaches, nau-
sea and vomiting, encephalopathy, and
papilledema. Nuchal rigidity is present
in only 15% of cases. Undiagnosed and
untreated, leptomeningeal metastases
rapidly progress, causing more severe
neurological signs and death over
weeks to several months.
Leptomeningeal metastases are of-
ten suspected, but not diagnosed,
by abnormal findings on cranial and
lumbosacral spine neuroimaging. Cra-
nial enhanced CT is abnormal in 25% to
50% of patients, but MRI with gadolin-
ium demonstrates abnormalities in
over 75%. Common cranial MRI abnor-
malities include sulcal enhancement in
57%, ependymal enhancement in 21%,
subarachnoid enhancing nodules in
36%, and communicating hydrocepha-
lus in 7%. An abnormal lumbosacral
MRI is seen in up to 70% of patients
with appropriate leg and bowel symp-
toms and includes thickened nerve
roots in cauda equina, enhancement
of nerve roots, and subarachnoid nod-
ules on spinal cord or roots. It is
suggested that an MRI be performed
before the lumbar puncture as a few
patients develop transient gadolinium
enhancement in the lumbar dura and
meninges after the lumbar puncture
that confuses the picture.
Identification of malignant cells on
cytological examination of CSF or by
meningeal biopsy establishes a firm
diagnosis. The first cytological exami-
nation of CSF may be negative in 50% of
patients. Factors that increase the
chance of finding malignant cells in-
clude high CSF volumes of 20 mL to
30 mL, prompt fixation of the CSF by
notifying the laboratory before the
lumbar puncture is performed, and
obtaining two CSF samples. Use of
monoclonal antibodies for immuno-
histochemical analysis does not sig-
nificantly increase the sensitivity of
cytology alone. However, in cases of
possible leukemia or lymphoma, flow
cytometry using antibodies against
surface markers helps distinguish be-
tween neoplastic and reactive CSF
lymphocytes. Unfortunately, negative
CSF cytology in cases of proven neo-
plastic meningitis ranges from 25%
to 40%.
In patients with a high suspicion
of neoplastic meningitis, but negative
CSF cytology, analysis of biochemical
tumor markers in CSF may occasion-
ally be helpful. Unfortunately, the
sensitivity is not high and specificity
is poor if the patient has high serum
titers of the marker. Common bio-
chemical markers include: carcinoem-
bryonic antigen for adenocarcinoma,
prostate specific antigen (PSA) for
prostate cancer, b2-microglobulin for
lymphoma and leukemia, b-human
chorionic-gonadotropin for choriocar-
cinoma and germ cell tumors, a-
fetoprotein for testicular cancer, and
cancer antigen (CA) 15-3 for breast
cancer (Chamberlain, 2005). In patients
with negative CSF cytology, the diag-
nosis comes more frequently from
biopsy of an MRI- or CT-enhancing
meningeal site with subsequent histo-
logical examination.
50
KEY POINT:
A Identification of
malignant cells
on cytological
examination of
CSF or by
meningeal
biopsy
establishes a
firm diagnosis
of neoplastic
meningitis, but
the first
cytological
examination of
CSF may be
negative in
50% of
patients.
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
25. Vasculitis
Vasculitis means inflammation of blood
vessels with associated structural dam-
age and frequently vascular necrosis. It
may be caused by direct invasion of
blood vessels and perivascular spaces
by infectious organisms, by immuno-
logical responses to drugs and heterolo-
gous proteins, or from an underlying
autoimmune or neoplastic process.
The vascular inflammatory cells then
spill into the CSF, producing the
chronic meningitis. While CNS vascu-
litis is a recognized cause of chronic
meningitis, the percentage of cases due
to vasculitis appears to be low, al-
though precise information is lacking.
CNS vasculitis can be divided into three
subcategories: (1) CNS manifestations
of systemic vasculitis, (2) primary CNS
vasculitis, and (3) CNS vasculitis due to
infectious causes or drugs.
Systemic vasculitis generally begins
elsewhere in the body, and CNS in-
volvement occurs in less than 10% of
cases. Accordingly, imaging (CT, MRI, or
arteriography) is more likely to identify
abnormal arteries and related patholog-
ical changes in lungs, liver, or kidney.
Wegener granulomatosis, a small
vessel systemic granulomatous vasculi-
tis that frequently involves lungs, nasal
passages, paranasal sinuses, and kid-
neys, affects the CNS in 8% of patients
(Nadeau, 2002). CNS involvement pro-
duces ischemic cerebral infarctions,
meningeal thickening, and nonspecific
white matter changes. Meningeal in-
volvement may damage the optic nerve
or chiasm and cause visual loss, cranial
nerve palsies (especially nerves VI, VII,
and VIII), and diabetes insipidus from
pituitary or pituitary stalk destruction.
Granulomatous masses may also ex-
tend from nasal and paranasal sinus
cavities into the orbit affecting extra-
ocular muscles (Younger, 2004). Crani-
al CT may demonstrate bony changes
in the nasal passages, sinuses, or
calvarium and cerebral infarctions
(Schmidt, 2004). MRI is more sensitive
for parenchymal or meningeal changes,
but the changes are nonspecific. Often
the serum antineutrophil cytoplasmic
antibody test is positive.
Polyarteritis nodosa is a systemic
necrotizing arteritis that affects multi-
ple systemic organs. Meningeal vessels
may be damaged and are character-
ized by a neutrophil inflammatory
infiltrate of all three vessel layers,
especially at arterial branch points that
can result in aneurysms (Nadeau,
2002). Resulting clinical deficits may
include cerebral or subarachnoid hem-
orrhage, cranial neuropathies (espe-
cially nerves III and VIII), and ischemic
strokes. Patients typically have elevat-
ed erythrocyte sedimentation rate,
positive antineutrophil cytoplasmic
antibody, and a characteristic vasculitis
on histological examination of tissue.
Primary CNS vasculitis is uncommon
and generally comprises two major
diseases: temporal arteritis (also called
giant cell arteritis) and primary angiitis
of the CNS (also called granulomatous
angiitis of the CNS or isolated angiitis
of the CNS). Although traditionally
considered a primary vasculitis, tem-
poral arteritis is now considered to be
a systemic disease affecting elderly
persons and heralded by a persistent
headache, constitutional symptoms,
and occasionally vision loss. The tem-
poral artery wall is most commonly
invaded by a mixed inflammatory
infiltrate that ultimately becomes gran-
ulomatous. In addition, intracranial
meningeal arteries occasionally be-
come involved, producing chronic
meningitis and associated neurological
signs that include vertigo, deafness,
diplopia, homonymous hemianopia,
and hemiparesis (Caselli et al, 1988).
High-frequency color ultrasonic Dopp-
ler sonography demonstrating abnor-
mal areas of one or both temporal
arteries raises suspicion of the diagno-
sis (Schmidt, 2004). However, the gold
51
KEY POINTS:
A While CNS
vasculitis is a
recognized
cause of
chronic
meningitis, the
percentage of
cases due to
vasculitis
appears to be
low, although
precise
information is
lacking.
A Primary CNS
vasculitis is an
uncommon
cause of
chronic
meningitis and
generally
comprises two
major diseases:
temporal
arteritis (also
called giant cell
arteritis) and
primary angiitis
of the CNS
(also called
granulomatous
angiitis of the
CNS or isolated
angiitis of the
CNS).
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
26. standard is histological examination of
a 1-cm to 2-cm length of a temporal
artery that shows medial wall necrosis,
usually with giant cells.
Primary CNS angiitis is a rare
vasculitis of unknown etiology that
mainly affects small leptomeningeal
and parenchymal vessels (200-mm to
500-mm diameter) without evidence of
systemic disease (West, 2003). The
disease may affect any people of any
age but typically occurs in middle-aged
adults. The onset is usually insidious
over months. Clinical characteristics
are typical for chronic meningitis, but
fever and weight loss are unusual.
About 10% of patients will develop an
intracerebral or subarachnoid hemor-
rhage, and brain mass lesions occa-
sionally develop. No specific laboratory
tests are available. The erythrocyte
sedimentation rate is elevated in only
60% of patients, and liver enzymes are
usually normal. Cranial CT is reported
to be abnormal in 60% of patients and
MRI in 75%. MRI with gadolinium
findings includes multifocal and bilat-
eral gray and white matter lesions
mainly in the cerebral hemispheres
as well as leptomeningeal enhance-
ment. Catheter angiography is abnor-
mal in about 75% of patients and often
demonstrates arterial beading (alter-
nating stenosis and ectasia with or
without aneurysms) and irregular
lumens. If the arteritis is only in small
arterioles, arteriography may be nor-
mal. A meningeal biopsy remains the
gold standard and has a sensitivity of
75% or even higher if arteriography
demonstrates abnormal vessels.
CNS vasculitis can be caused by a
wide variety of infectious causes or
drugs. Infectious agents that are most
prone to cause a CNS vasculitis include
varicella-zoster virus, Cytomegalovirus,
M. tuberculosis, Rickettsia rickettsii,
Treponema pallidum, B. burgdorferi,
Aspergillus species, C. immitis, and H.
capsulatum (Siva, 2001; West, 2003).
CNS vasculitis has been reported in
association with repeated intravenous
or oral exposure to a variety of rec-
reational drugs, including amphet-
amine and related sympathomimetic
agents, cocaine, and heroin (Nadeau,
2002; Siva, 2001). Although rare, CNS
vasculitis has been reported as a para-
neoplastic syndrome in patients with
Hodgkin’s lymphoma, non-Hodgkin’s
lymphoma, and hairy-cell leukemia
(Siva, 2001). CNS necrotizing arteritis
and microvasculitis has rarely been
associated with anti-Hu antibody in
the CSF (Younger, 2004).
GENERAL PRINCIPLES OF
CHRONIC MENINGITIS
MANAGEMENT
Providing detailed instructions on treat-
ments for specific etiologies of chronic
meningitis is beyond the scope of this
chapter. However, when the cause is
not yet established, the problem be-
comes when to treat and with what to
treat. This is a serious problem when the
etiology is infectious because isolation
of the infectious agent often takes
weeks (unless the PCR assay is positive).
In patients with high-grade meningitis
and risk factors for tuberculosis, treat-
ment for tuberculous meningitis is usu-
ally recommended since serious adverse
neurological events develop if the pa-
tient is not promptly and appropriately
treated. As noted above, antitubercu-
lous drugs can be given for several days
without affecting the ability to isolate M.
tuberculosis from CSF. In addition,
other causes of high-grade chronic men-
ingitis should be sought (Table 2-3).
Deciding whether to include cortico-
steroids in the empiric antituberculous
regimen is difficult since patients in
stage II and III tuberculous meningitis
do better when corticosteroids are
added. However, if the chronic men-
ingitis is due to another infectious
organism, addition of corticosteroids
may worsen the CNS infection.
52
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
27. In spite of extensive workup, 15% to
30% of patients have no etiology for the
chronic meningitis discovered. Limited
literature is available to aid in manage-
ment of these patients. In a report of 49
patients with ‘‘idiopathic’’ chronic
meningitis from the Mayo Clinic (Smith
and Aksamit, 1994), 60% had a nonfatal
outcome when followed for a mean of
50 months. In many cases, the menin-
gitis spontaneously resolved and these
patients were classified as having
chronic benign lymphocytic meningi-
tis. Other authors have reported similar
patients who develop a chronic benign
lymphocytic meningitis syndrome (Ell-
ner and Bennett, 1976). Unfortunately,
not all undiagnosed patients had a be-
nign outcome. Eight patients were
subsequently found to have neoplastic
meningitis based on subsequent CSF
cytology or brain biopsy. Two addition-
al patients were later shown to have a
CNS fungal infection. When empirical
corticosteroids were administered to
21 patients, half showed clinical im-
provement during the period of treat-
ment, but corticosteroid admin-
istration showed no improvement in
final outcome when compared with
patients not given such treatment.
Since corticosteroids impair the host
immune response that may be partially
controlling the meningeal infection, it
may be wise to repeat CSF cultures 1 to
3 weeks after the corticosteroids are
started.
Because many causes of chronic
meningitis exist with many factors
affecting the etiology, it is difficult to
create a simple, straightforward algo-
rithm for diagnosis and treatment. In
patients presenting with a rapid pro-
gression of signs and symptoms from
an intense meningitis, one should
consider early empirical treatment. If
the patient has risk factors for tuber-
culosis, antituberculous drugs should
be started. If the patient also has risk
factors for fungal meningitis, one
could add fluconazole. However, it is
essential to continue to search for the
etiology as described earlier.
In summary, this chapter has out-
lined an approach that should be
helpful toward evaluating the patient
with chronic meningitis. In addition,
major diagnostic tests available for the
more common causes of chronic
meningitis have been presented.
REFERENCES
" Anderson NE, Willoughby EW. Chronic meningitis without predisposing
illness—a review of 83 cases. Q J Med 1987;63:283–295.
Authors discuss etiologies of 83 patients with chronic meningitis in New Zealand. Since
many patients were rural tribesmen, tuberculous meningitis was found in 40%.
" Bicanic T, Harrison TS. Cryptococcal meningitis. Br Med Bull 2004;72:99–118.
This article reviews cryptococcal meningitis in both healthy and immunocompromised
patients with respect to clinical presentation, diagnosis, and treatment.
" Brazis PW, Stewart M, Lee AG. The uveo-meningeal syndromes. Neurologist
2004;10:171–184.
Authors review a spectrum of diseases including Behc¸et’s syndrome and Vogt-Koyanagi-
Harada syndrome that cause uveitis along with meningitis.
" Caselli RJ, Hunder GG, Whisnant JP. Neurologic disease in biopsy-proven
giant cell (temporal) arteritis. Neurology 1988;38:352–359.
This article reviews neurological findings in 166 consecutive patients with biopsy-proven
temporal arteritis.
53
KEY POINT:
A In spite of
extensive
workup, 15%
to 30% of
patients have
no etiology for
the chronic
meningitis
discovered.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
28. " Chamberlain MC. Neoplastic meningitis. J Clin Oncol 2005;23:3605–3613.
Author presents broad overview of leptomeningeal metastases including pathogenesis,
clinical features, diagnosis, and treatment options.
" Cheng T, O’Neill BP, Scheithauer BW, Piepgras DG. Chronic meningitis: the
role of meningeal or cortical biopsy. Neurosurgery 1994;34:590–596.
This article discusses the diagnoses made from 37 meningeal biopsies from patients with
chronic meningitis.
" Davies NW, Brown LJ, Gonde J, et al. Factors influencing PCR detection
of viruses in cerebrospinal fluid of patients with suspected CNS infections.
J Neurol Neurosurg Psychiatry 2005;76:82–87.
This recent article using multiplex polymerase chain reaction (PCR) found that 10% of
cerebrospinal fluid (CSF) samples were positive for two or more viruses, and 5% of patients
classified as ‘‘unlikely’’ to have a central nervous system (CNS) viral infection were positive
for a virus. Most of the questionable viruses detected belonged to the herpes family.
" Davis LE. Neurocysticercosis. In: Power C, Johnson RT, eds. Emerging
neurological infections. Boca Raton, Fla: Taylor & Francis, 2005;261–287.
This chapter reviews the clinical, laboratory, neuroimaging, and treatment aspects of
neurocysticercosis, including meningeal and ventricular cysticercosis.
" Davis LE. Tuberculous meningitis. In: Davis LE, Kennedy PGE, eds.
Infectious diseases of the nervous system. Oxford: Butterworth-Heinemann,
2000:481–498.
This chapter reviews the clinical, laboratory, radiological, and management features of
tuberculous meningitis.
" Davis LE, Paddock CD, Childs JE. Ehrlichiosis and the nervous system. In: Davis
LE, Kennedy PGE, eds. Infectious diseases of the nervous system. Oxford:
Butterworth-Heinemann, 2000:499–520.
This chapter provides a comprehensive review of meningitis caused by Ehrlichiosis.
" Davis LE, Porter BS. Central nervous system Coccidioides immitis infections.
Curr Treat Options Neurol 2005;7:157–165.
This article reviews current methods of diagnosis and treatment of coccidioidal meningitis.
" Davis LE, Rastogi KR, Lambert LC, Skipper BJ. Tuberculous meningitis
in the southwest United States: a community-based study. Neurology
1993;43:1775–1778.
This article reviewed all cases of tuberculous meningitis in New Mexico over a 20-year
period. Cases were found in all ages and ethnic backgrounds. Acid-fast staining of CSF
demonstrated bacilli in only 4% of patients because their CSF had low colony counts that
were below detection sensitivity by acid-fast staining.
" DeAngelis LM, Boutros D. Leptomeningeal metastasis. Cancer Invest
2005;23:145–154.
Article discusses leptomeningeal metastases from a clinical, CSF, and neuroimaging
viewpoint with a general review of treatment options.
" Demopoulos A. Leptomeningeal metastases. Curr Neurol Neurosci Rep
2004;4:196–204.
This article reviews incidence, clinical features, neuroimaging, and treatment of neoplastic
meningitis.
54
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
29. " Ellner JJ, Bennett JE. Chronic meningitis. Medicine 1976;55:341–369.
Early classic article describing the major causes of chronic meningitis and helpful
diagnostic approaches.
" Friedman JA, Wijdicks EF, Fulgham JR, Wright AJ. Meningoencephalitis due
to Blastomyces dermatitidis: case report and literature review. Mayo Clin
Proc 2000;75:403–408.
This article reviews current methods of diagnosis and treatment of blastomycotic
meningoencephalitis.
" Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, et al. Neurologic
complications of reactivation of varicella-zoster virus. N Engl J Med
2000;342:635–645.
Authors review the many CNS and peripheral nervous system complications of shingles,
including small vessel meningoencephalitis.
" Gullapalli D, Phillips LH 2nd. Neurologic manifestations of sarcoidosis.
Neurol Clin 2002;20:59–83.
This extensive review covers the clinical features, diagnosis, and therapy of CNS sarcoidosis.
" Halperin JJ. Nervous system Lyme disease. J Neurol Sci 1998;153:182–191.
This article reviews the common CNS infections from Borrelia burgdorferi.
" Hildebrand J, Aoun M. Chronic meningitis: still a diagnostic challenge.
J Neurol 2003;250:653–660.
This is a brief review of major causes of chronic meningitis with useful information on
leptomeningeal metastases.
" Hoitsma E, Fabver CG, Drent M, Sharma OP. Neurosarcoidosis: a clinical
dilemma. Lancet Neurol 2004;3:397–407.
Article reviews current thinking on clinical features, laboratory findings, neuroimaging,
and therapeutic approaches in neurosarcoidosis.
" Holmes MD, Brant-Zawadzki MM, Simon RP. Clinical features of
meningovascular syphilis. Neurology 1984;34:553–556.
This article discusses progressive syphilitic meningitis, which often transforms into a
bacterial encephalitis.
" Kim L, Glantz MJ. Neoplastic meningitis. Curr Treat Options Oncol
2001;2:517–527.
Authors review the many clinical features with focus on treatment options.
" Marra CM. Human immunodeficiency virus. In: Scheld WM, Whitley RJ,
Marra CM, eds. Infections of the central nervous system. 3rd edition.
Philadelphia: Lippincott Williams & Wilkins, 2004:271–286.
The author reviews the many opportunistic CNS infections associated with human
immunodeficiency virus infection.
" Mazurek GH, Jereb J, LoBue P, et al. Guidelines for using the QuantiFERON-TB
Gold Test for detecting Mycobacterium tuberculosis infection, United States.
MMWR Recomm Rep 2005;54(RR15)49–55.
Latest Centers for Disease Control and Prevention guidelines for the use of QuantiFERON-
TB Gold Test, but report does not address its use to diagnose tuberculous meningitis.
55
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
30. " McKinney RE Jr, Katz SL, Wilfert CM. Chronic enteroviral
meningoencephalitis in agammaglobulinemic patients. Rev Infect Dis
1987;9:334–356.
Reviews 42 patients with chronic enteroviral meningitis associated with
agammaglobulinemia.
" Nadeau SE. Neurologic manifestations of systemic vasculitis. Neurol Clin
2002;20:123–150.
This is an excellent review of the major types of vasculitis that affect the CNS.
" Pai M, Flores LL, Pai N, et al. Diagnostic accuracy of nucleic acid amplification
tests for tuberculous meningitis: a systematic review and meta-analysis.
Lancet Infect Dis 2003;3:633–643.
This meta-analysis found the specificity to be 56% (confidence interval [CI] 46-66) and
sensitivity to be 98% (CI 97–99) for CSF-PCR tests for M. tuberculosis.
" Pai M, Riley LW, Colford JM Jr. Interferon-gamma assays in the
immunodiagnosis of tuberculosis: a systematic review. Lancet Infect Dis
2004;4:761–776.
This article reviews the basis for newly developed interferon assays to diagnose tuberculosis.
" Pappas PG, Rex JH, Sobel JD, et al. Guidelines for treatment of candidiasis.
Clin Infect Dis 2004;38:161–189.
This article discusses challenges to diagnosis and treatment of Candida meningitis.
" Perfect JR. Fungal meningitis. In: Scheld WM, Whitley RJ, Marra CM, eds.
Infections of the central nervous system. 3rd edition. Philadelphia:
Lippincott Williams & Wilkins, 2004:691–712.
This is an up-to-date, thorough review of CNS fungal infections.
" Read RW, Rao NA, Cunningham ET. Vogt-Koyanagi-Harada disease. Curr Opin
Ophthalmol 2000;11:437–442.
Authors briefly review the eye, hair, skin, and meningeal features of Vogt-Koyanagi-Harada
disease and include approaches to therapy.
" Schmidt WA. Use of imaging studies in the diagnosis of vasculitis. Curr
Rheumatol Rep 2004;6:203–211.
This article reviews the value of various neuroimaging techniques to establish a diagnosis
in the large- and small-sized vessel arteritis syndromes.
" Siva A. Vasculitis of the nervous system. J Neurol 2001;248:451–468.
This article covers the many infectious organisms as well as other causes of primary
vasculitis of the CNS.
" Smith CE, Saito MT, Simons SA. Patterns of 39,500 serologic tests in
coccidioidomycosis. JAMA 1956;160:546–552.
This classic paper describes the high sensitivity and specificity of this serological test in
CSF.
" Smith JE, Aksamit AJ Jr. Outcome of chronic idiopathic meningitis. Mayo Clin
Proc 1994;69:548–556.
This is an excellent study that followed patients with chronic meningitis in which the
diagnosis could not be established.
56
"SUBACUTE AND CHRONIC MENINGITIS
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
31. " Tan TQ. Chronic meningitis. Semin Pediatr Infect Dis 2003;14:131–139.
This is a comprehensive review of major infectious causes of chronic meningitis with
helpful ways to approach the workup.
" Thwaites GE, Tran TH. Tuberculous meningitis: many questions, too few
answers. Lancet Neurol 2005;4:160–170.
This article reviews current challenges for diagnosis and treatment of tuberculous
meningitis as we move into the antibiotic-resistant era.
" Weinberg A, Bloch KC, Li S, et al. Dual infections of the central nervous
system with Epstein-Barr virus. J Infect Dis 2005;191:234–237.
These authors report 10 of 16 immunocompromised patients and three of six
immunocompetent patients who had dual infections (Epstein-Barr virus plus another
infectious agent) detected in CSF by PCR assay, raising the question as to whether
Epstein-Barr virus had anything to do with the original illness.
" West SG. Central nervous system vasculitis. Curr Rheumatol Rep
2003;5:116–127.
This article reviews the clinical features, laboratory tests, neuroimaging, and brain biopsy
findings in diagnosing this uncommon but challenging primary vasculitis of the CNS.
" Wheat J, Sarosi G, McKinsey D, et al. Practice guidelines for management
of patients with histoplasmosis. Infectious Diseases Society of America.
Clin Infect Dis 2000;30:688–695.
These are the current guidelines for diagnosis and treatment of patients with
histoplasmosis, including histoplasma meningitis.
" Wilhelm C, Ellner JJ. Chronic meningitis. Neurol Clin 1986;4:115–141.
This article presents a general approach to the patient with chronic meningitis, coupled
with information on the more common causes.
" Wilhelm CS, Marra CM. Chronic meningitis. Semin Neurol 1992;12:234–247.
This article reviews the major causes of chronic meningitis with some information on
treatment.
" Wynne PJ, Younger DS, Khandji A, Silver AJ. Radiographic features of central
nervous vasculitis. Neurol Clin 1997;15:779–804.
Article reviews the typical findings in cerebral arteriography, computer tomography,
and magnetic resonance imaging for many causes of vasculitis and includes excellent
illustrations.
" Younger DS. Vasculitis of the nervous system. Curr Opin Neurol
2004;17:317–336.
This article reviews the recent findings in CNS vasculitis, including classification and
immunopathogenesis.
" Yurdakul S, Hamuryudan V, Yazici H. Behc¸et syndrome. Curr Opin Rheumatol
2004;16:38–42.
Authors briefly review the clinical features including the CNS with current treatment
approaches.
" Zimmerman RA, Wong AM, Girard N. Imaging of intracranial infections.
In: Scheld WM, Whitley RJ, Marra CM, eds. Infections of the central nervous
system. 3rd edition. Philadelphia: Lippincott Williams & Wilkins, 2004:31–55.
This chapter reviews all neuroimaging findings in CNS infections, including meningitis.
57
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.