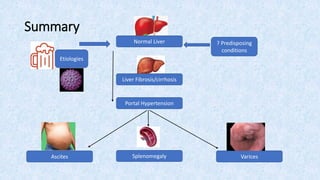
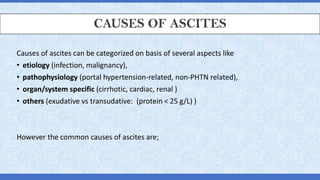
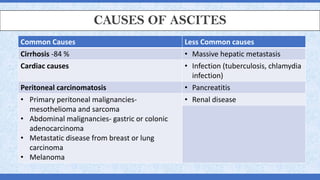
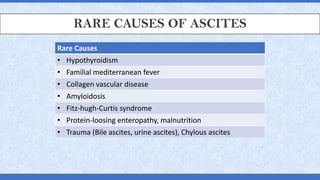
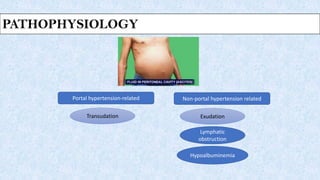
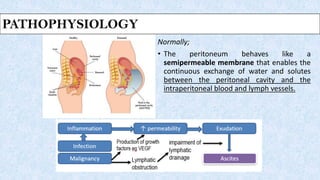
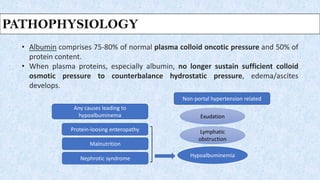
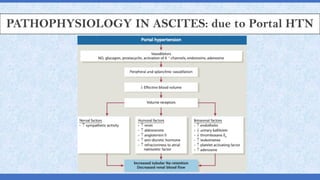
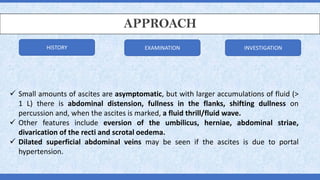
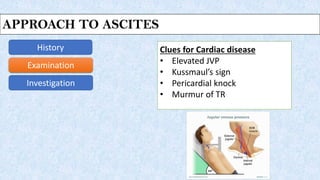
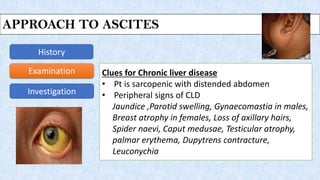
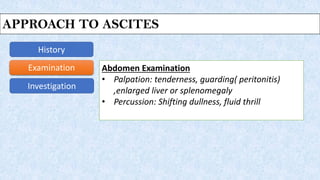
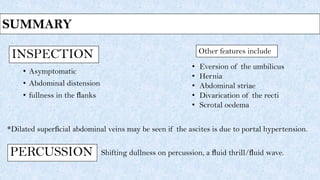
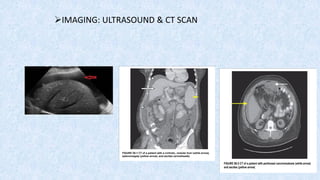
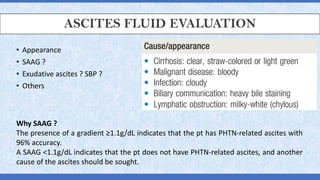
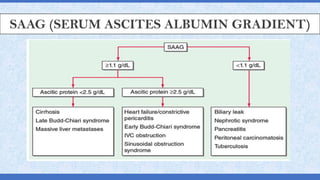
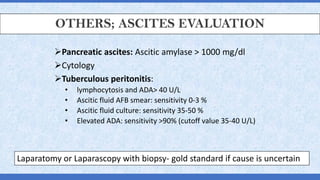
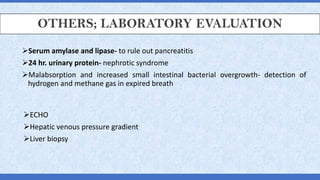
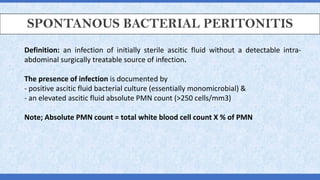
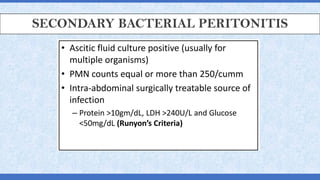
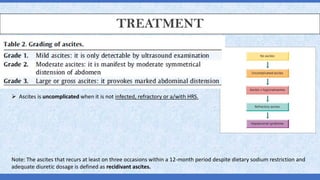
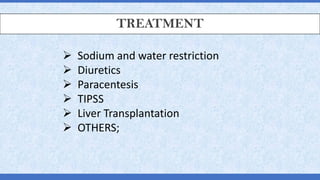
This document provides a comprehensive overview of ascites, including its definitions, causes, pathophysiology, and management approaches. Common causes of ascites are categorized primarily into cirrhosis and less common conditions such as malignancies and infections, with diagnostic approaches involving history, examination, imaging, and fluid evaluation. It also details the significance of the serum-ascites albumin gradient (SAAG) and discusses spontaneous bacterial peritonitis, emphasizing treatment options for recurring cases.