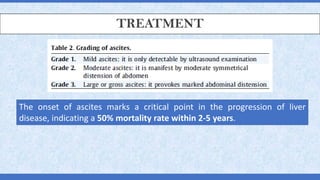
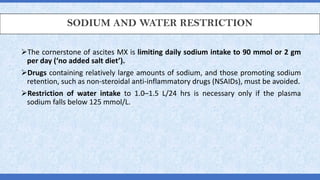
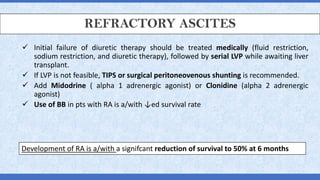
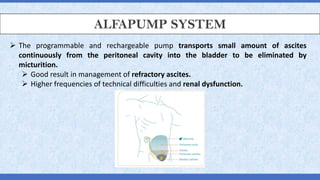
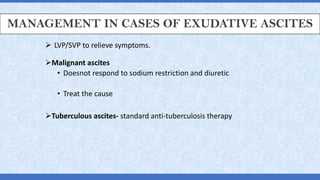
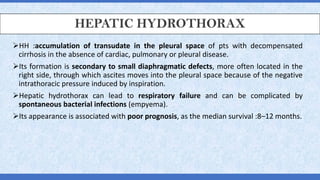
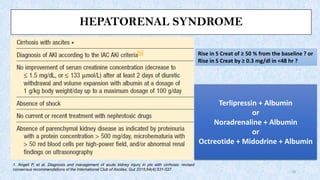
This document outlines the management and treatment of ascites and related conditions in patients with liver disease, emphasizing sodium and water restriction, diuretics, and therapeutic procedures like paracentesis and TIPS. Refractory ascites and its definition, causes, and treatment options are discussed, including medication alternatives and the importance of monitoring renal function. Also covered are complications such as spontaneous bacterial peritonitis and hepatic hydrothorax, with recommendations for antibiotic therapy and management strategies.