This document provides information about Idiopathic Thrombocytopenic Purpura (ITP), including:
- ITP is a blood disorder characterized by a decreased number of platelets, which can cause easy bruising and bleeding.
- There are two main forms - acute (seen in children and resolves in <6 months) and chronic (onset at any age and lasts >6 months).
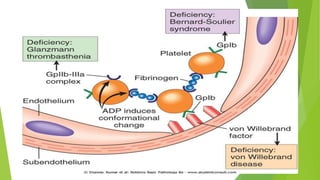
- The cause is unknown in most cases but involves antibodies destroying platelets. Diagnosis involves ruling out other causes through testing.
- Treatment options depend on severity but may include steroids, IVIg, splenectomy, thrombopoietin receptor agonists, and experimental agents.
![Anti-D
Another option, suitable for Rh-positive, non-splenectomized patients is
intravenous administration of Rho(D) immune globulin [Human; Anti-D].
The mechanism of action of anti-D is not fully understood. However, following
administration, anti-D-coated red blood cell complexes saturate Fcγ receptor sites
on macrophages, resulting in preferential destruction of red blood cells (RBCs),
therefore sparing antibody-coated platelets.
Steroid-sparing agents
Immunosuppresants such as mycophenolate mofetil and azathioprine
vincristine, a chemotherapy agent,and vinca alkaloid, has significant side-effects
and To be used with caution, especially in children.
Intravenous immunoglobulin (IVIg) may be infused in some cases. it is costly and
produces improvement that generally lasts less than a month.](https://image.slidesharecdn.com/itp-141120133517-conversion-gate02/85/idiopathic-thrombocytopinic-purpura-13-320.jpg)