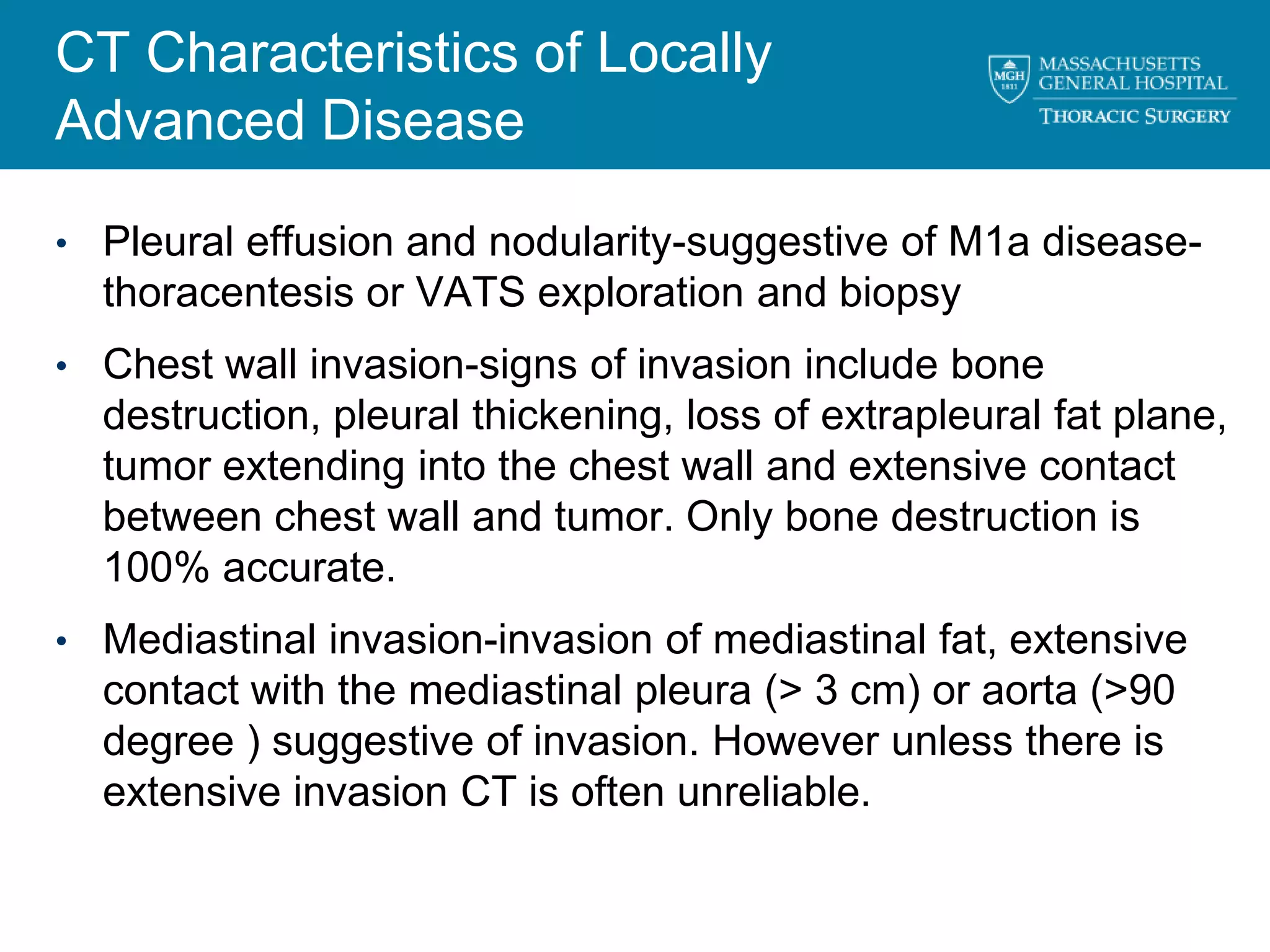
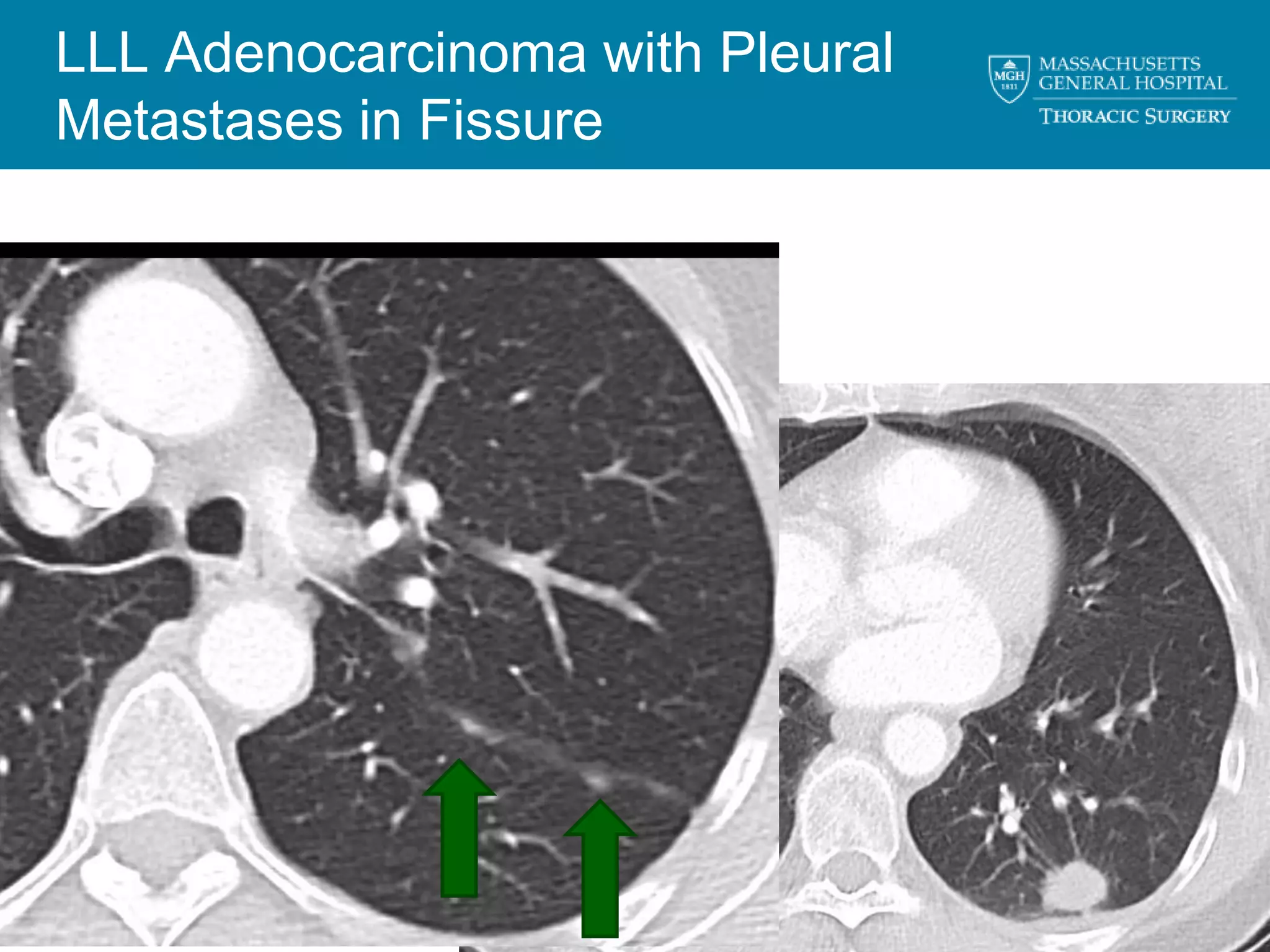
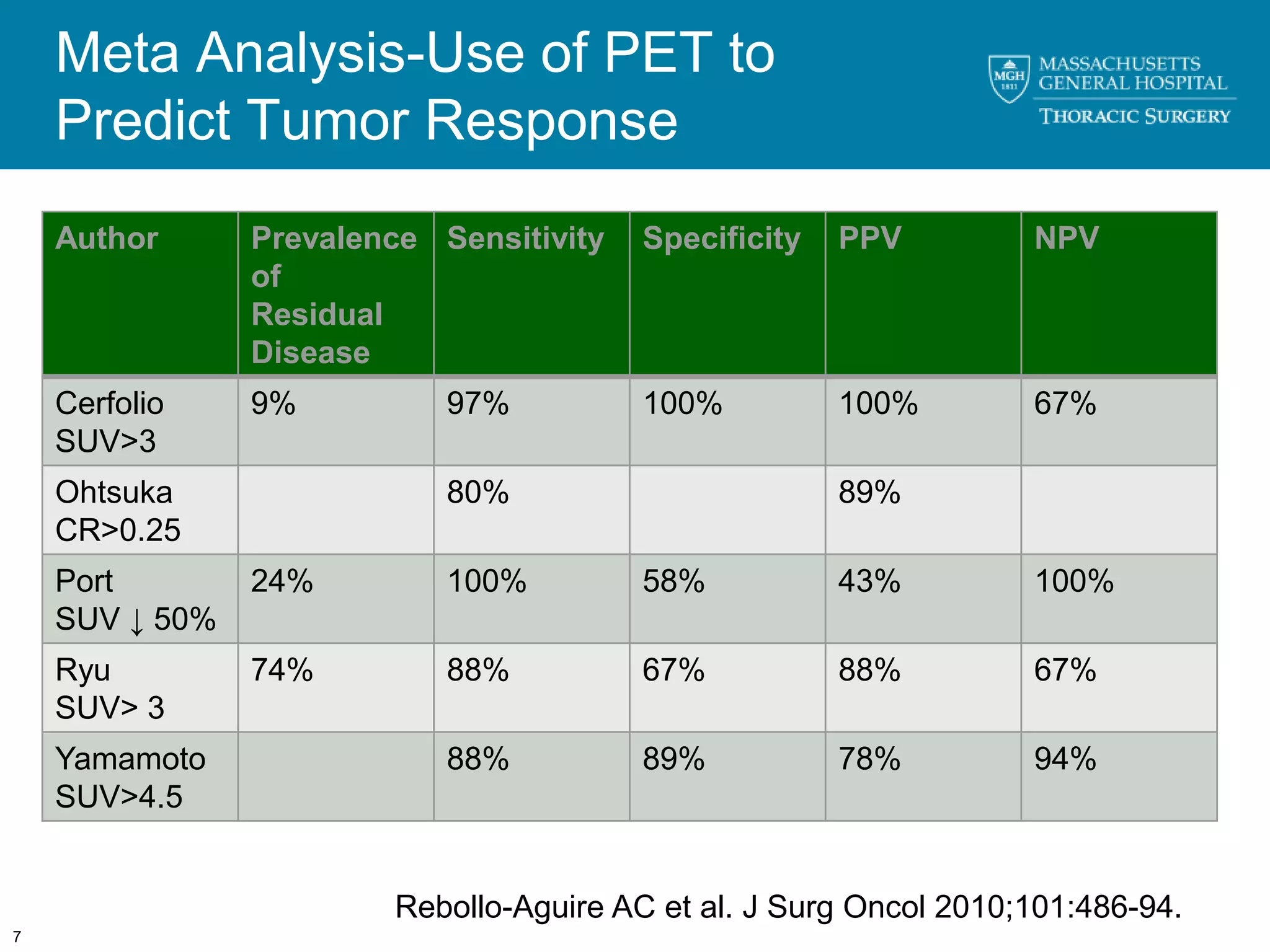
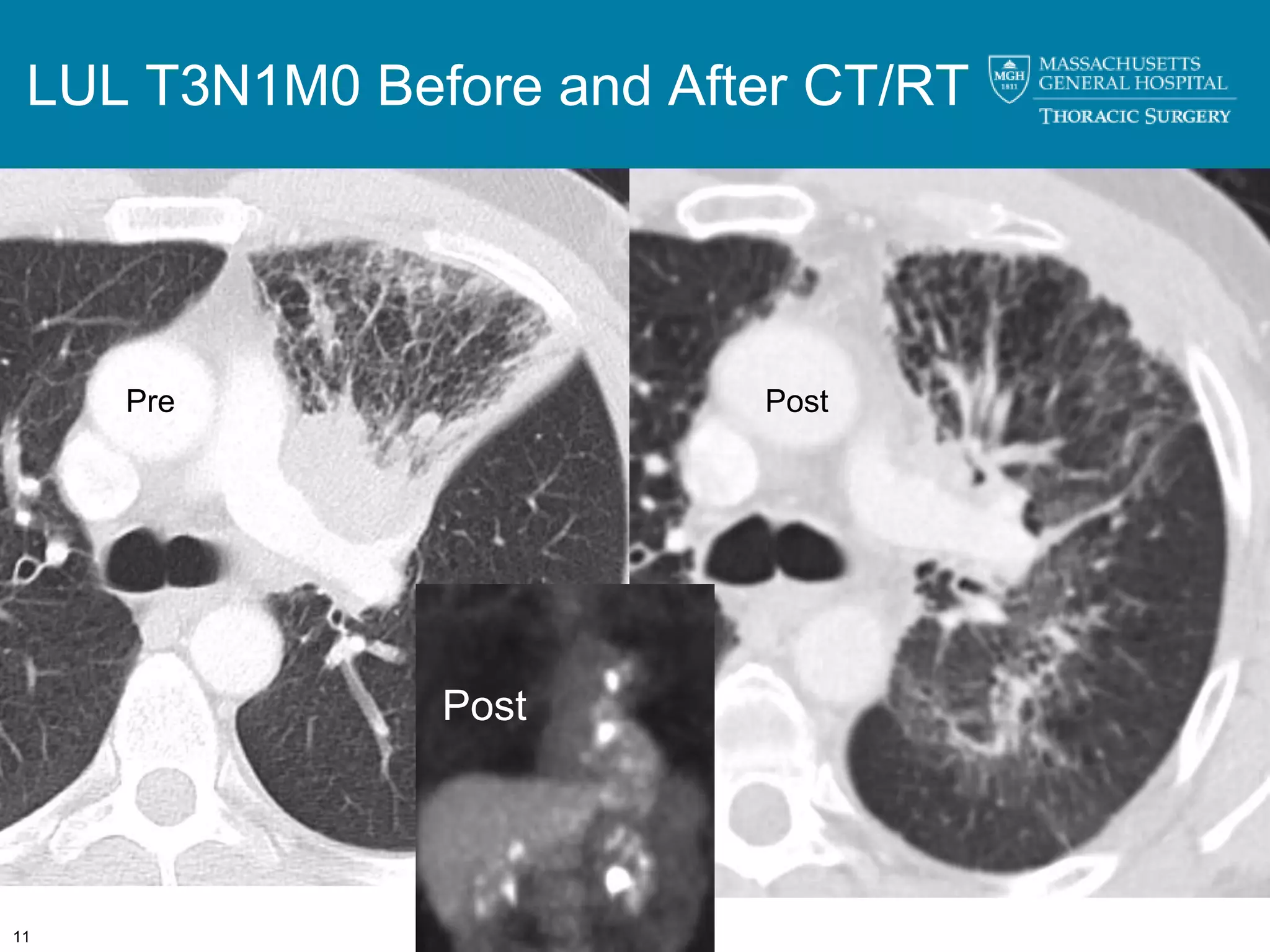
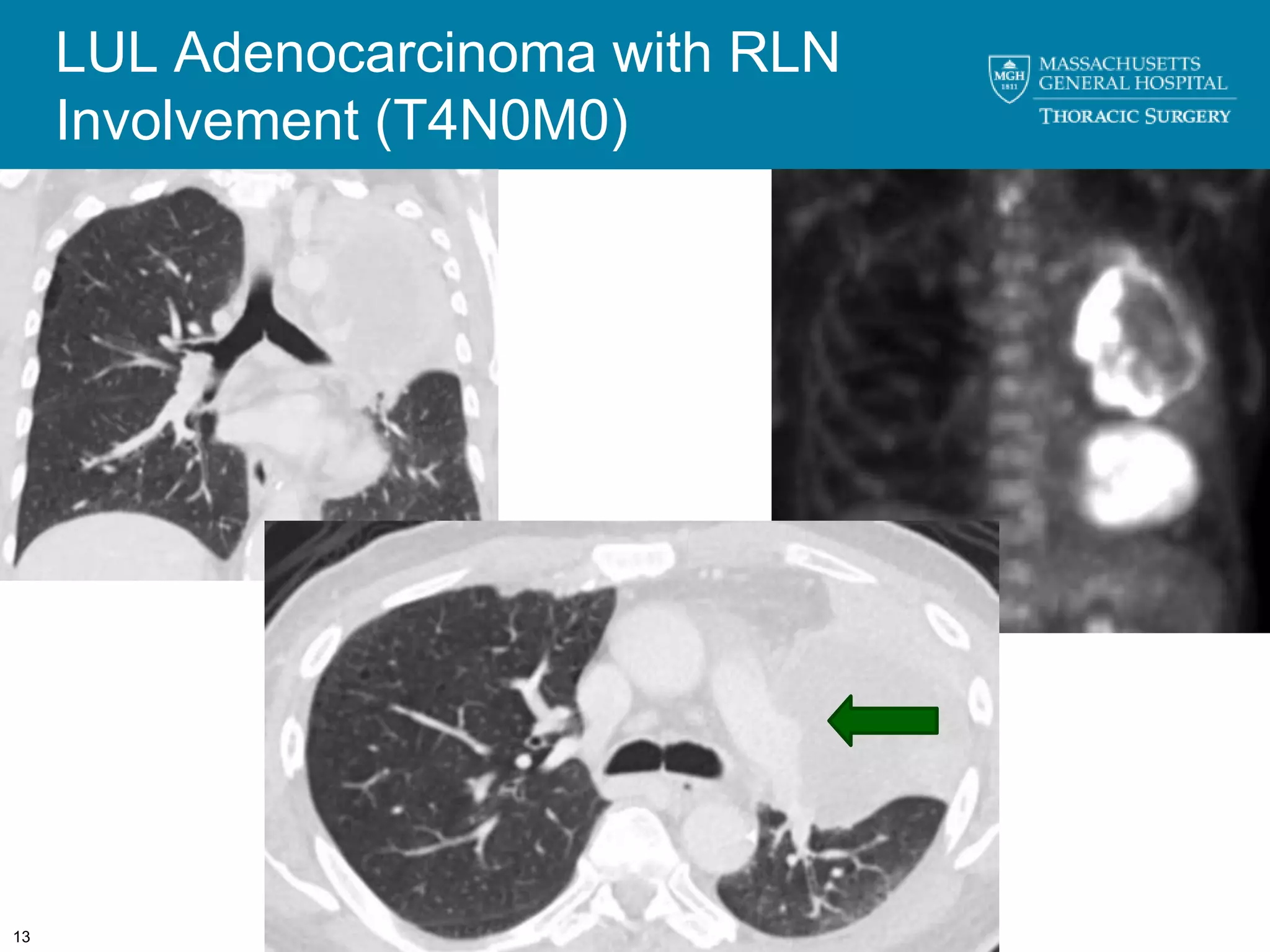
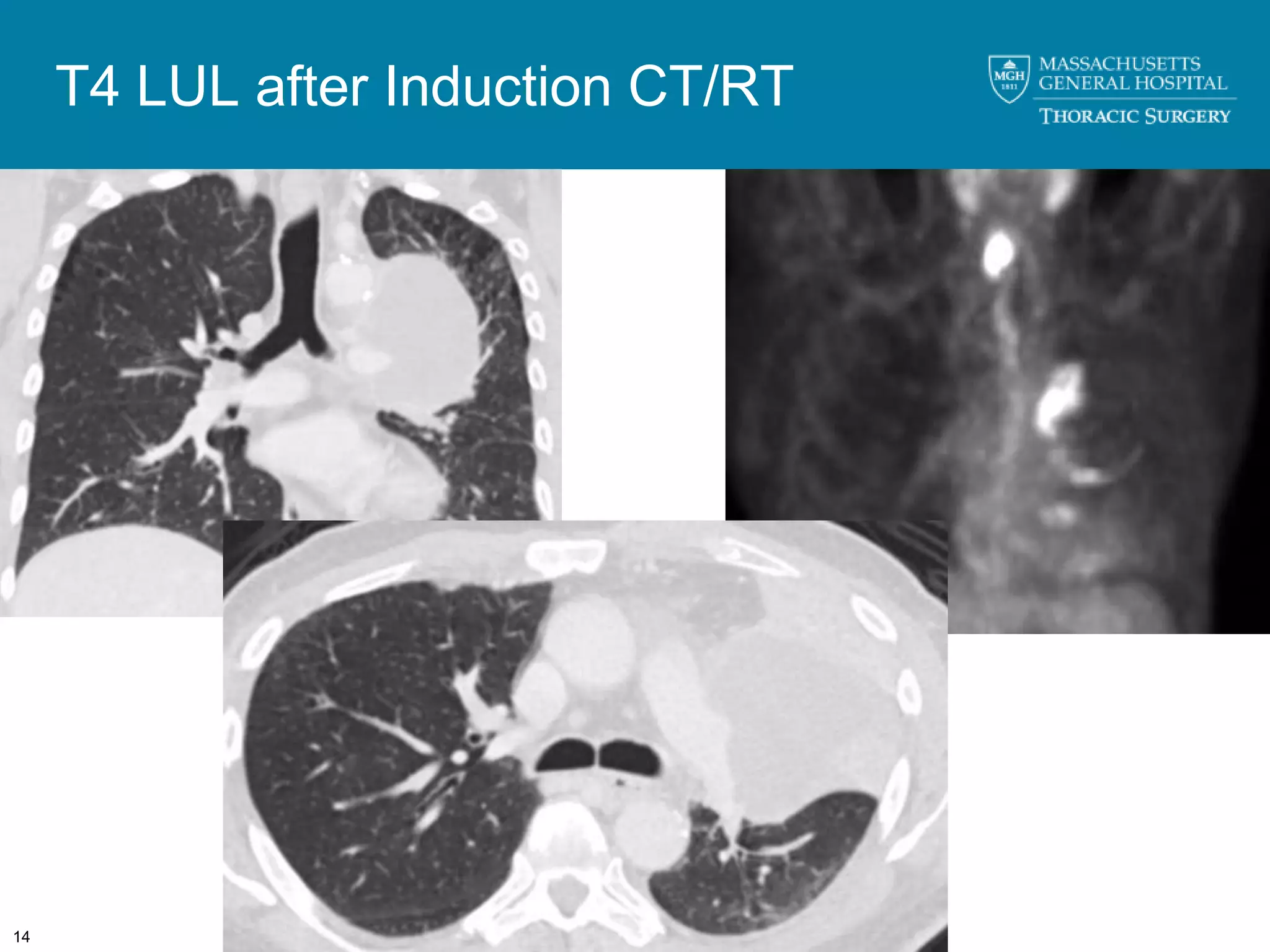
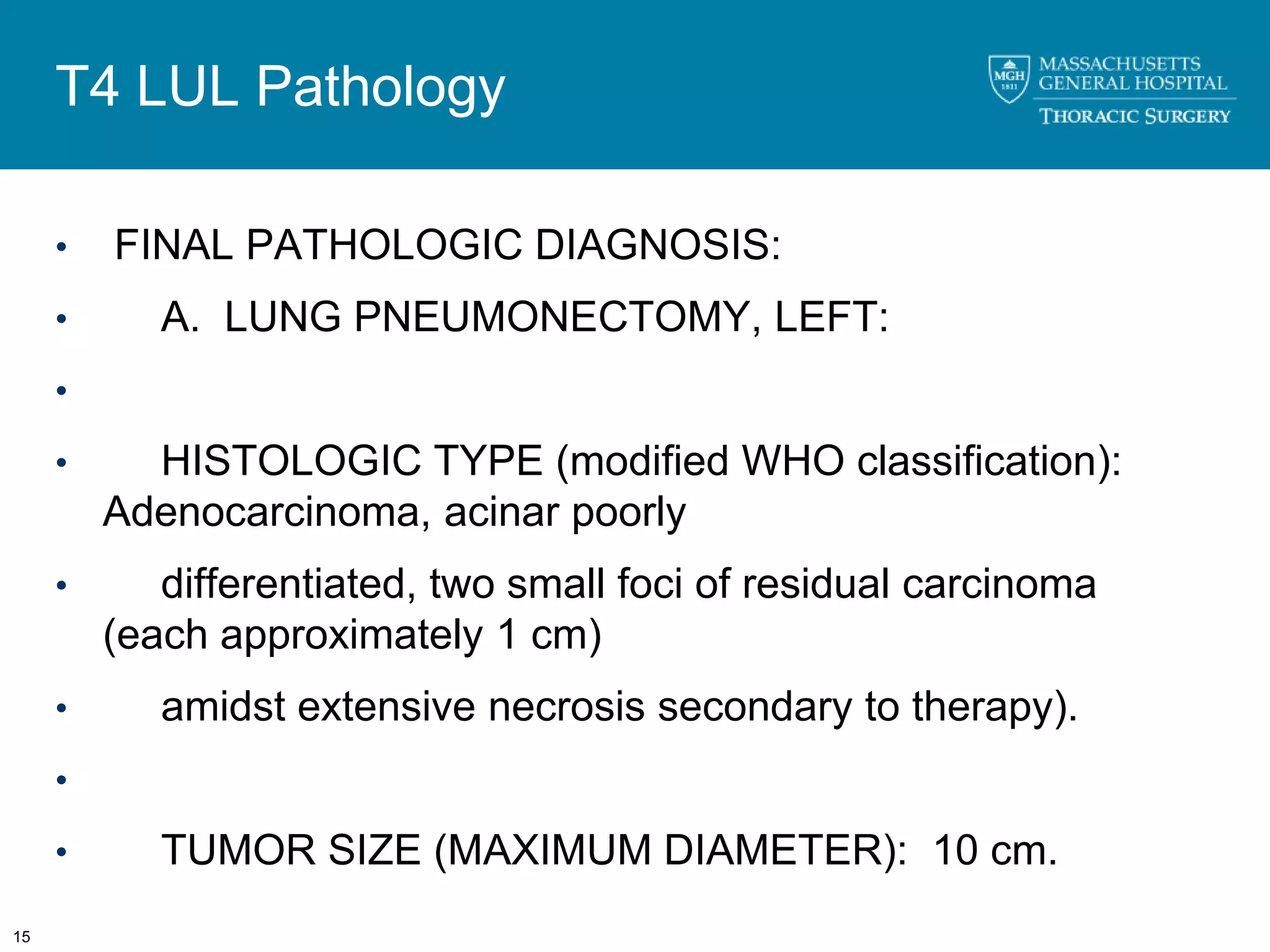
1. Restaging lung cancer patients after induction therapy is difficult to interpret based on radiographic methods alone due to their poor predictive value in assessing tumor response and mediastinal involvement.
2. While PET/CT may help predict tumor response, timing is important as optimal accuracy occurs around 26 days after therapy.
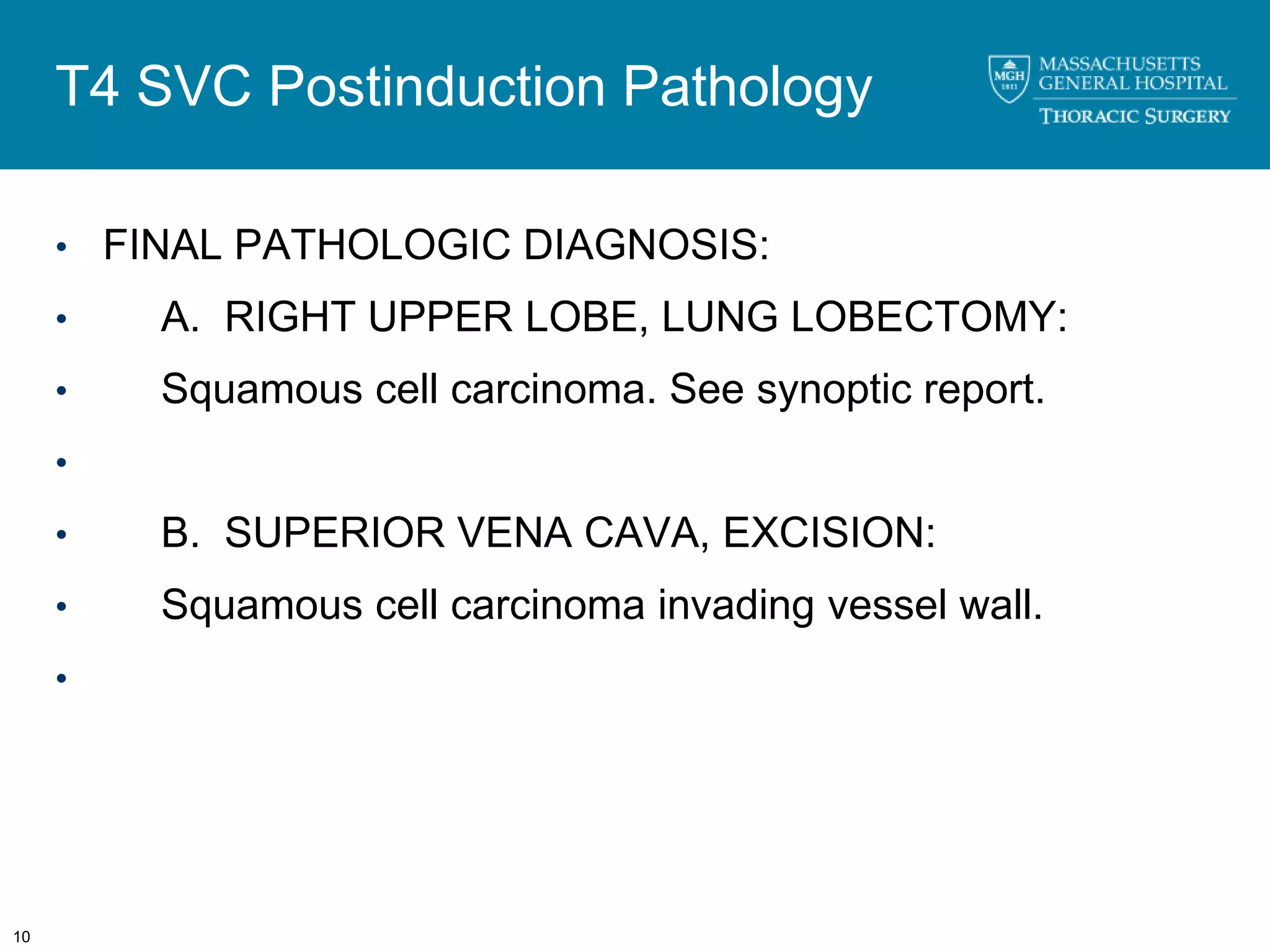
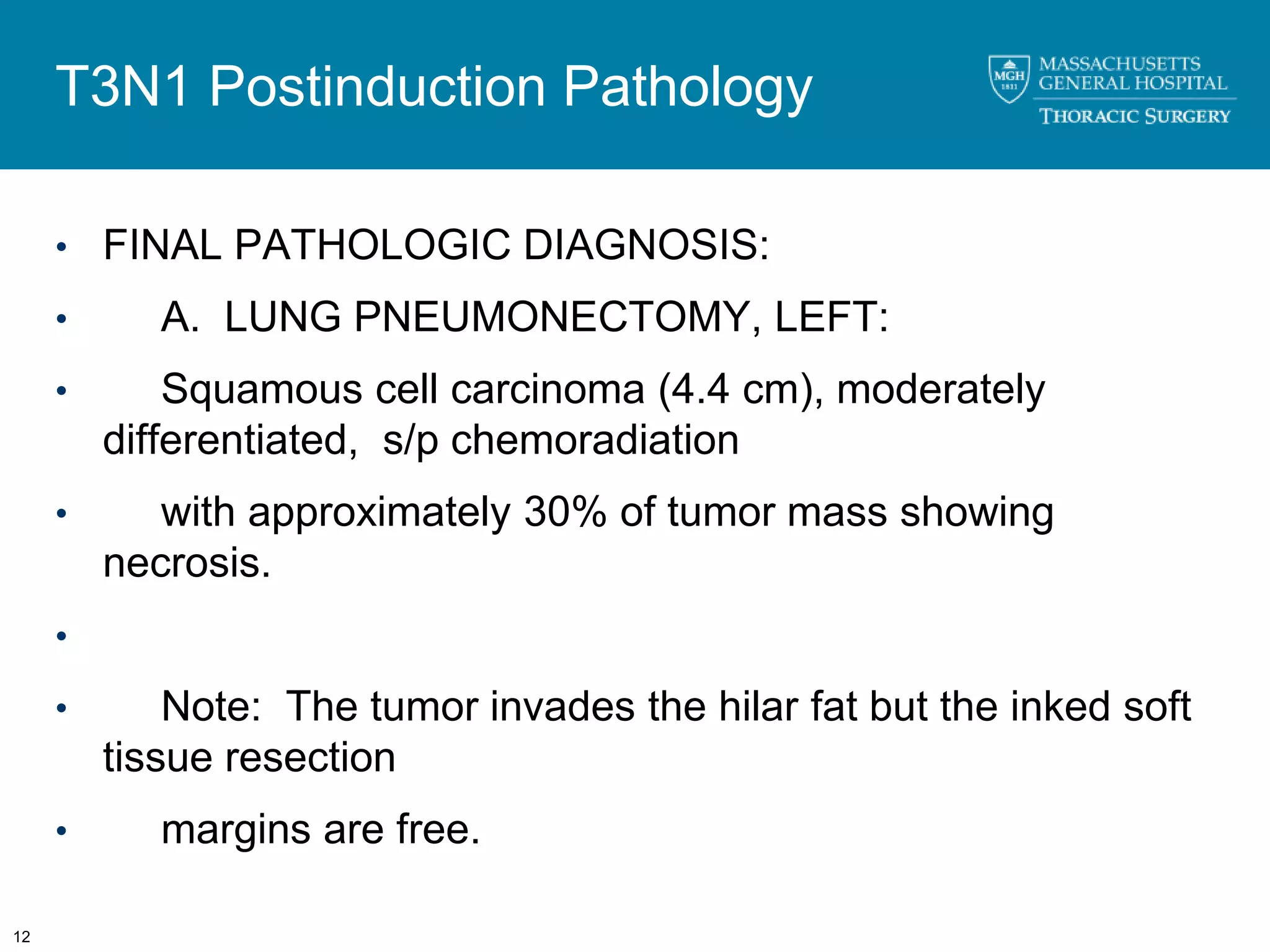
3. Surgical exploration remains important for confirming radiographic findings and assessing resectability given imaging limitations in evaluating response to induction therapies.