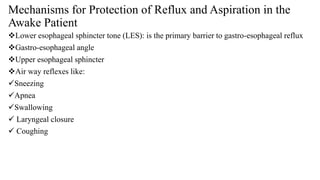
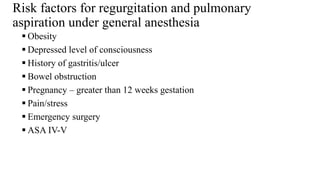
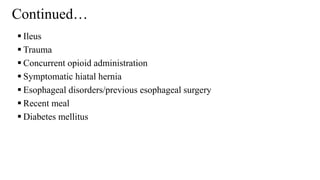
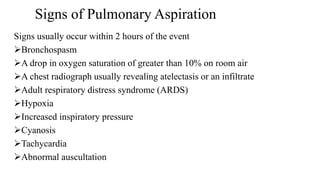
This document discusses aspiration, its classification, risk factors, signs, and prevention. It defines aspiration as the inhalation of oropharyngeal or gastric contents into the larynx and lower respiratory tract. Aspiration can cause aspiration pneumonitis from gastric contents or aspiration pneumonia from oropharyngeal material. Risk factors for aspiration under anesthesia include obesity, impaired consciousness, and recent eating. Signs usually occur within 2 hours and include bronchospasm, hypoxia, and infiltrates on chest x-ray. Prevention methods discussed are using medications to reduce gastric volume or increase pH, as well as applying cricoid pressure during intubation.