This document summarizes different diseases of skeletal muscle including:
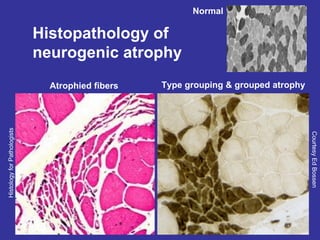
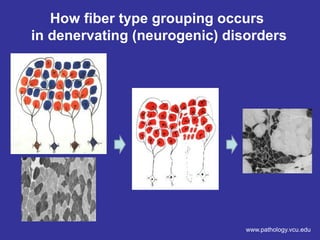
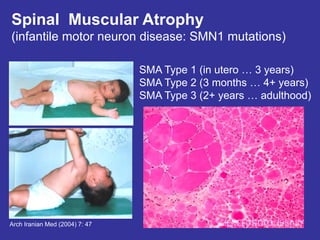
1) Neurogenic atrophy which is caused by damage to peripheral nerves or motor neurons. It results in muscle fiber atrophy and grouping.
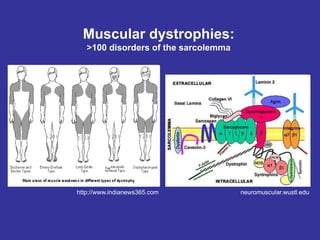
2) Muscular dystrophies which are genetic disorders of the sarcolemma including Duchenne muscular dystrophy characterized by loss of dystrophin and inflammation.
3) Metabolic myopathies such as McArdle disease caused by glycogen breakdown defects and mitochondrial myopathies with accumulation of abnormal mitochondria.
4) Inflammatory myopathies such as dermatomyositis with skin rashes and perivascular inflammation and inclusion body myositis seen in older adults.