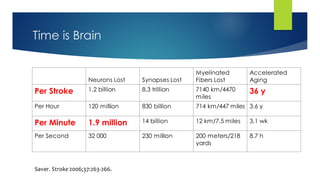
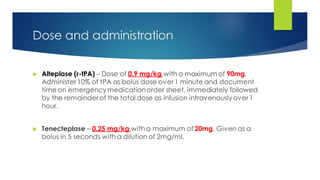
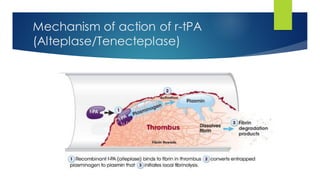
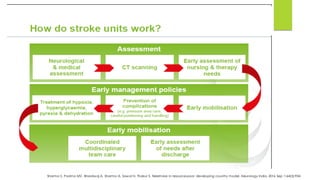
The document discusses the critical guidelines for thrombolysis in acute ischemic stroke, emphasizing that treatment should be administered within a 4.5-hour window to maximize brain preservation. It outlines eligibility criteria, contraindications, and post-thrombolysis management protocols to mitigate complications. The importance of a coordinated stroke management team and ongoing staff training is highlighted to improve patient outcomes.