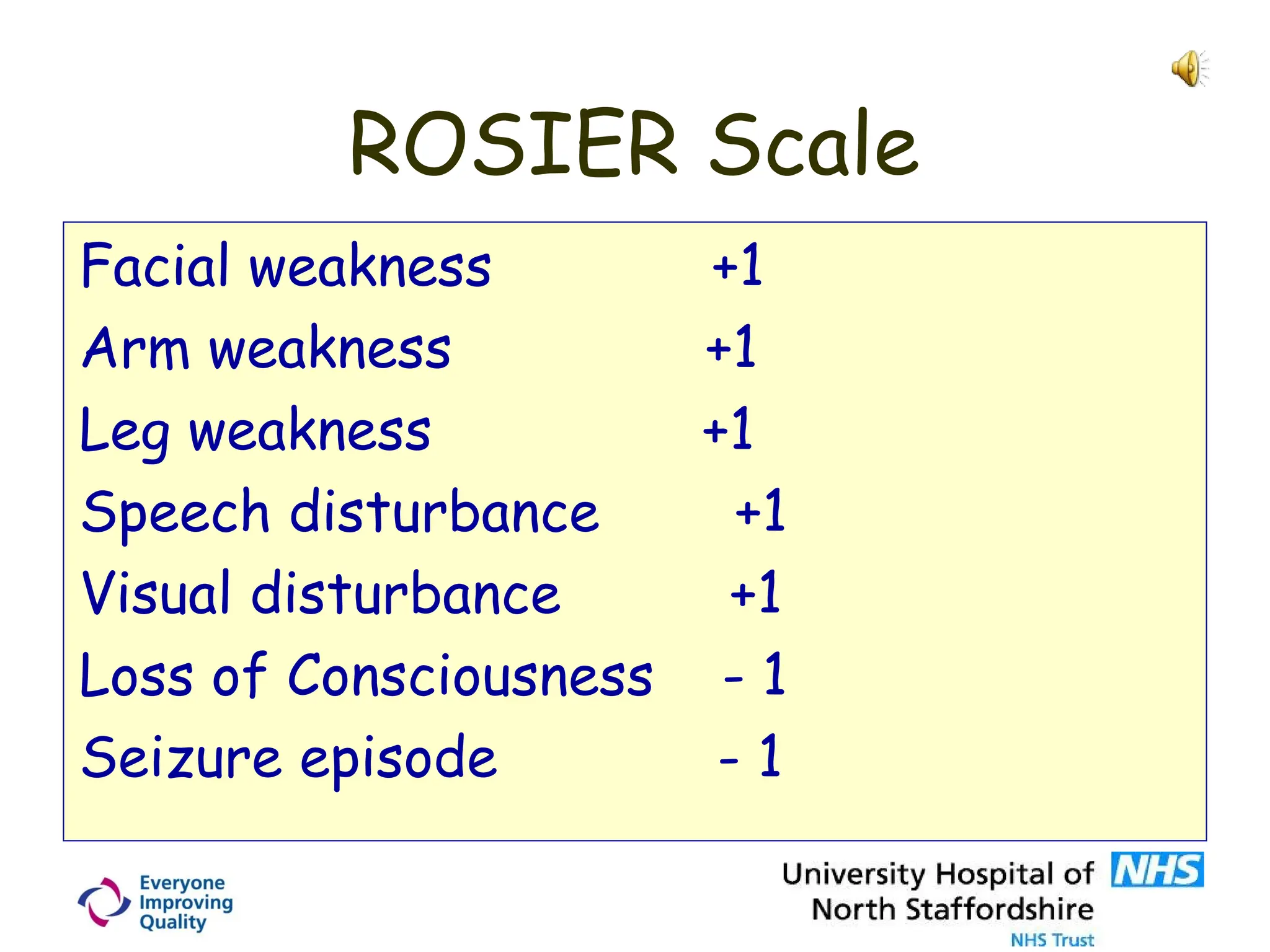
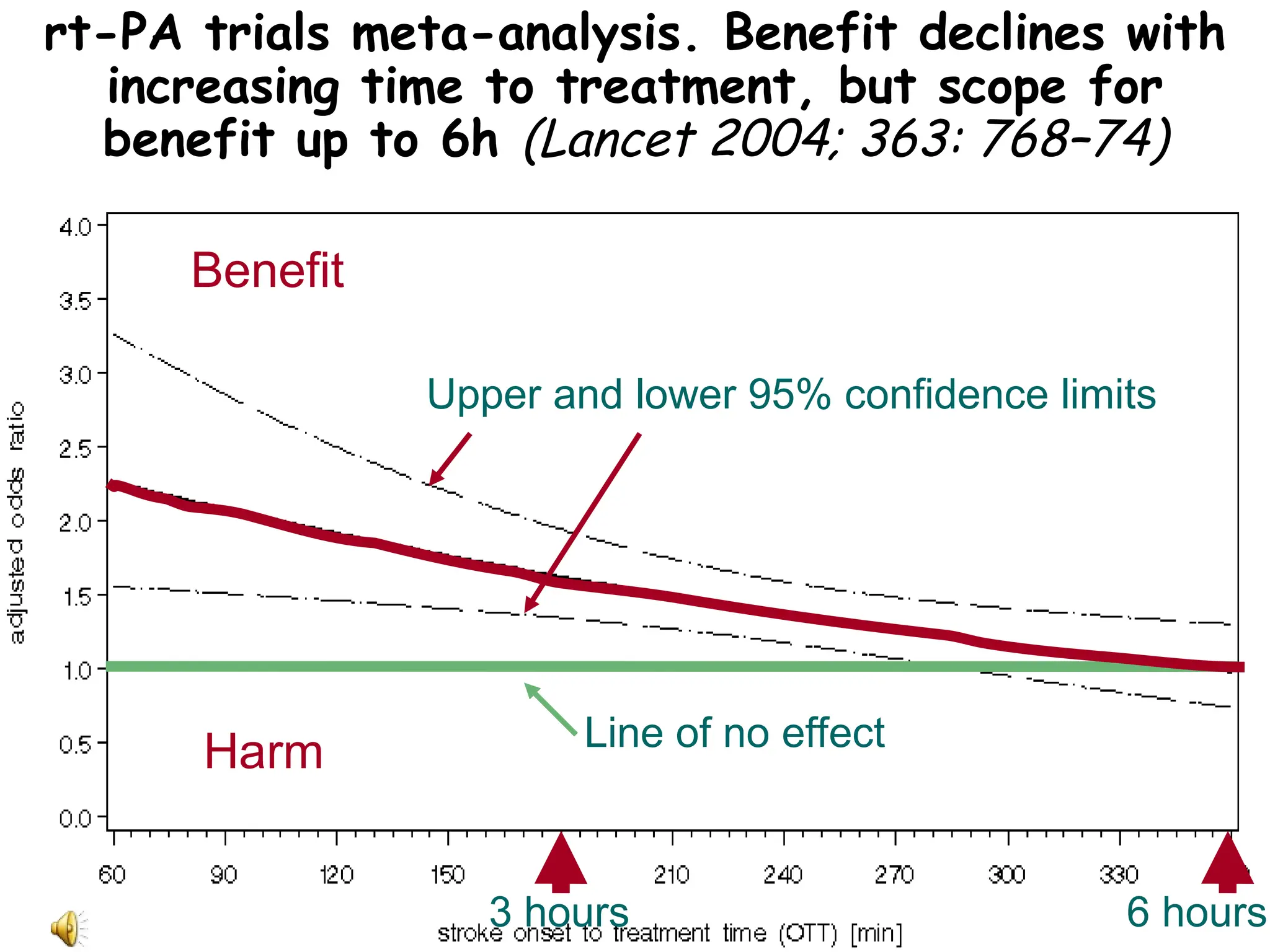
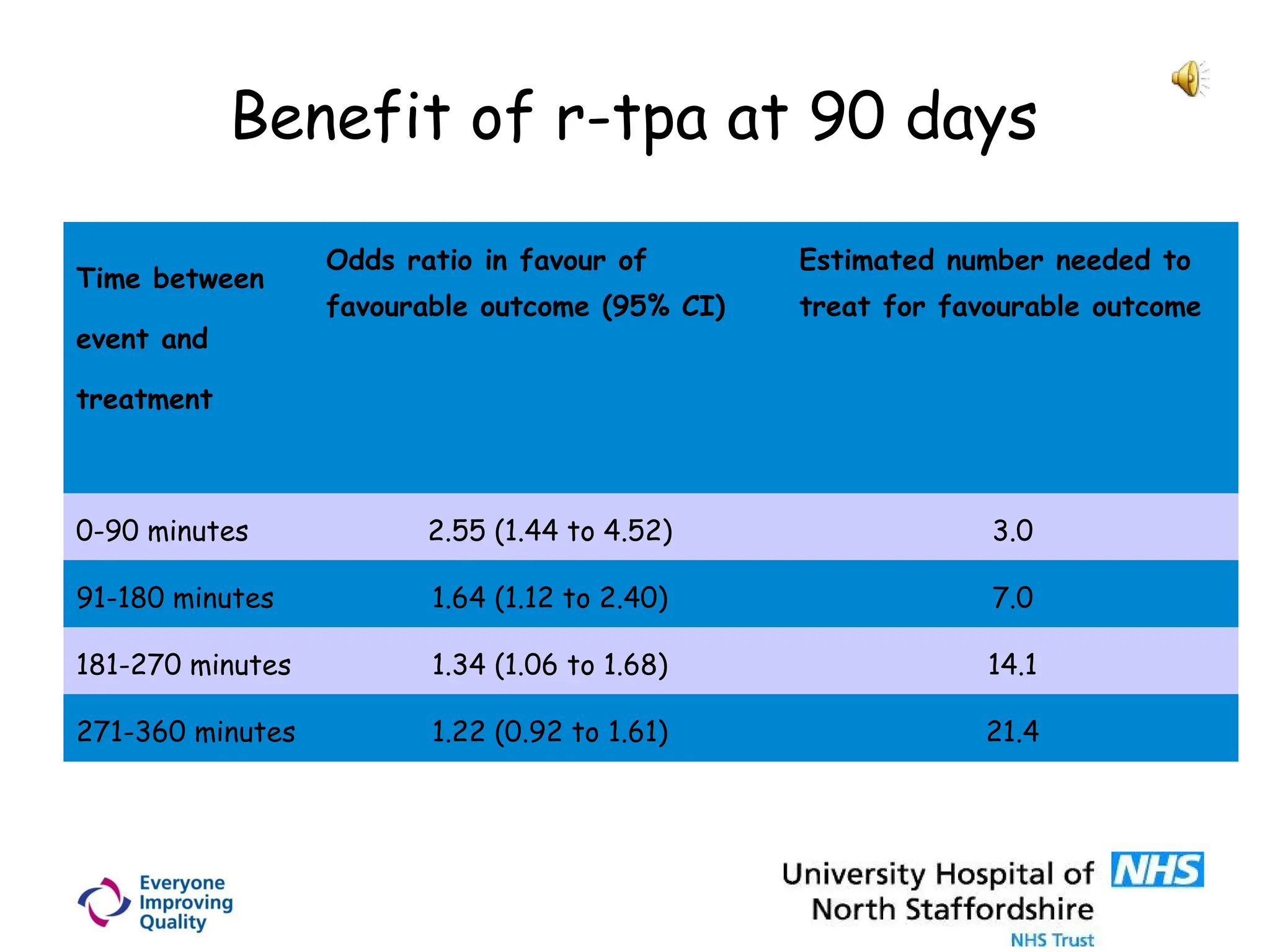
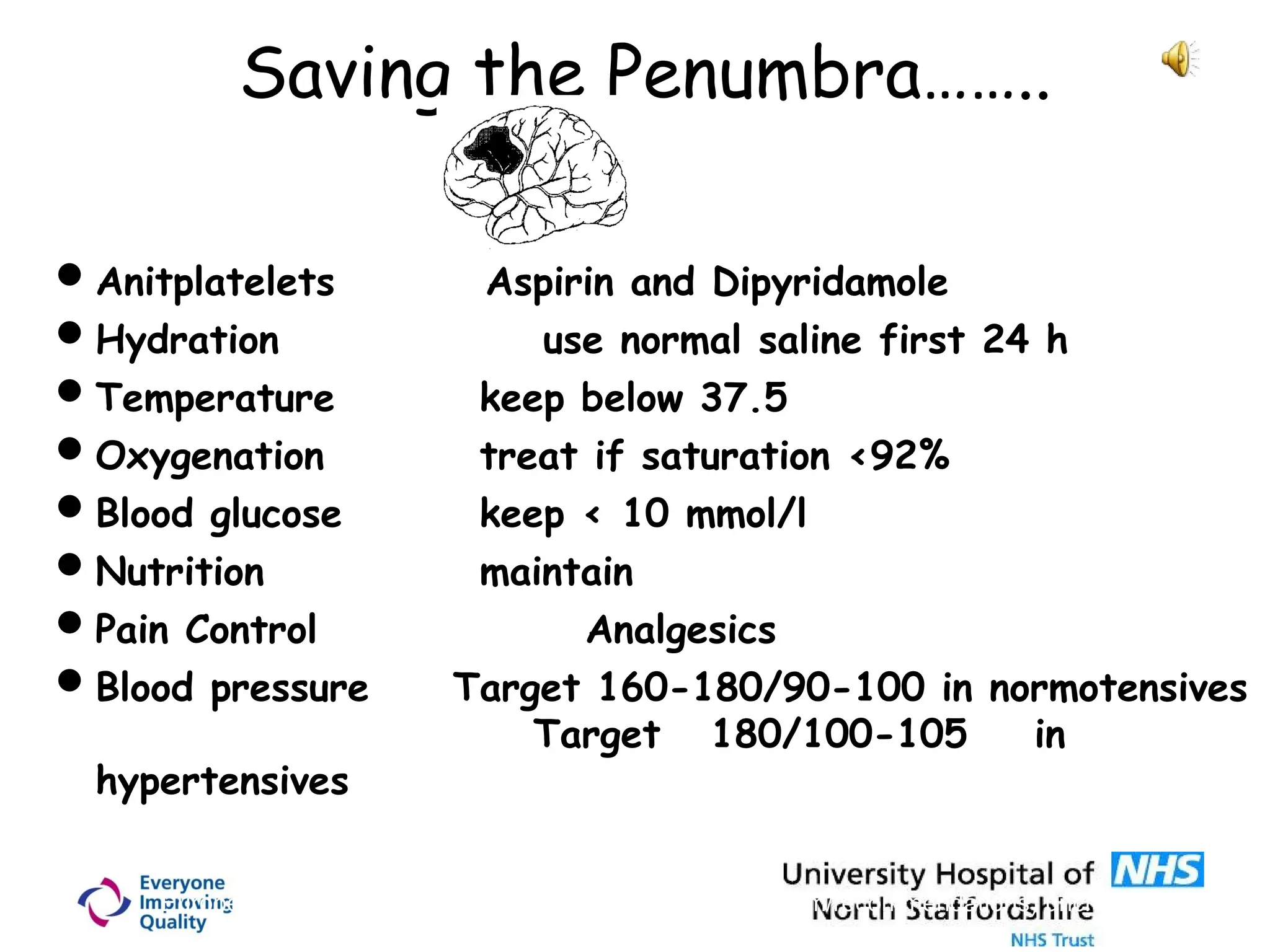
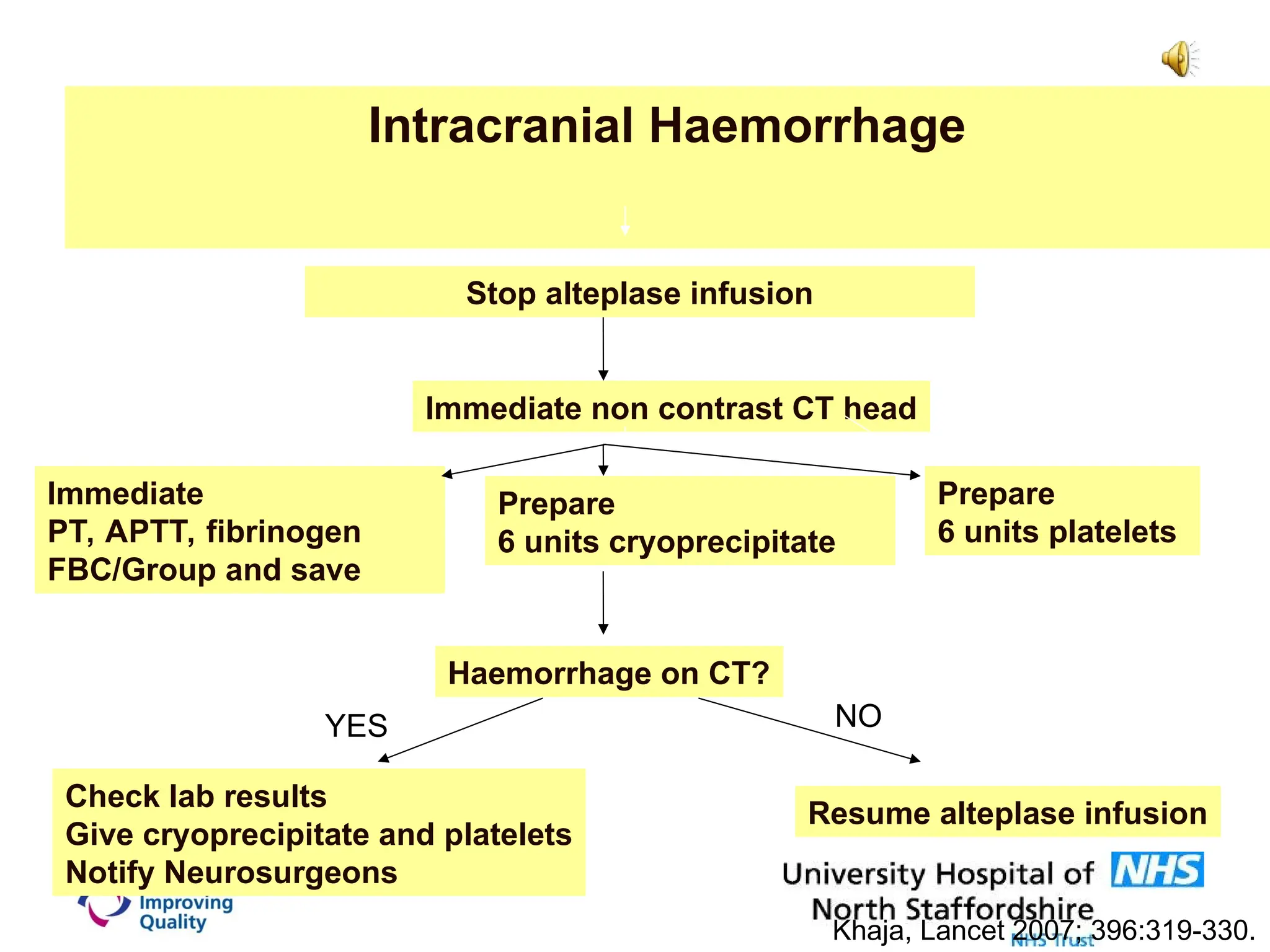
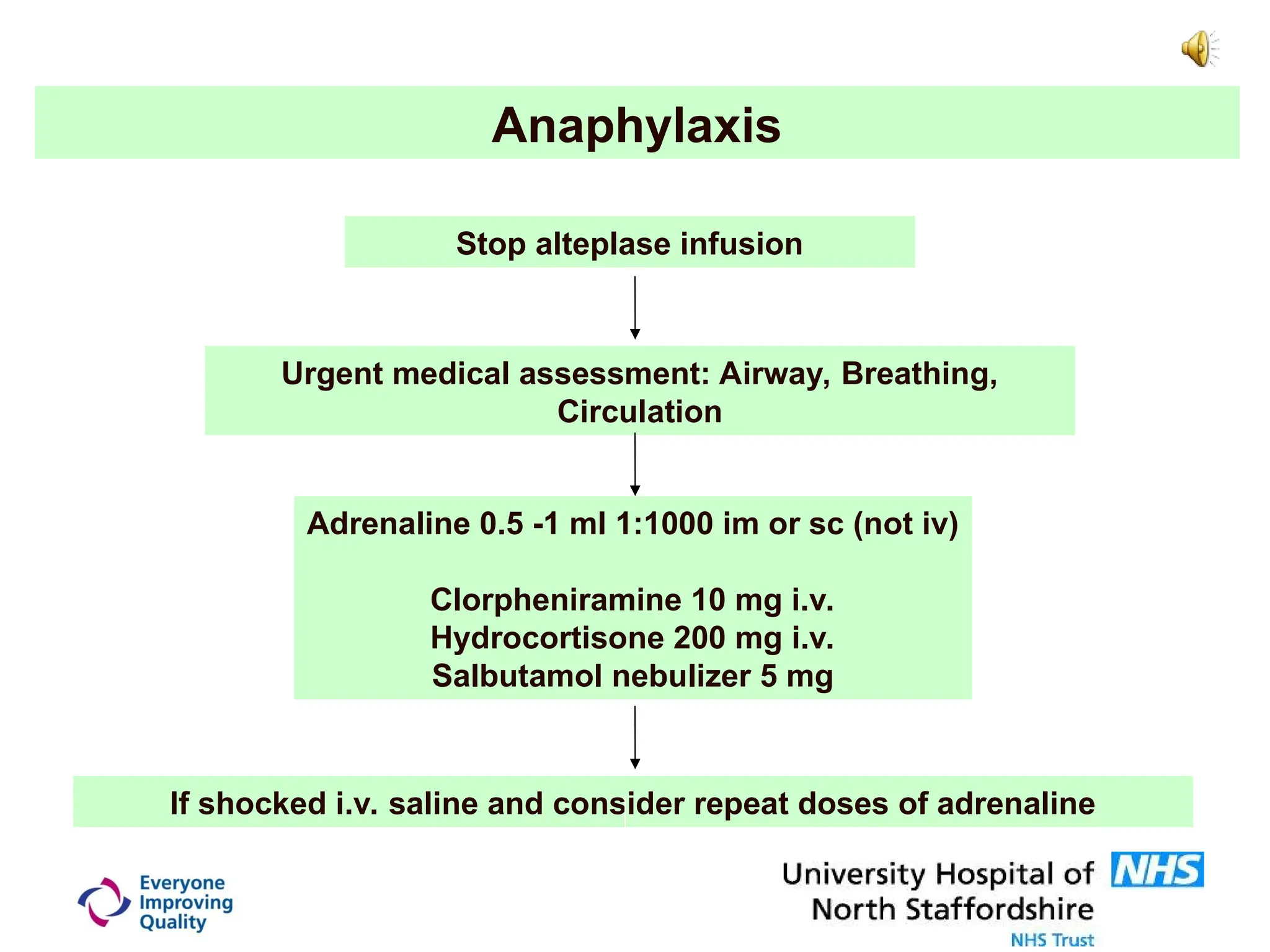
The document outlines essential practices in stroke thrombolysis training, emphasizing the importance of timely treatment to minimize neuronal loss. It covers diagnostic dilemmas, treatment eligibility criteria, potential complications, and management of intracranial hemorrhage. Key recommendations include maintaining patient stability, monitoring specific physiological parameters, and addressing contraindications for thrombolysis.