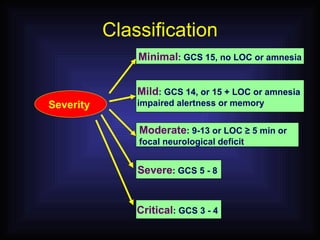
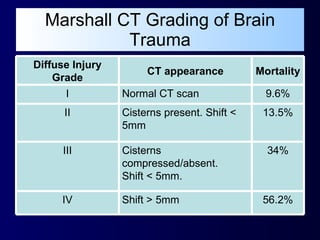
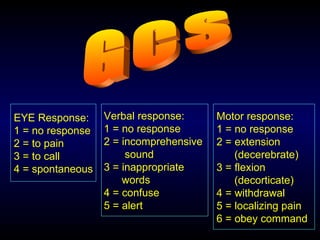
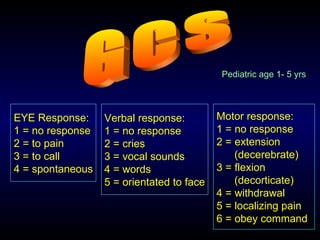
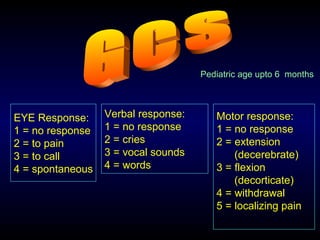
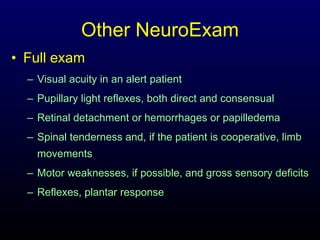
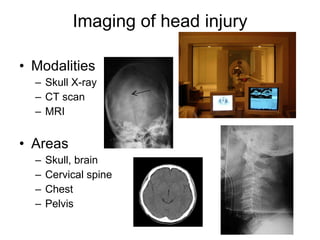
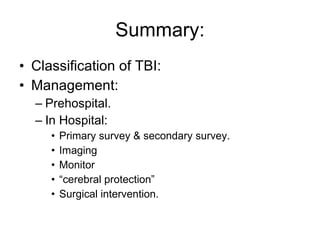
1. The document discusses classification and management of traumatic head injuries, including grading severity based on Glasgow Coma Scale and anatomical findings on CT scans.
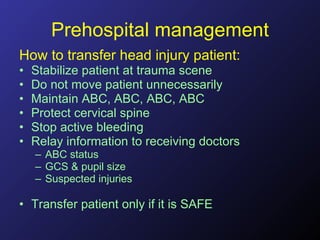
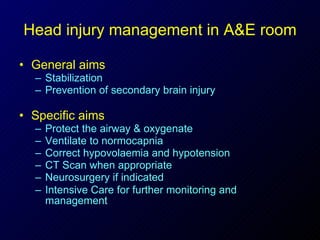
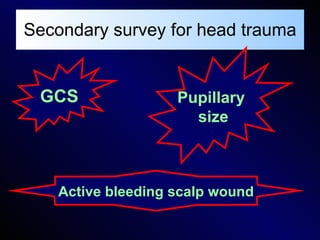
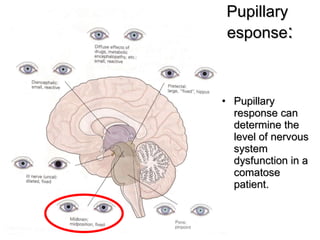
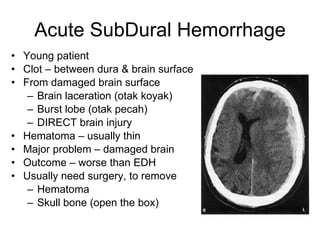
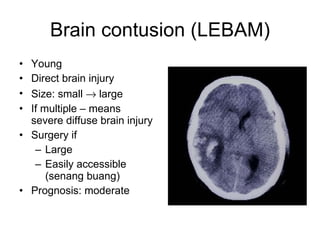
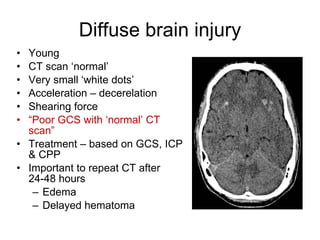
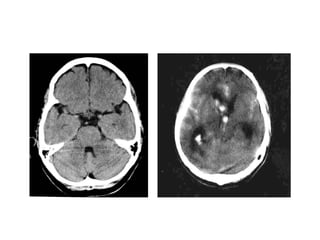
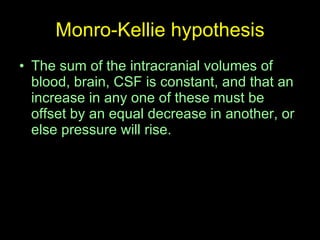
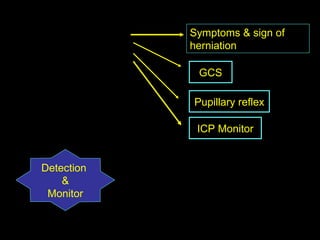
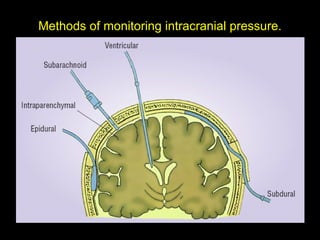
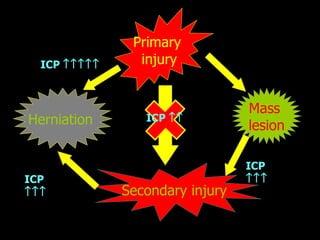
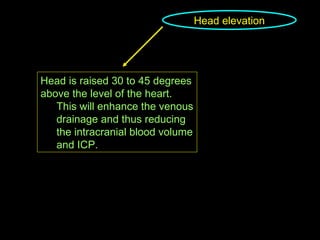
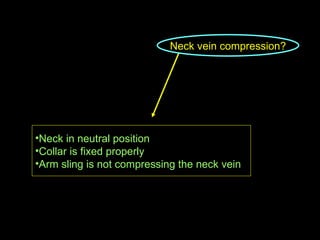
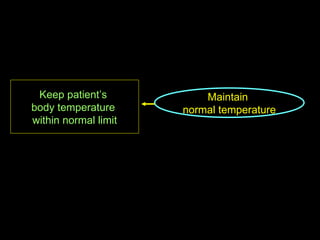
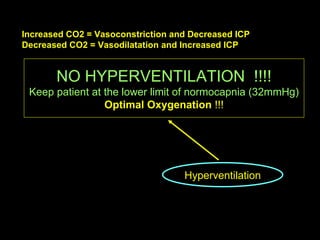
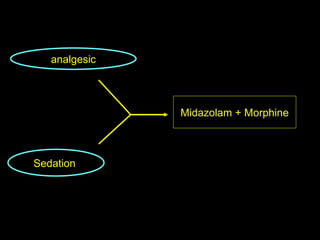
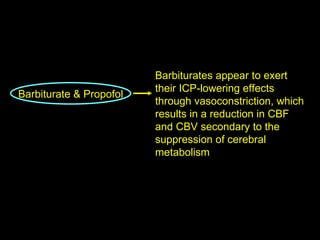
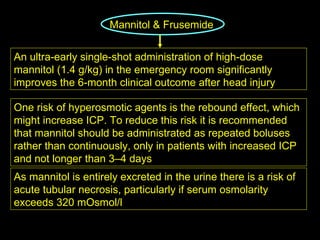
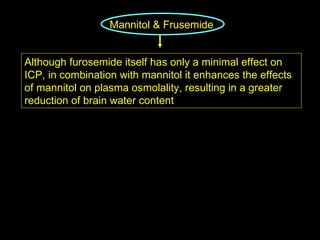
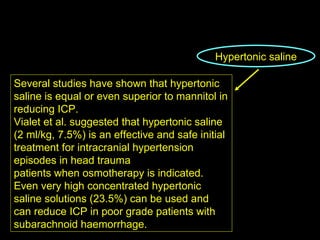
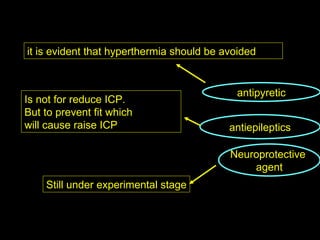
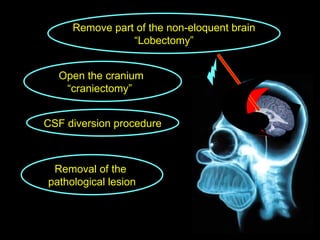
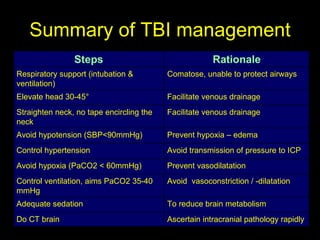
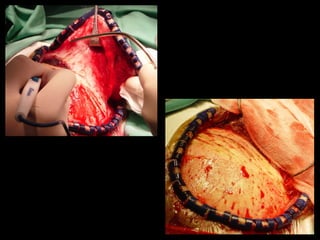
2. Management involves stabilizing patients through the pre-hospital and hospital phases, monitoring intracranial pressure, and treating to prevent secondary brain injuries using medical and surgical methods like intubation, sedation, osmotherapy, and surgical evacuation of hematomas if needed.
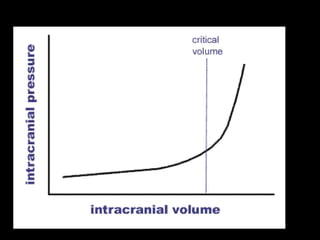
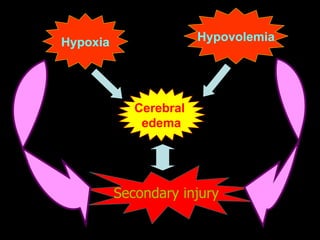
3. The goal of management is to control factors that raise intracranial pressure like hypoxia, hypotension, and cerebral edema in order to maintain adequate cerebral perfusion pressure and optimize outcomes.