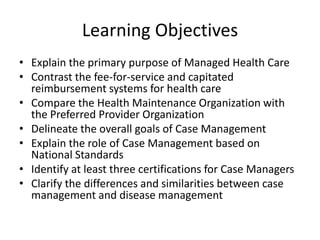
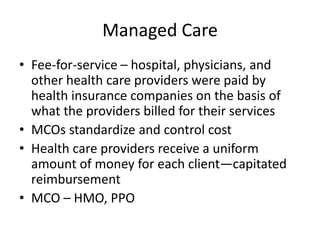
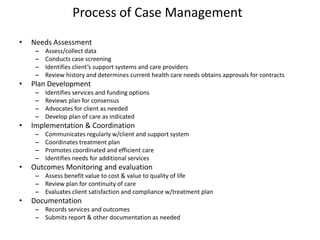
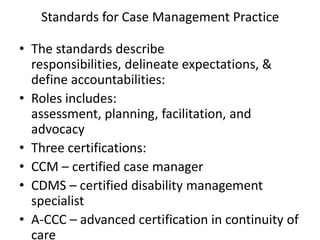
Managed care systems like HMOs and PPOs aim to control healthcare costs by establishing networks of providers and using utilization management. They may use capitated reimbursement instead of fee-for-service. Case management also aims to improve quality of care and reduce costs through coordinated care plans. It involves assessing needs, planning care, implementing and coordinating the plan, and monitoring outcomes. Case managers are certified through examinations in case management, disability management, or advanced care coordination. While similar, case management addresses individual needs while disease management focuses on populations with chronic illnesses.