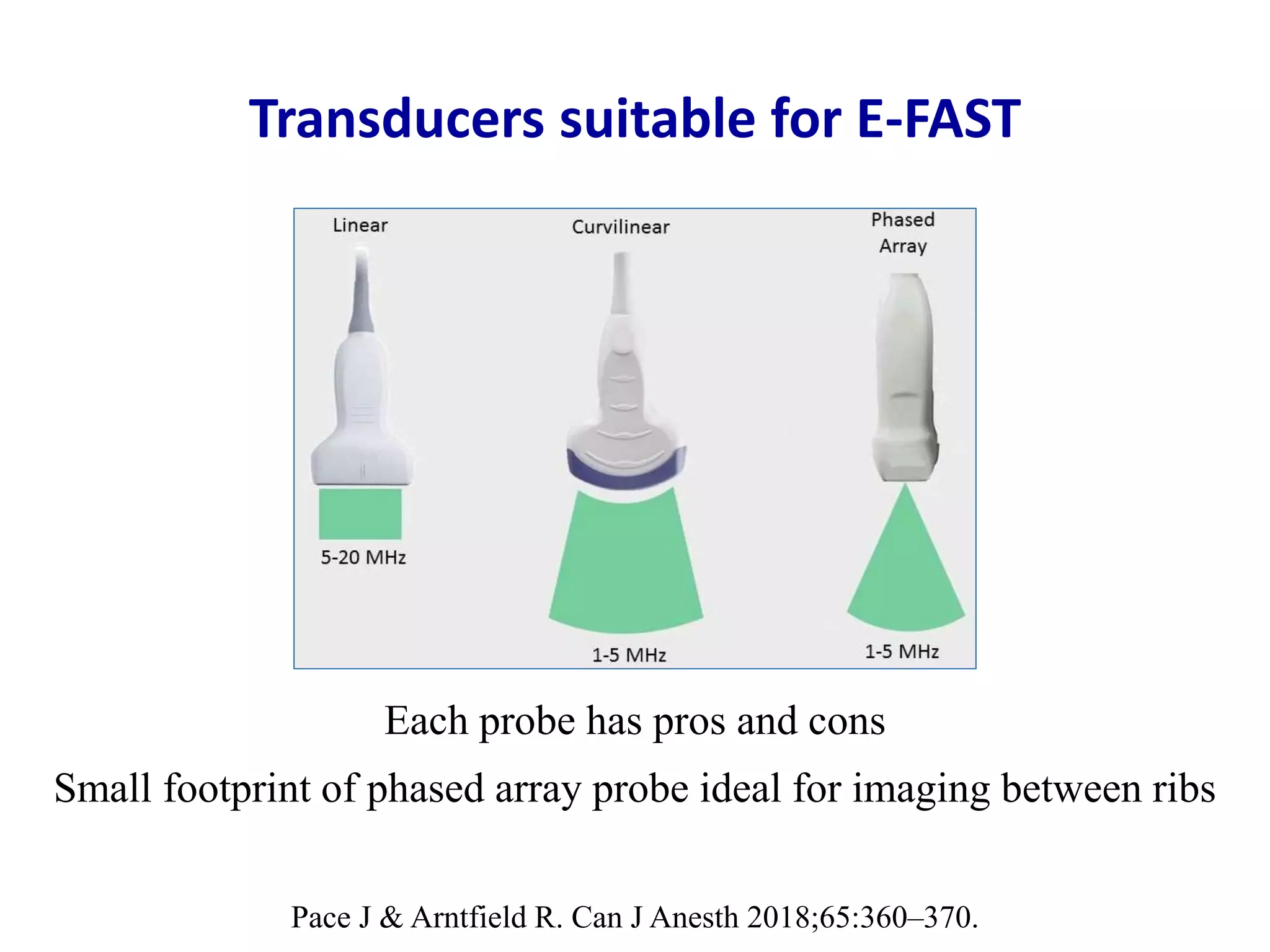
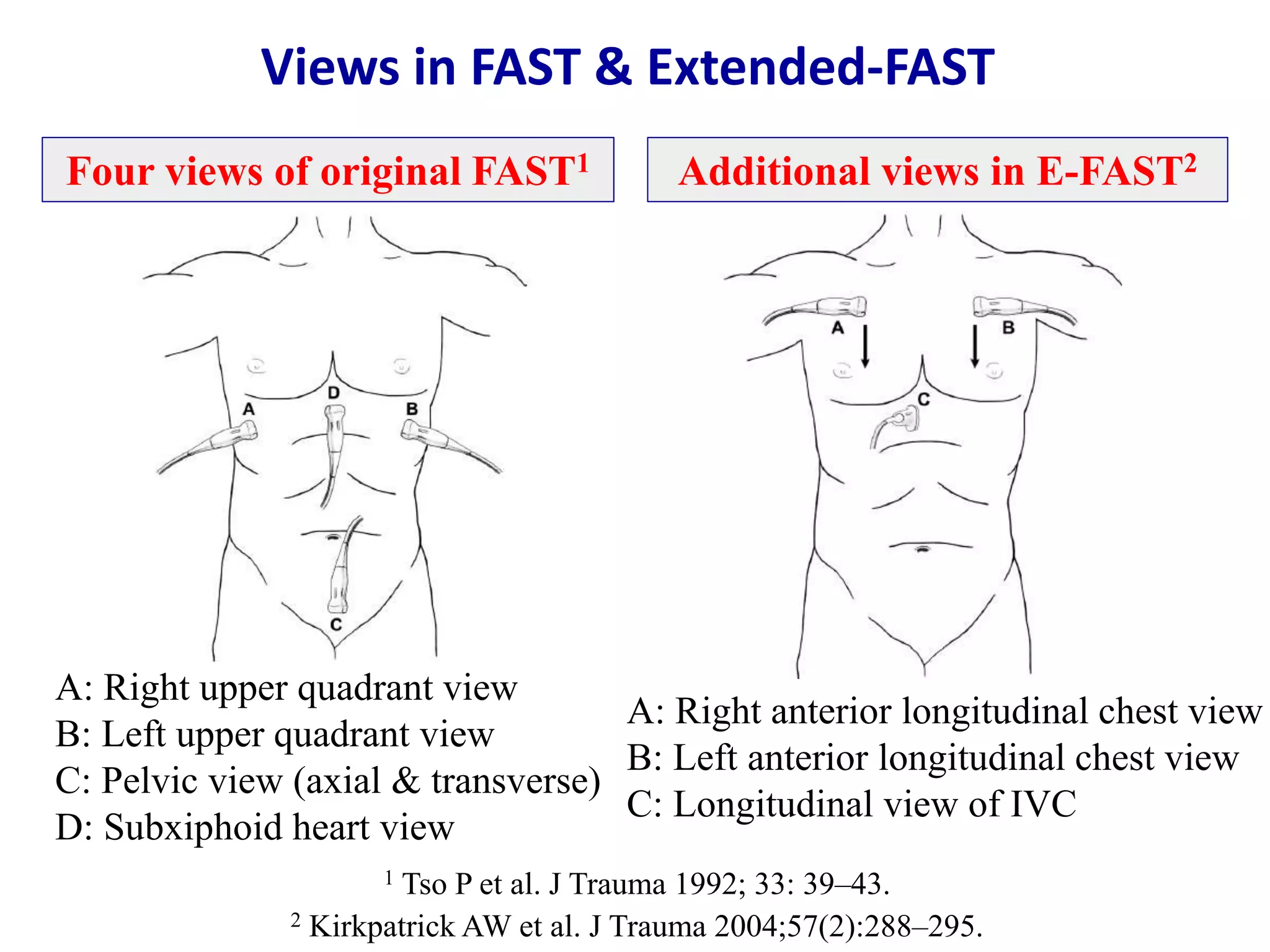
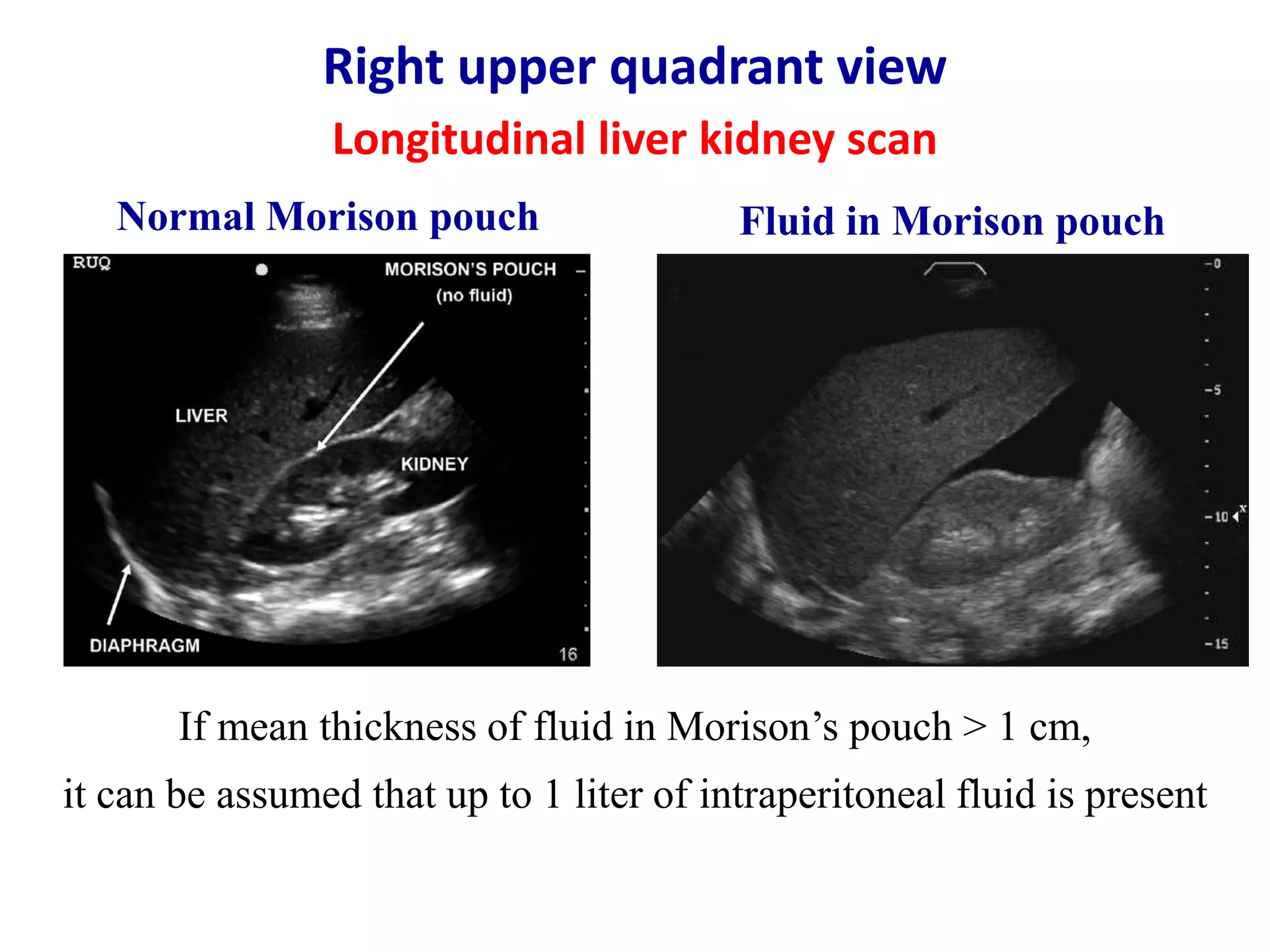
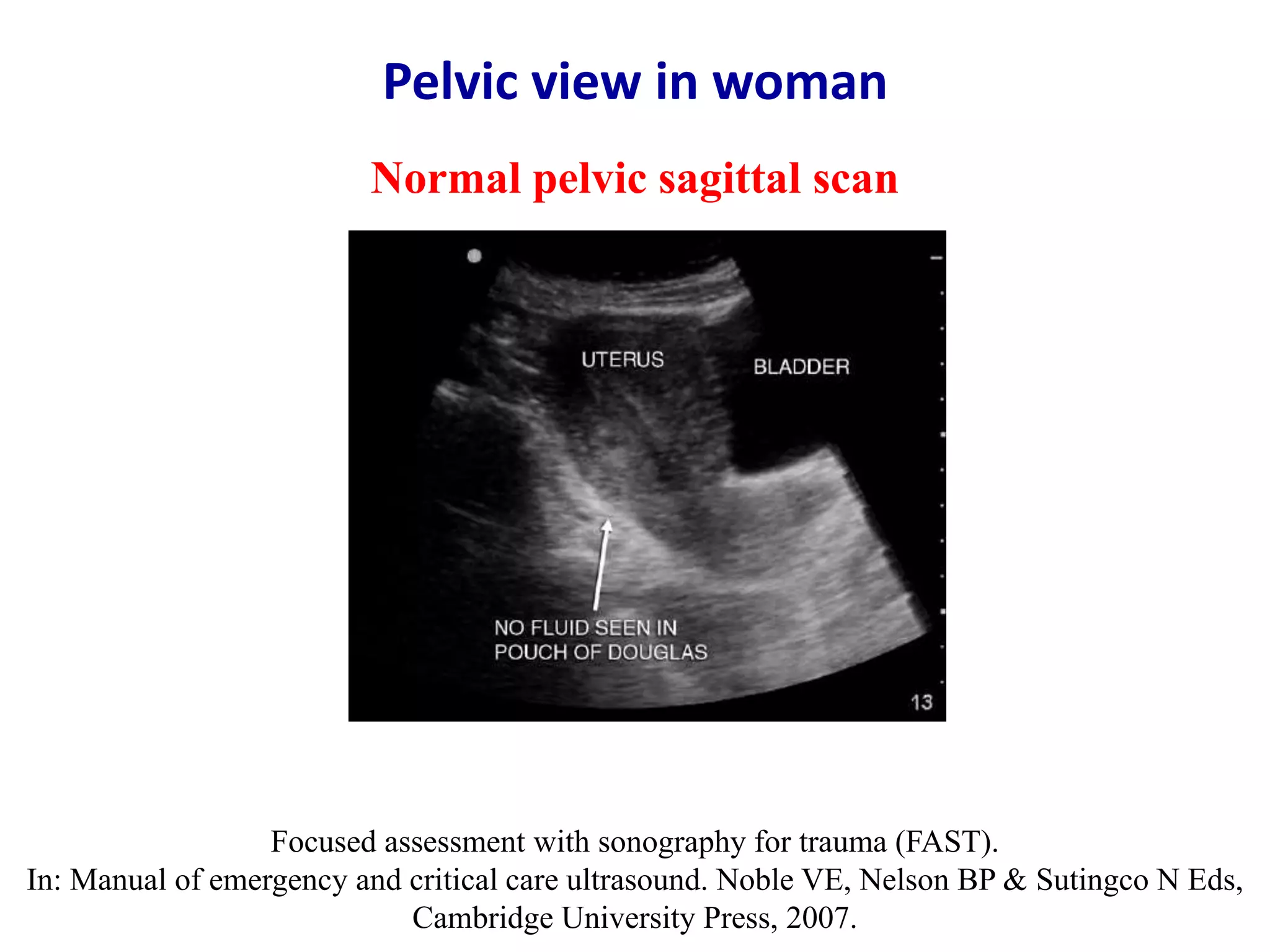
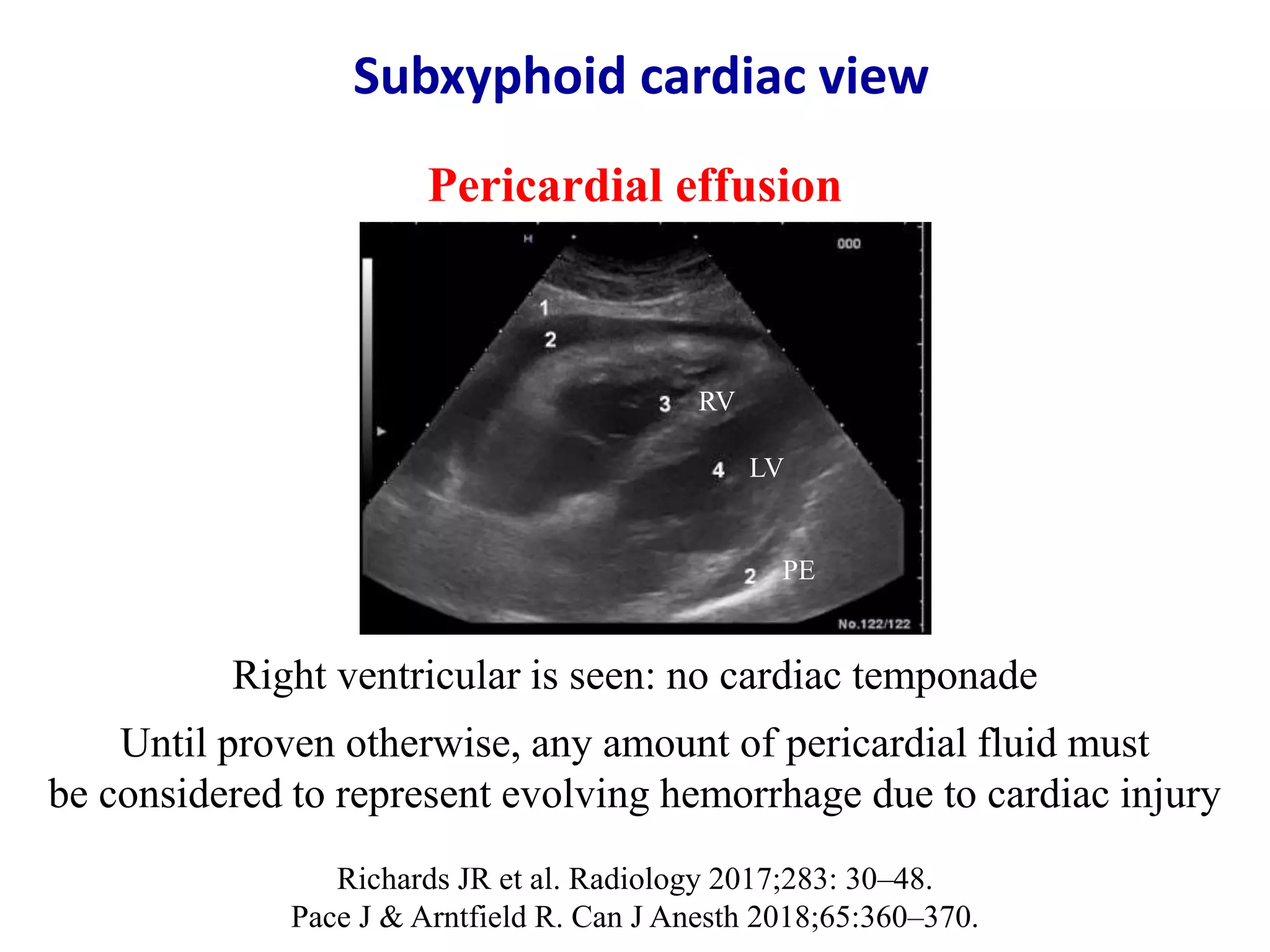
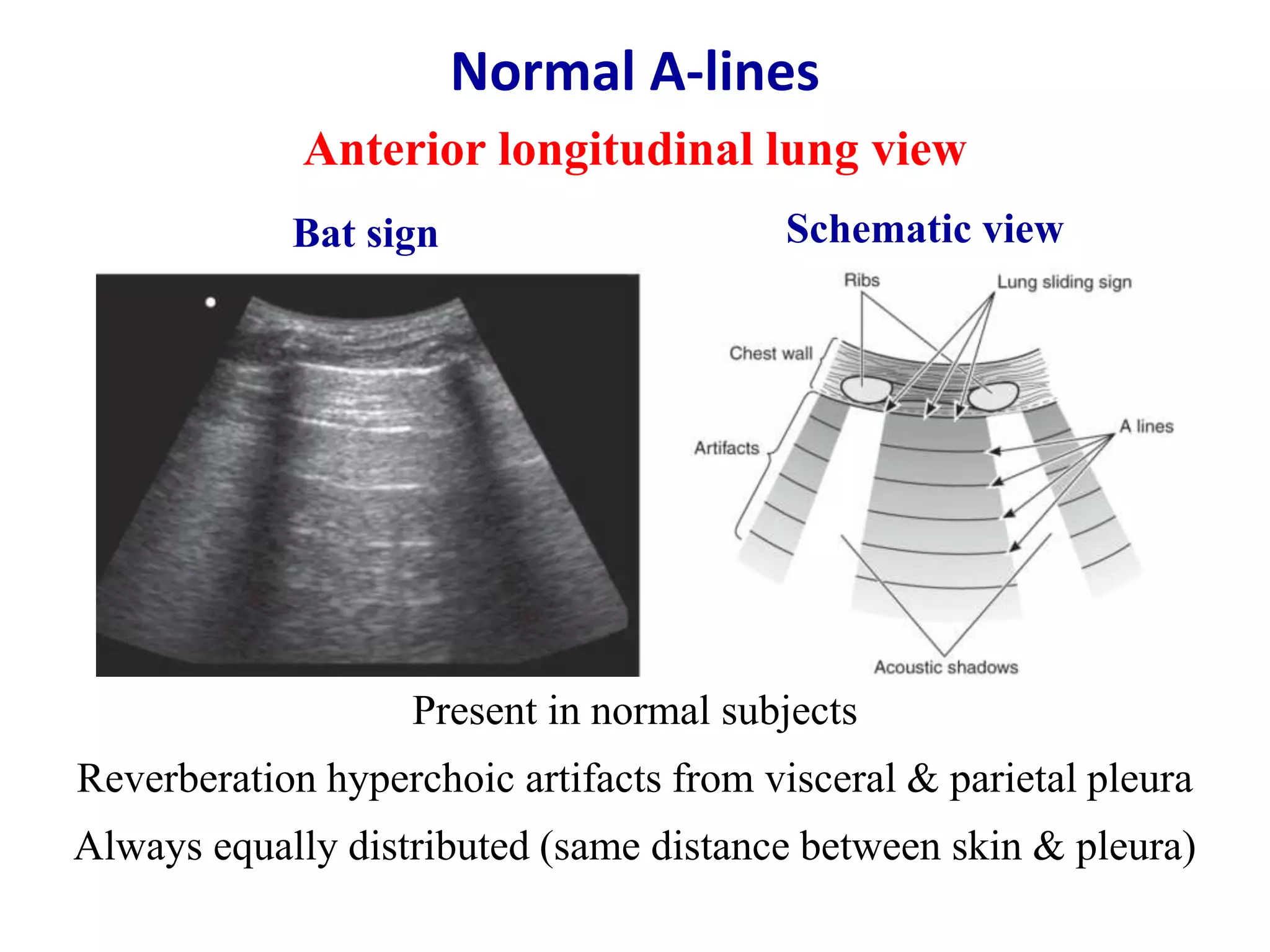
The document discusses extended focused assessment with sonography for trauma (E-FAST), an ultrasound technique used to rapidly detect fluid in body cavities resulting from trauma. It describes the indications, views, techniques, findings and advantages of E-FAST. Key points include that E-FAST can detect blood or fluid in the abdomen, chest or heart within 3-5 minutes without radiation. It is a useful first-line tool to identify life-threatening bleeding but does not replace definitive diagnostic tests if findings are uncertain or positive. E-FAST examination involves six standard views of the abdomen, chest and heart and can be repeated as needed at the bedside to dynamically monitor trauma patients.