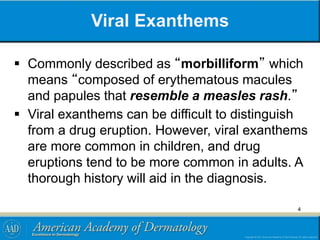
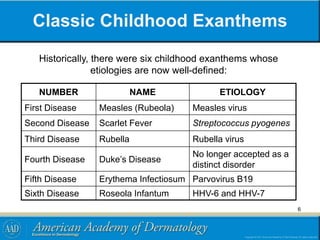
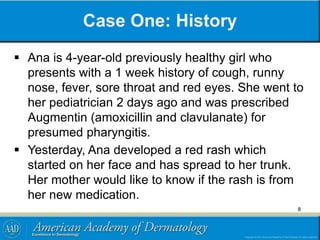
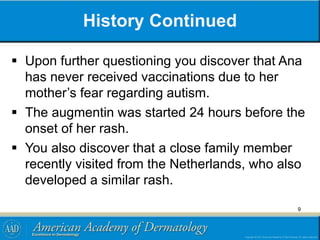
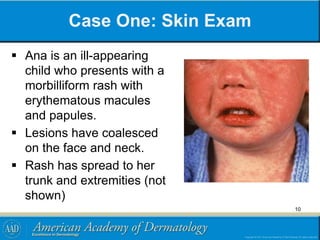
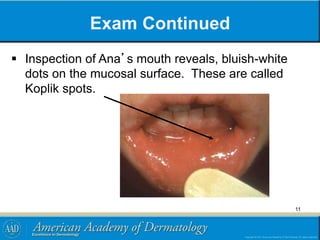
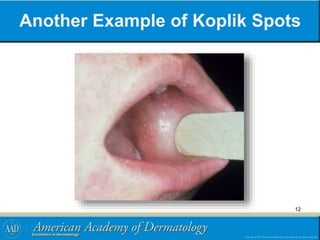
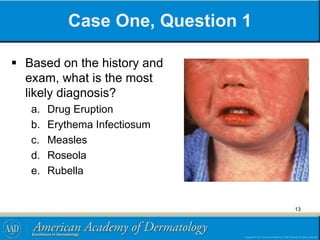
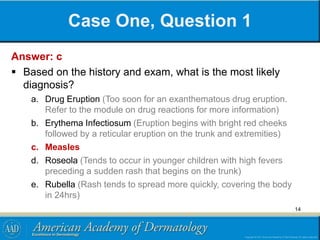
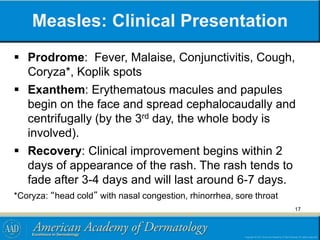
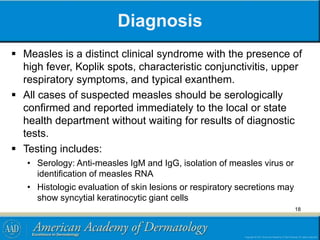
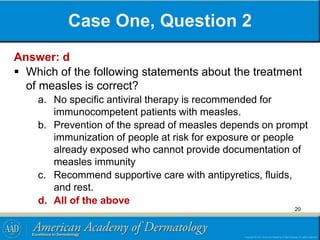
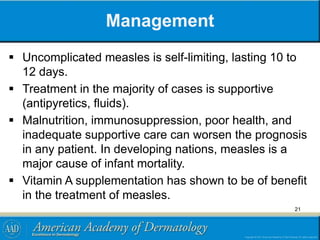
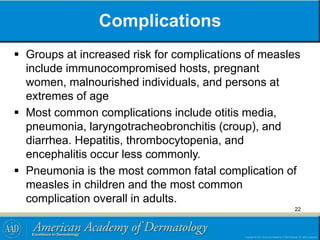
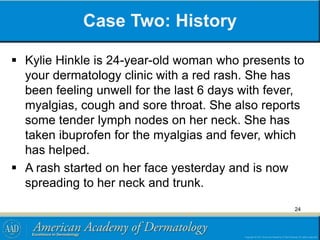
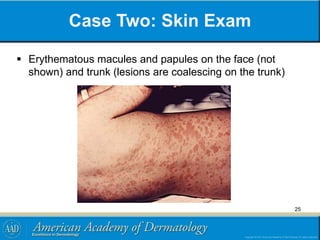
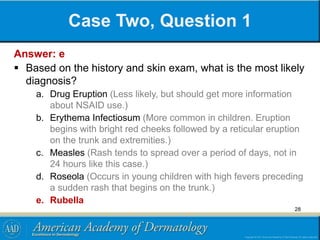
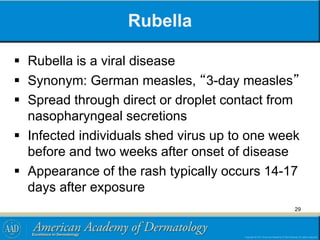
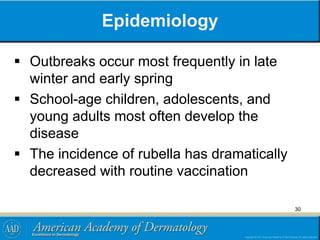
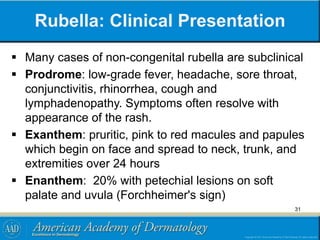
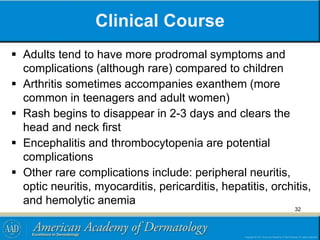
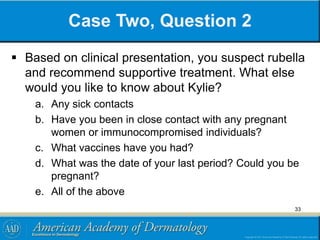
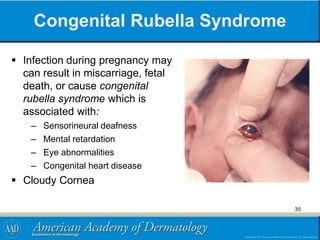
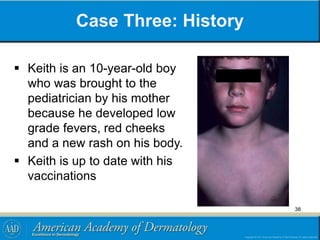
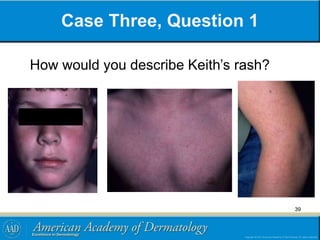
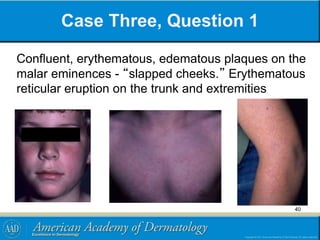
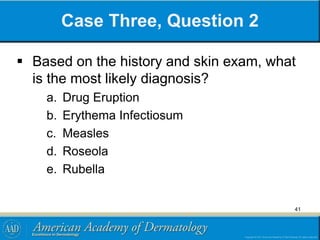
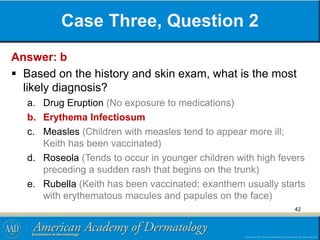
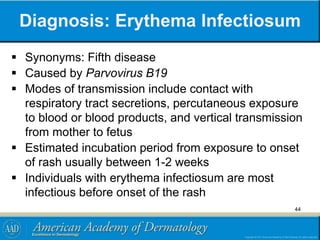
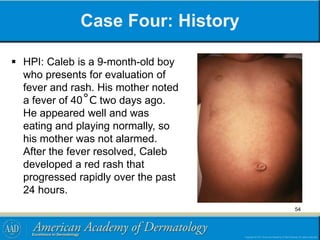
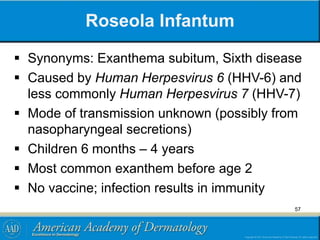
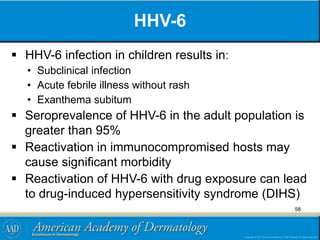
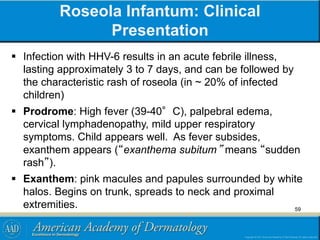
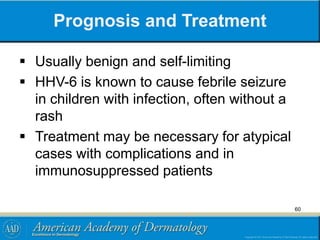
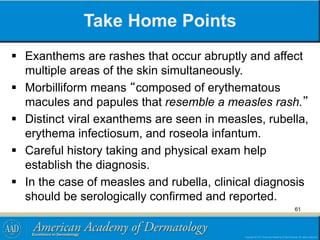
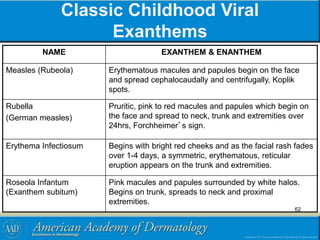
This document provides information on viral exanthems, including goals of recognizing a morbilliform rash and describing presentations of childhood viral exanthems. It defines exanthem and enanthem rashes and describes morbilliform rashes as composed of erythematous macules and papules resembling measles. Classic childhood exanthems are described as measles, scarlet fever, rubella, roseola, and erythema infectiosum. Two case studies are presented - one involving a child with Koplik spots and a rash consistent with measles, and another involving an unvaccinated adult woman with a rash consistent with rubella.

![References
American Academy of Pediatrics. In: Pickering LK, Baker CJ,
Kimberlin DW, Long SS, eds. Red Book: 2009 Report of the
Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL:
American Academy of Pediatrics; 2009:[online]
Barinaga J, Skolnik P. Epidemiology and transmission of measles.
In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA, 2010.
Barinaga J, Skolnik P. Clinical presentation and diagnosis of
measles. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA,
2010.
Bialecki C, Feder HM, Grant-Kels JM. The six classic childhood
exanthems: A review and update. J Am Acad Dermatol. 1989; 21:
891-903.
64](https://image.slidesharecdn.com/viral-exanthems-module-140817015843-phpapp02/85/Viral-exanthems-module-64-320.jpg)