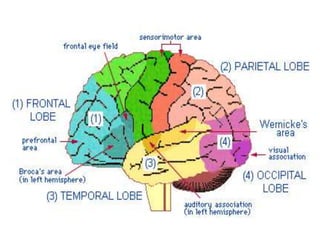
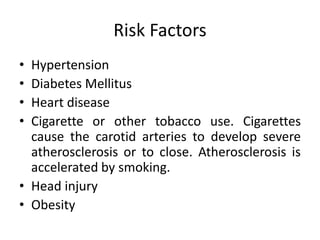
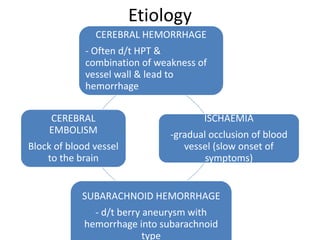
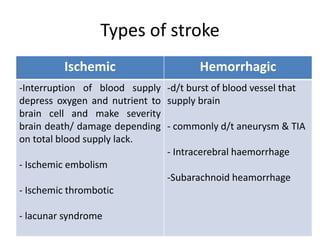
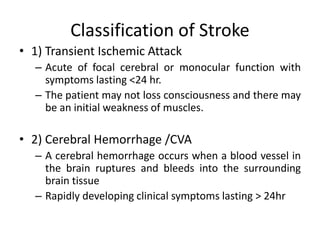
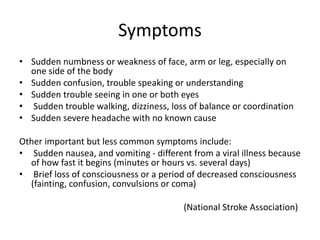
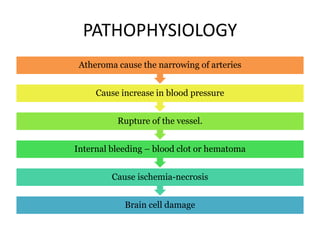
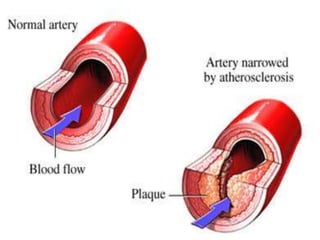
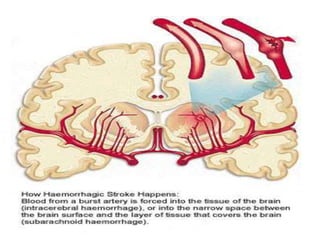
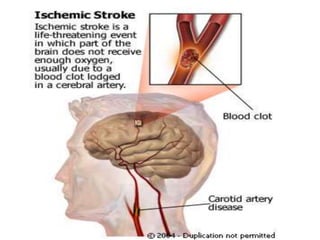
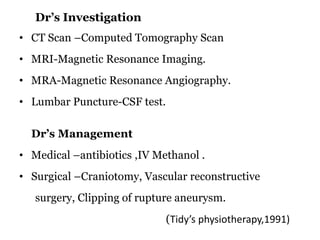
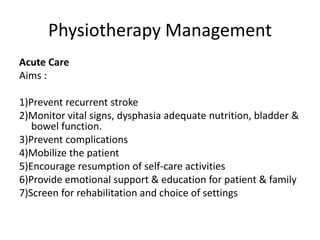
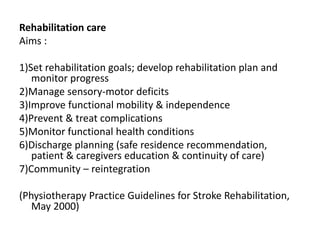
A stroke occurs when a blood vessel in the brain is blocked or ruptures, interrupting blood flow and oxygen to the brain. This causes brain cells to die. The main types of stroke are ischemic, caused by a clot blocking an artery, and hemorrhagic, caused by a ruptured blood vessel. Risk factors include hypertension, diabetes, heart disease, smoking, obesity, and head injuries. Symptoms include sudden numbness, weakness, confusion, trouble seeing or walking. Diagnosis involves CT scans, MRI, or lumbar puncture. Treatment includes medications, surgery, and rehabilitation to regain functions and prevent complications.