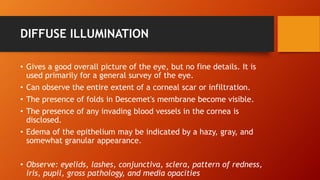
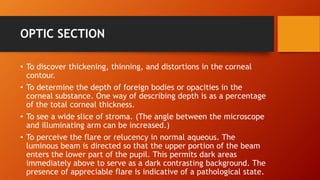
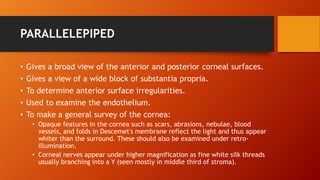
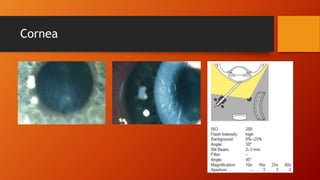
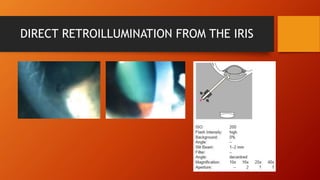
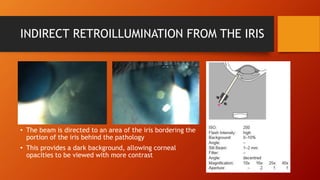
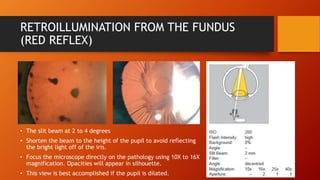
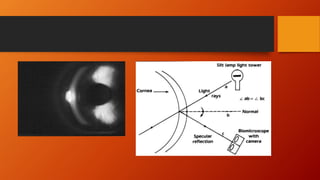
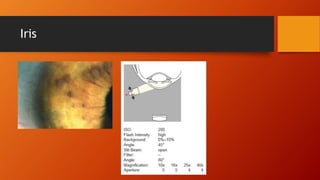
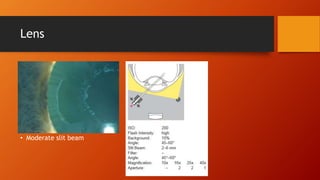
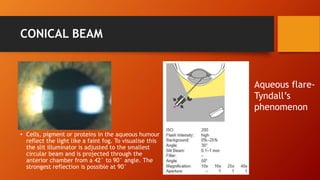
This document describes various methods of illumination used with a slit lamp to examine different parts of the eye. Diffuse illumination allows for a general survey of the eye while optic section, parallelepiped, and retroillumination techniques are used to view specific structures like the cornea, lens, and vitreous in more detail. Different angles of illumination like tangential, conical beam, and oscillatory help observe surface textures, cells in the aqueous humor, and lens opacities. Precise illumination techniques are crucial for comprehensive eye exams.