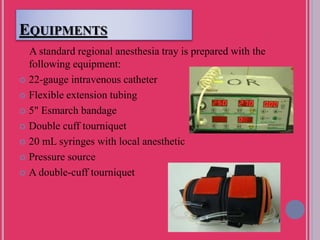
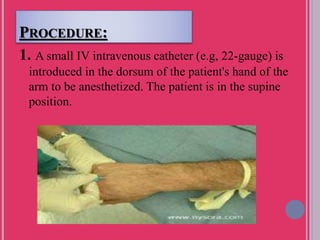
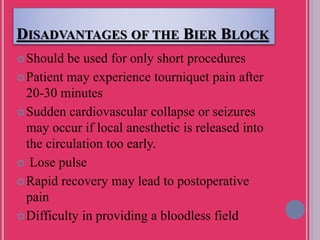
The Bier block, introduced by August Bier in 1908, is a technique for intravenous regional anesthesia primarily used for surgical procedures on the arms and legs below the elbow and knee, respectively. It offers rapid onset of anesthesia with relatively low risks when performed correctly, though it is limited to short procedures and carries potential complications such as tourniquet pain and local anesthetic toxicity. The technique involves the use of a tourniquet and local anesthetic, with careful monitoring of dosage and duration to ensure patient safety.