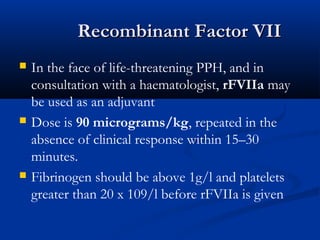
Postpartum haemorrhage (PPH) is the leading cause of maternal mortality worldwide, accounting for 34% of deaths in developing countries. PPH is defined as blood loss of 500ml or more following a vaginal birth or 1000ml or more following a caesarean section. Early identification of at-risk patients and active management of the third stage of labour can help prevent PPH. Diagnosis involves communication, resuscitation with fluids and blood products, monitoring, and investigating the cause of bleeding. Treatment focuses on bimanual compression, uterotonic drugs, surgical haemostasis procedures if conservative measures fail, and consideration of recombinant factor VII.