Small intestinal inflammation and infection
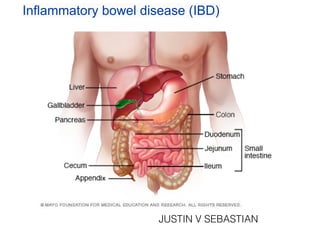
- 1. Inflammatory bowel disease (IBD) JUSTIN V SEBASTIAN
- 2. Infl ammatory bowel disease (IBD) is an umbrella term used to describe disorders that involve chronic in fl ammation of digestive tract. Types of IBD include : • Ulcerative colitis. This condition causes long-lasting in fl ammation and sores (ulcers) in the innermost lining of large intestine (colon) and rectum . • Crohn's disease. This type of IBD is characterised by in fl ammation of the lining of digestive tract, which often spreads deep into affected tissues . Both ulcerative colitis and Crohn's disease usually involve severe diarrhoea, abdominal pain, fatigue and weight loss.
- 3. Cause s • The exact cause of in fl ammatory bowel disease remains unknown . • One possible cause is an immune system malfunction. When immune system tries to fi ght off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too. • Heredity also seems to play a role in that IBD is more common in people who have family members with the disease. However, most people with IBD don't have this family history.
- 4. Risk factor s • Age. Most people who develop IBD are diagnosed before they're 30 years old . • Race or ethnicity. Although whites have the highest risk of the disease, it can occur in any race . • Family history. Persons are at higher risk if there is a close relative — such as a parent, sibling or child — with the disease . • Cigarette smoking. Cigarette smoking is the most important controllable risk factor for developing Crohn's disease . • Non-steroidal anti-in fl ammatory medications. These include ibuprofen (Advil, Motrin IB, others). These medications may increase the risk of developing IBD or worsen disease in people who have IBD . • Environment. Living in an industrialised country, more likely to develop IBD. Therefore, it may be that environmental factors.
- 5. Pathophysiology Ulcerative colitis affects the super fi cial mucosa of the colon and is characterised by multiple ulcerations, diffuse in fl ammations, and desquamation or shedding of the colonic epithelium . Bleeding occurs as a result of the ulcerations. The mucosa becomes edematous and in fl amed. The lesions are contiguous, occurring one after the other. Abscesses form, and in fi ltrate is seen in the mucosa and submucosa with clumps of neutrophils in the crypt lumens (ie, crypt abscesses). The disease process usually begins in the rectum and spreads proximally to involve the entire colon. Eventually, the bowel narrows, shortens, and thickens because of muscular hypertrophy and fat deposits.
- 6. Symptom s In fl ammatory bowel disease symptoms vary, depending on the severity of in fl ammation and where it occurs. Symptoms may range from mild to severe. Patient may likely to have periods of active illness followed by periods of remission . Signs and symptoms that are common to both Crohn's disease and ulcerative colitis include : • Diarrhoe a • Fever and fatigu e • Abdominal pain and crampin g • Blood in stoo l • Reduced appetit e • Unintended weight loss
- 7. Complication s Ulcerative colitis and Crohn's disease have some complications in common and others that are speci fi c to each condition. Complications found in both conditions may include : • Colon cancer. Having IBD increases risk of colon cancer . • Medication side effects. Certain medications for IBD are associated with a small risk of developing certain cancers. Corticosteroids can be associated with a risk of osteoporosis, high blood pressure and other conditions . • Primary sclerosing cholangitis. In this condition, in fl ammation causes scars within the bile ducts, eventually making them narrow and gradually causing liver damage.
- 8. Complications of ulcerative colitis may include : • Toxic megacolon. Ulcerative colitis may cause the colon to rapidly widen and swell, a serious condition known as toxic megacolon . • A hole in the colon (perforated colon). A perforated colon most commonly is caused by toxic megacolon, but it may also occur on its own . • Severe dehydration. Excessive diarrhoea can result in dehydration.
- 9. Diagnosis Blood test s • Tests for anaemia or infection. Doctor may suggest blood tests to check for anaemia — a condition in which there aren't enough red blood cells to carry adequate oxygen to tissues — or to check for signs of infection from bacteria or viruses . • Fecal occult blood test. Patient may need to provide a stool sample so that doctor can test for hidden blood in stool . Imaging procedure s • X-ray. If there severe symptoms, doctor may use a standard X-ray of abdominal area to rule out serious complications, such as a perforated colon . • Computerized tomography (CT) scan. patient may have a CT scan — a special X- ray technique that provides more detail than a standard X-ray does . • Magnetic resonance imaging (MRI). An MRI is particularly useful for evaluating a fi stula around the anal area (pelvic MRI) or the small intestine (MR enterography).
- 10. Endoscopic procedures • Colonoscopy. This exam allows doctor to view entire colon using a thin, fl exible, lighted tube with an attached camera. During the procedure, doctor can also take small samples of tissue (biopsy) for laboratory analysis . • Flexible sigmoidoscopy. Doctor uses a slender, fl exible, lighted tube to examine the rectum and sigmoid, the last portion of colon . • Upper endoscopy. In this procedure, doctor uses a slender, fl exible, lighted tube to examine the esophagus, stomach and fi rst part of the small intestine (duodenum).
- 11. Treatmen t Anti-infl ammatory drug s Anti-in fl ammatory drugs are often the fi rst step in the treatment of in fl ammatory bowel disease. Anti-in fl ammatories include corticosteroids and aminosalicylates . Immune system suppressor s These drugs work in a variety of ways to suppress the immune response that releases in fl ammation-inducing chemicals in the intestinal lining. For some people, a combination of these drugs works better than one drug alone . Some examples of immunosuppressant drugs include azathioprine (Azasan, Imuran), cyclosporine (Gengraf, Neoral, Sandimmune) and methotrexate (Trexall) . Antibiotic s Antibiotics may be used in addition to other medications or when infection is a concern — in cases of perianal Crohn's disease, for example. Frequently prescribed antibiotics include cipro fl oxacin (Cipro) and metronidazole (Flagyl).
- 12. Other medications and supplement s • Antidiarrheal medications. A fi ber supplement — such as psyllium powder (Metamucil) or methyl-cellulose (Citrucel) — can help relieve mild to moderate diarrhea by adding bulk to stool . • Pain relievers. For mild pain, doctor may recommend acetaminophen (Tylenol, others) . • Iron supplements. If there chronic intestinal bleeding, may develop iron de fi ciency anaemia and need to take iron supplements . • Calcium and vitamin D supplements. Crohn's disease and steroids used to treat it can increase risk of osteoporosis, so may need to take a calcium supplement with added vitamin D.
- 13. Surger y If diet and lifestyle changes, drug therapy, or other treatments don't relieve IBD signs and symptoms, doctor may recommend surgery . • Surgery for ulcerative colitis. Surgery can often eliminate ulcerative colitis. But that usually means removing entire colon and rectum (proctocolectomy). In most cases, this involves a procedure called an ileal pouch anal anastomosis. This procedure eliminates the need to wear a bag to collect stool. Surgeon constructs a pouch from the end of small intestine. The pouch is then attached directly to anus, allowing to expel waste relatively normally.
- 15. Nursing Diagnosis 1. Diarrhoea may be related to Inflammation, irritation, or malabsorption of the bowel. Nursing Interventions •Ascertain onset and pattern of diarrhea •Observe and record stool frequency, characteristics, amount, and precipitating factors. •Observe for presence of associated factors, such as fever, chills, abdominal pain,cramping, bloody stools, emotional upset, physical exertion and so forth. •Promote bedrest.
- 16. 2. Risk for Deficient Fluid Volume may be related to excessive losses through normal routes (severe frequent diarrhea, vomiting) Nursing Interventions •Note possible conditions or processes that may lead to deficits such as fluid loss, limited intake, fluid shifts, environmental factor. •Monitor I&O. Note number, character, and amount of stools; estimate insensible fluid losses (diaphoresis). Measure urine specific gravity; observe for oliguria. •Assess vital signs (BP, pulse, temperature). •Observe for excessively dry skin and mucous membranes, decreased skin turgor, slowed capillary refill.
- 17. 3. Acute Pain may be related to Hyper-peristalsis, prolonged diarrhea, skin/tissue irritation, perirectal excoriation, fissures, fistulas Nursing Interventions •Assess reports of abdominal cramping or pain, noting location, duration, intensity (0–10 scale). Investigate and report changes in pain characteristics. •Review factors that aggravate or alleviate pain. •Encourage patient to assume position of comfort (knees flexed). •Provide comfort measures (back rub, reposition) and diversional activities.
- 18. 4. Anxiety may be related to Physiological factors/ sympathetic stimulation (inflammatory process) Nursing Interventions •Review physiological factors, such as active medical condition; recent or ongoing stressors. •Observe and note behavioral clues (restlessness, irritability, withdrawal, lack of eye contact, demanding behavior). •Encourage verbalization of feelings. Provide feedback. •Provide a calm, restful environment.
- 19. ENTERITIS
- 20. ○ ENTERITIS IS THE INFLAMMATION OF THE SMALL INTESTINE ENTERO=Small intestine +ITIS=Inflammation
- 21. CAUSES ○ It is most commonly caused by contaminated food and drinks by pathogenic microorganism such as norovirus , rotavirus, campylobacter, salmonella e.t.c (INFECTIOUS ENTERITIS) ○ Autoimmune diseases- crohn’s disease (regional enteritis 40%) and Coeliac disease-autoimmune reaction to gluten ○ Vascular disease( Ischemic enteritis) due to blood flow.
- 22. ○ It may be medication induced such as NSAIDs ○ Alcohol or drug induced such as cocaine ○ Inflammation after radiation therapy (treatment of cancer) it is radiation enteritis. In early stage it causes destruction of crypt epithelium in chronic form majority of intestine
- 23. SIGNS AND SYMPTOMS Signs and symptoms of enteritis are highly variable and vary based on the specific cause and other factors such as individual variance and stage of disease. • Abdominal pain • Cramping • Diarrhoea • Nausea • Vomiting • Dehydration • Fever • Weight loss • Pain, bleeding, Mucus discharge from rectum
- 24. ACUTE ENTERITIS ○ Acute inflammation of the small intestine ○ Etiology:-many infections(cholera, staphylococcal, typhoid, sepsis) alimentary toxication (salmonellosis, botulism) poisoning, allergic
- 25. CHRONIC ENTERITIS ○ It is the chronic inflammation of the small intestine It may be:-hemorrhagic ,necrotic and granulomatous
- 26. COMPLICATIONS ○ Dehydration ○ Excessive thirst ○ Weakness ○ Fatigue ○ Lethargy ○ Poor urine output and urine is dark colour ○ dizziness
- 27. DIAGNOSIS ○ A medical history, physical examination and tests such as blood counts, stool cultures, CT scans, MRIs, PCRs, colonoscopies and upper endoscopies may be used in order to perform a differential diagnosis. A biopsy may be required to obtain a sample for histopathology.
- 30. TREATMENT ○ For mild cases treatment is not need, it recovers within two to three days ○ In cases where symptoms persist or severe cases treatment is needed ○ Oral rehydration solution(ORS) is used in cases of diarrhoea ○ In infectious enteritis antibiotics are taken.
- 31. Malabsorption syndrome • The main role of small intestine is to absorb nutrients from the food you eat into your bloodstream. • Malabsorption syndrome refers to a number of disorders in which the small intestine can’t absorb enough of certain nutrients and fluids. • Nutrients that the small intestine often has trouble absorbing can be macronutrients (proteins, carbohydrates, and fats), micronutrients (vitamins and minerals), or both.
- 32. Causes of malabsorption syndrome Factors that may cause malabsorption syndrome include: • damage to the intestine from infection, inflammation, trauma, or surgery • prolonged use of antibiotics • other conditions such as celiac disease, Crohn’s disease, chronic pancreatitis, or cystic fibrosis • lactase deficiency, or lactose intolerance • certain defects that are congenital, or present at birth, such as biliary atresia, when the bile ducts don’t develop normally and prevent the flow of bile from the liver • diseases of the gallbladder, liver, or pancreas • parasitic diseases • radiation therapy, which may injure the lining of the intestine • certain drugs that may injure the lining of the intestine, such as tetracycline, colchicine, or cholestyramine
- 34. Symptoms of malabsorption syndrome Symptoms of malabsorption syndrome are caused when unabsorbed nutrients pass through the digestive tract. Many symptoms differ depending on the specific nutrient or nutrients that aren’t being absorbed properly. Other symptoms are a result of a deficiency of that nutrient, which is caused by its poor absorption. You may have the following symptoms if you’re unable to absorb fats, protein, or certain sugars or vitamins: • Fats. You may have light-colored, foul-smelling stools that are soft and bulky. Stools are difficult to flush and may float or stick to the sides of the toilet bowl. • Protein. You may have dry hair, hair loss, or fluid retention. Fluid retention is also known as edema and will manifest as swelling. • Certain sugars. You may have bloating, gas, or explosive diarrhea. • Certain vitamins. You may have anemia, malnutrition, low blood pressure, weight loss, or muscle wasting.
- 35. Diagnosing malabsorption syndrome Your doctor may suspect malabsorption syndrome if you have chronic diarrhea or nutrient deficiencies, or have lost a significant amount of weight despite eating a healthy diet. Certain tests are used to confirm the diagnosis. These tests may include: Stool tests Stool tests can measure fat in samples of stool, or feces. These tests are the most reliable because fat is usually present in the stool of someone with malabsorption syndrome. Blood tests These tests measure the level of specific nutrients in your blood, such as vitamin B-12, vitamin D, folate, iron, calcium, carotene, phosphorus, albumin, and protein.
- 36. Breath tests Breath tests can be used to test for lactose intolerance. If lactose isn’t being absorbed, it enters the colon. Bacteria in the colon break down the lactose and produce hydrogen gas. The excess hydrogen is absorbed from your intestine, into your bloodstream, and then into your lungs. You’ll then exhale the gas. Imaging tests Imaging tests, which take pictures of your digestive system, may be done to look for structural problems. For instance, your doctor could request a CT scan to look for thickening of the wall of your small intestine, which could be a sign of Crohn’s disease. Biopsy You may have a biopsy if your doctor suspects you have abnormal cells in the lining of your small intestine.
- 37. Treatment • Doctor will likely start your treatment by addressing symptoms such as diarrhea. Medications such as loperamide can help. • Doctor will also want to replace the nutrients and fluids that body has been unable to absorb. And they may monitor for signs of dehydration, which can include increased thirst, low urine output, and dry mouth, skin, or tongue. • Doctor will provide care based on the cause of the absorption problem. For instance, if you’re found to have lactose intolerance, doctor will likely advise to avoid milk and other dairy products or take a lactase enzyme tablet. At this point, doctor may refer you to a dietitian. Dietitian may recommend: • Enzyme supplements. These supplements can help your body absorb the nutrients it can’t absorb on its own. • Vitamin supplements. dietitian may recommend high doses of vitamins or other nutrients to make up for those that are not being absorbed by intestine. • Diet changes. dietitian may adjust diet to increase or decrease certain foods or nutrients. For instance, patient may be advised to avoid foods high in fat to decrease diarrhea, and increase foods high in potassium to help balance electrolytes.
- 38. Nursing Diagnosis • Diarrhea related to indigestion secondary to malabsorption • Imbalanced nutrition less than body requirement related to indigestion secondary to diarrhea. • Fluid and electrolyte imbalance related to indigestion secondary to malabsorption • Knowledge deficit related to hospitalisation and malabsorption disease • Fear and anxiety related to hospitalisation
- 39. Nursing Intervention •Improvement of nutritional status by appropriate diet planning and supplementation of deficient nutrition. •Restoration of fluid and electrolyte balance by oral and parenteral therapy •Continuous monitoring and recording of patient’s condition •Relief of pain by medication and antidiarrheal agents for diarrhea as prescribed by doctor •Maintenance of skin integrity specially perineal area •Health education to parents about general cleanliness, nutrition, hydration, danger sign, home care and follow-up, for necessary medical help. •Relief of fear and anxiety about long term illness and hospitalisation by appropriate explanation, reassurance and necessary support.
- 41. Intestinal Obstruction Intestinal obstruction exists when blockage prevents the normal fl ow of intestinal contents through the intestinal tract. Two types of processes can impede this fl ow. Mechanical obstruction: An intraluminal obstruction or a mural obstruction from pressure on the intestinal walls occurs. Examples are intussusception, polypoid tumors and neoplasms, stenosis, strictures, adhesions, hernias, and abscesses. Functional obstruction: The intestinal musculature cannot propel the contents along the bowel. Examples are amyloidosis, muscular dystrophy, neurologic disorders such as Parkinson’s disease. The blockage also can be temporary and the result of the manipulation of the bowel during surgery.
- 42. • The obstruction can be partial or complete. Its severity depends on the region of bowel affected, and especially the degree to which the vascular supply to the bowel wall is disturbed. • Most bowel obstructions occur in the small intestine. Adhesions are the most common cause of small bowel obstruction, followed by hernias and neoplasms. Other causes include intussusception, volvulus (ie, twisting of the bowel), and paralytic ileus. • About 15% of intestinal obstructions occur in the large bowel; most of these are found in the sigmoid colon. The most common causes are carcinoma, diverticulitis, in fl ammatory bowel disorders, and benign tumors.
- 43. SMALL BOWEL OBSTRUCTION Pathophysiology Intestinal contents accumulate above the intestinal obstruction. Abdominal distention and retention of fl uid Reduce the absorption of fl uids Stimulate more gastric secretion. Increasing distention and pressure within the intestinal lume n Decrease in venous and arteriolar capillary pressure. Edema, congestion, necrosi s Rupture or perforation of the intestinal wal l Peritonitis.
- 44. Clinical Manifestations • The initial symptom is usually crampy pain that is wavelike and colicky. • The patient may pass blood and mucus, but no fecal matter and no fl atus. • Vomiting occurs. • If the obstruction is complete, the peristaltic waves initially become extremely vigorous and eventually assume a reverse direction, with the intestinal contents propelled toward the mouth instead of toward the rectum. • If the obstruction is in the ileum, fecal vomiting takes place. • First, the patient vomits the stomach contents, then the bile-stained contents of the duodenum and the jejunum, and fi nally, with each paroxysm of pain, the darker, fecal-like contents of the ileum. • If the obstruction continues uncorrected, hypovolemic shock occurs from dehydration and loss of plasma volume.
- 45. Assessment and Diagnostic Findings • Abdominal x-ray studies show abnormal quantities of gas, fl uid, or both in the bowel. • Laboratory studies (ie, electrolyte studies and a complete blood cell count) reveal a picture of dehydration, loss of plasma volume, and possible infection.
- 46. Medical Management Decompression of the bowel through a nasogastric or small bowel tube is successful in most cases. When the bowel is completely obstructed, the possibility of strangulation warrants surgical intervention. Before surgery, intravenous therapy is necessary to replace the depleted water, sodium, chloride, and potassium. The surgical treatment of intestinal obstruction depends largely on the cause of the obstruction. In the most common causes of obstruction, such as hernia and adhesions, the surgical procedure involves repairing the hernia or dividing the adhesion to which the intestine is attached. In some instances, the portion of affected bowel may be removed and an anastomosis performed.
- 47. Nursing Management • Nursing management of the nonsurgical patient with a small bowel obstruction includes maintaining the function of the nasogastric tube, assessing and measuring the nasogastric output, assessing for fluid and electrolyte imbalance, monitoring nutritional status, and assessing improvement (eg, return of normal bowel sounds, decreased abdominal distention, subjective improvement in abdominal pain and tenderness, passage of flatus or stool). • The nurse reports discrepancies in intake and output, worsening of pain or abdominal distention, and increased nasogastric output. • If the patient’s condition does not improve, the nurse prepares him or her for surgery. • Nursing care of the patient after surgical repair of a small bowel obstruction is similar to that for other abdominal surgeries
- 48. LARGE BOWEL OBSTRUCTION Pathophysiology As in small bowel obstruction, large bowel obstruction results in an accumulation of intestinal contents, fluid, and gas proximal to the obstruction. Obstruction in the large bowel can lead to severe distention and perforation unless some gas and fluid can flow back through the ileal valve. Large bowel obstruction, even if complete, may be undramatic if the blood supply to the colon is not disturbed. If the blood supply is cut off, however, intestinal strangulation and necrosis (ie, tissue death) occur; this condition is life threatening. In the large intestine, dehydration occurs more slowly than in the small intestine because the colon can absorb its fluid contents and can distend to a size considerably beyond its normal full capacity.
- 49. Clinical Manifestations • Large bowel obstruction differs clinically from small bowel obstruction in that the symptoms develop and progress relatively slowly. • In patients with obstruction in the sigmoid colon or the rectum, constipation may be the only symptom for days. • Eventually, the abdomen becomes markedly distended, loops of large bowel become visibly outlined through the abdominal wall, and the patient has crampy lower abdominal pain. • Finally, fecal vomiting develops. Symptoms of shock may occur.
- 50. Assessment and Diagnostic Findings Diagnosis is based on symptoms and on x-ray studies. Abdominal x-ray studies (flat and upright) show a distended colon. Barium studies are contraindicated.
- 51. Medical Management • A colonoscopy may be performed to untwist and decompress the bowel. • A cecostomy, in which a surgical opening is made into the cecum, may be performed for patients who are poor surgical risks and urgently need relief from the obstruction. The procedure provides an outlet for releasing gas and a small amount of drainage. • A rectal tube may be used to decompress an area that is lower in the bowel. • The usual treatment, however, is surgical resection to remove the obstructing lesion. • A temporary or permanent colostomy may be necessary. An ileoanal anastomosis may be performed if it is necessary to remove the entire large colon.
- 53. Nursing Management • The nurse’s role is to monitor the patient for symptoms that indicate that the intestinal obstruction is worsening and to provide emotional support and comfort. • The nurse administers intra- venous fluids and electrolytes as prescribed. • If the patient’s condition does not respond to nonsurgical treatment, the nurse prepares the patient for surgery. • This preparation includes pre- operative teaching as the patient’s condition indicates. • After surgery, general abdominal wound care and routine post operative nursing care are provided.
- 55. Bowel Perforation • Bowel perforations occur when a hole is made in this lining, often as a result of colon surgery or serious bowel disease. • A hole in the colon then allows the contents of the colon to leak into the usually sterile contents of abdominal cavity. • Perforation of the bowel is considered a medical emergency and requires immediate treatment.
- 56. Causes Bowel perforations may occur spontaneously (unexpectedly) as a result of a medical condition or instead be a complication of various diagnostic and surgical procedures that accidentally create a hole in the colon. Trauma, especially blunt trauma to the abdomen, is also an important cause of bowel perforations. Procedure-Associated Causes • Enema: An improperly or forcefully inserted rectal tube for an enema can rip or push through the colon lining. • Bowel preparation for colonoscopy: Rarely, the bowel preparation for a colonoscopy can result in a perforation. This is more common in people with a history of constipation. • Sigmoidoscopy: Although the endoscope for a flexible sigmoidoscopy is flexible, perforation remains a risk, but a rare one. • Colonoscopy: The tip of the endoscope has the potential to push through the inner lining of the colon, although this is a rare complication. • Abdominal or pelvic surgery: Particularly, colon surgery as for colon cancer may be a risk for perforation
- 57. Spontaneous Causes Causes of spontaneous bowel perforation (those unrelated to surgery or procedures) include: • Inflammatory bowel disease/colitis such as Crohn's disease and ulcerative colitis. • Severe bowel obstruction, especially when the colon is "weakened" by diverticular disease, or cancer • Trauma • Ischemic bowel disease (when the blood supply to the colon is compromised) • Colon cancer • Foreign body ingestion, most commonly due to the ingestion of fish bones, and bone fragments, as well as non-food items • Severe bowel impaction
- 58. Risk Factors Scientists have found that a number of factors may increase risk of developing a bowel perforation. These include both factors involved in surgery or a procedure (iatrogenic causes) and bowel diseases characterised by inflammation. Risk factors may include: • Recent or prior abdominal surgery • Recent or prior pelvic surgery • Age greater than 75 • History of multiple medical problems • Trauma to the abdomen or pelvis (such as in an automobile accident) • A history of diverticular disease • A history of inflammatory bowel disease • Colon cancer • Female sex (women typically have a more flexible colon, which can lead to accidental perforation during medical procedures, including a colonoscopy) • Diagnostic and surgical procedures involving the digestive tract, abdomen, or pelvis.
- 59. Bowel Perforation Symptoms The symptoms of a bowel perforation can vary and may come on slowly or rapidly depending on the underlying cause. Symptoms may include: • Abdominal pain (often severe and diffuse) • Severe abdominal cramping • Bloating • Nausea and vomiting • A change in bowel movements or habits • Rectal bleeding • Fever (usually not immediately) • Chills • Fatigue
- 60. Complications Left untreated, the contents of the bowel can leak out and cause inflammation, infection, and even abscesses in abdomen. The technical name for this is peritonitis. Complications of untreated perforation may include: • Bleeding • Infection (peritonitis and sepsis) • Death Complications depend on a person's general health, as well as the amount of time it has taken to diagnose and treat the perforation.
- 61. Diagnosis If doctor suspects a bowel perforation, he can order tests to confirm her suspicion. • A simple abdominal X-ray may show gas outside the colon but is not often diagnostic. A CT scan of abdomen with or without contrast or a barium enema or swallow may be needed. • A complete blood count may show an elevation of white blood cell count if the perforation has been present for a while, or evidence of anaemia due to bleeding. Small perforations may sometimes take several imaging studies and time to accurately diagnose.
- 62. Treatment • The majority of perforations are surgically repaired. • Depending on the location and size of the tear, the doctor might be able to fix it through an endoscope.
- 63. Colon cancer
- 64. • Colon cancer is cancer of the large intestine (colon), which is the final part of digestive tract.
- 65. • Most cases of colon cancer begin as small, noncancerous (benign) c l u m p s o f c e l l s c a l l e d adenomatous polyps. Over time some of these polyps can become colon cancers.
- 66. Causes In most cases, it's not clear what causes colon cancer. Inherited gene mutations that increase the risk of colon cancer Inherited gene mutations that increase the risk of colon cancer can be passed through families, but these inherited genes are linked to only a small percentage of colon cancers..
- 67. The most common forms of inherited colon cancer syndromes are: • Hereditary nonpolyposis colorectal cancer (HNPCC). HNPCC, also called Lynch syndrome, increases the risk of colon cancer and other cancers. People with HNPCC tend to develop colon cancer before age 50.
- 68. • Familial adenomatous polyposis (FAP). FAP is a rare disorder that causes to develop thousands of polyps in the lining of colon and rectum. People with untreated FAP have a greatly increased risk of developing colon cancer before age 40.
- 69. Association between diet and increased colon cancer risk Studies of large groups of people have shown an association between a typical Western diet and an increased risk of colon cancer. A typical Western diet is high in fat and low in fiber.
- 70. Risk factors Factors that may increase your risk of colon cancer include: • Older age. The great majority of people diagnosed with colon cancer are older than 50. • African-American race. African-Americans have a greater risk of colon cancer than do people of other races.
- 71. • A personal history of colorectal cancer or polyps. If already had colon cancer or adenomatous polyps, have a greater risk of colon cancer in the future. • Inflammatory intestinal conditions. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn's disease, can increase risk of colon cancer.
- 72. • Family history of colon cancer. • Low-fiber, high-fat diet. Colon cancer and rectal cancer may be associated with a diet low in fiber and high in fat and calories. Some studies have found an increased risk of colon cancer in people who eat diets high in red meat and processed meat.
- 73. • Smoking. People who smoke may have an increased risk of colon cancer. • Alcohol. Heavy use of alcohol increases risk of colon cancer. • Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers increases the risk of colon and rectal cancer.
- 74. Pathophysiology of cancer Carcinogens Alteration in the genetic structure of the cellular DNA Defective cellular proliferation and defective cellular differentiation Cancer development
- 75. Symptoms Signs and symptoms of colon cancer include: • A change in bowel habits, including diarrhea or constipation or a change in the consistency of stool, that lasts longer than four weeks • Rectal bleeding or blood in stool
- 76. • Persistent abdominal discomfort, such as cramps, gas or pain • A feeling that bowel doesn't empty completely • Weakness or fatigue • Unexplained weight loss
- 77. Diagnosing colon cancer • Using a scope to examine the inside of colon. Colonoscopy uses a long, flexible and slender tube attached to a video camera and monitor to view entire colon and rectum.
- 78. • Blood tests. Doctor may test blood for a chemical sometimes produced by colon cancers (carcinoembryonic antigen or CEA).
- 79. Treatment Surgery for early-stage colon cancer If colon cancer is very small, doctor may recommend a minimally invasive approach to surgery, such as: • Removing polyps during a colonoscopy. If cancer is small, localized and completely contained within a polyp and in a very early stage, doctor may be able to remove it completely during a colonoscopy.
- 80. • Endoscopic mucosal resection. Removing larger polyps may require also taking a small amount of the lining of the colon or rectum in a procedure called an endoscopic mucosal resection.
- 81. • Minimally invasive surgery. Polyps that can't be removed during a colonoscopy may be removed using laparoscopic surgery. In this procedure, surgeon performs the operation through several small incisions in abdominal wall, inserting instruments with attached cameras that display colon on a video monitor. The surgeon may also take samples from lymph nodes in the area where the cancer is located.
- 82. Surgery for invasive colon cancer If the cancer has grown into or through colon, surgeon may recommend: • Partial colectomy. During this procedure, the surgeon removes the part of colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. Surgeon is often able to reconnect the healthy portions of colon or rectum.
- 83. • Surgery to create a way for waste to leave body. When it's not possible to reconnect the healthy portions of colon or rectum, may need an ostomy. This involves creating an opening in the wall of abdomen from a portion of the remaining bowel for the elimination of stool into a bag that fits securely over the opening.
- 84. •Chemotherapy •Radiation therapy •Immunotherapy •Bone marrow transplantation •Stem cell research •Hospice
- 85. Nursing diagnosis Based on the assessment data, nursing diagnosis of the patient with cancer may include the following 1. Impaired tissue integrity (oral mucus membranes, alopecia, malignant skin lesions) related to the effect of treatment and disease 2. Imbalanced nutrition less than the body requirements related to anorexia or malabsorption or increased demand. 3. Pain or chronic pain related to disease and treatment effect. 4. Fatigue related to physical and psychological stressors
- 86. 5. Disturbed body image related to changes in appearance and role of function. 6. Anticipatory grieving related to expected loss and altered role function Nursing interventions • Maintaining tissue integrity • Addressing alopecia • Managing malignant skin lesions • Promoting nutrition • Relieving pain • Decreasing fatigue • Improving body image and self esteem
- 87. • Assisting grieving • Monitoring and managing potential complications • Managing bleeding.
