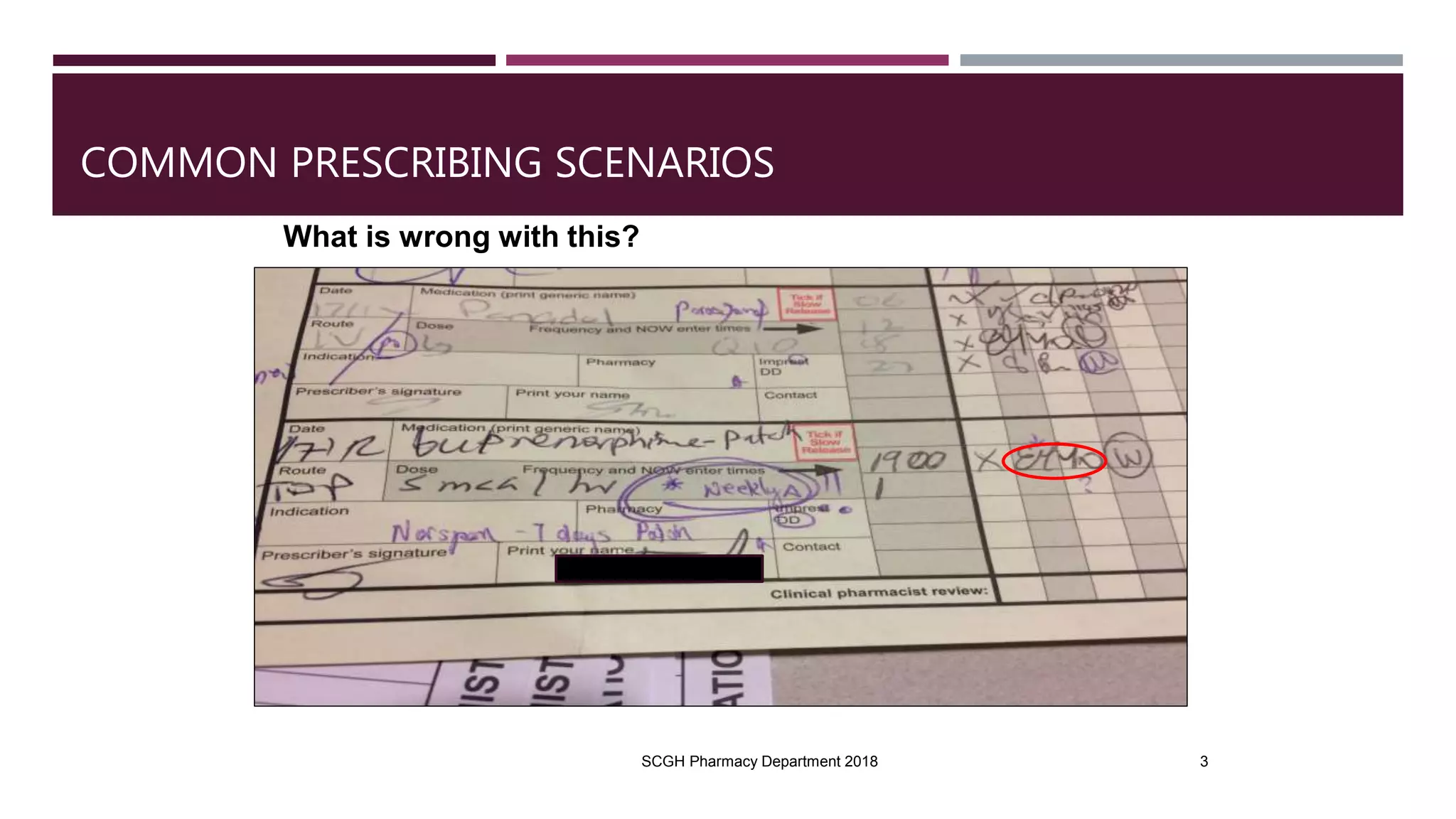
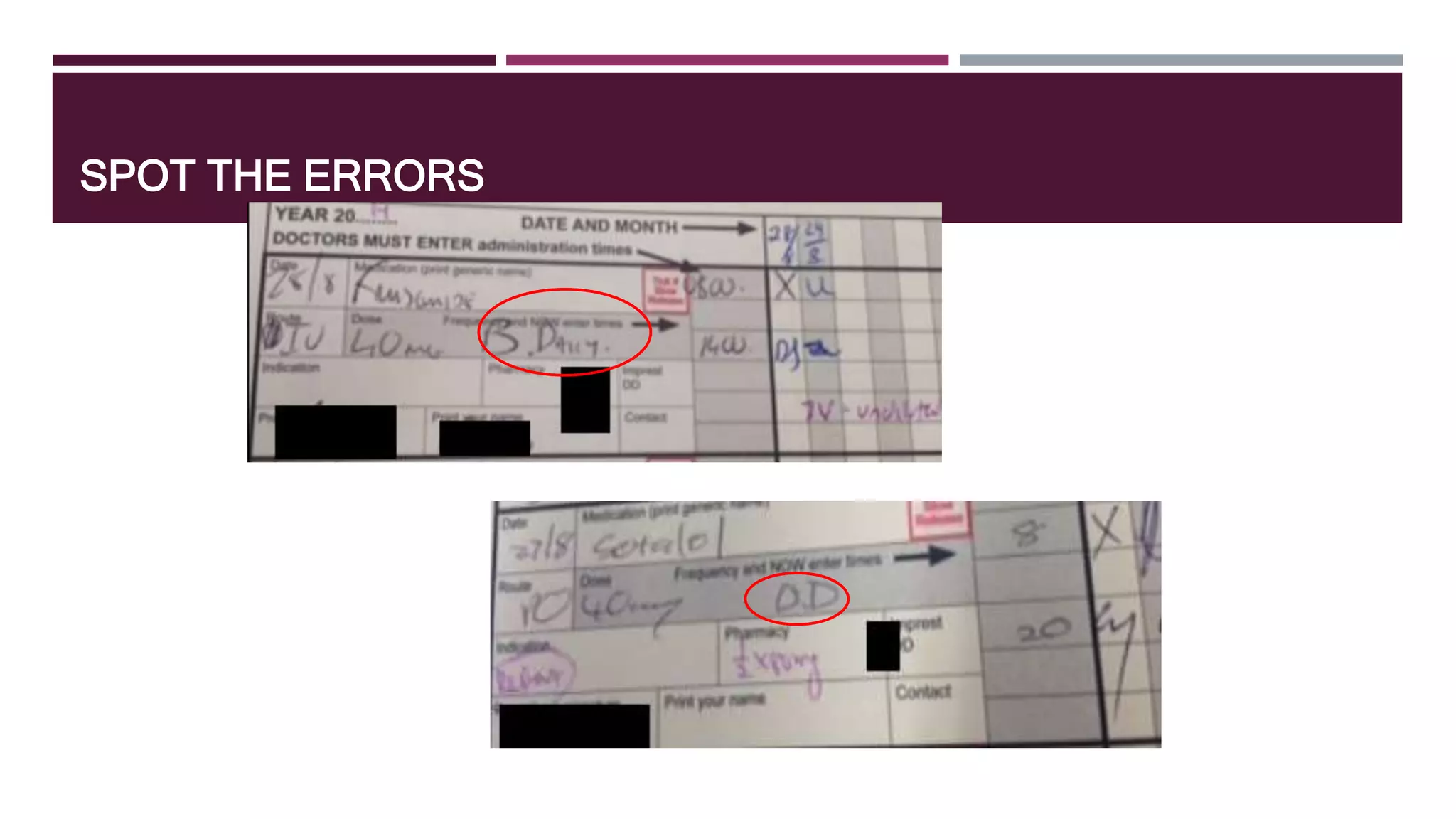
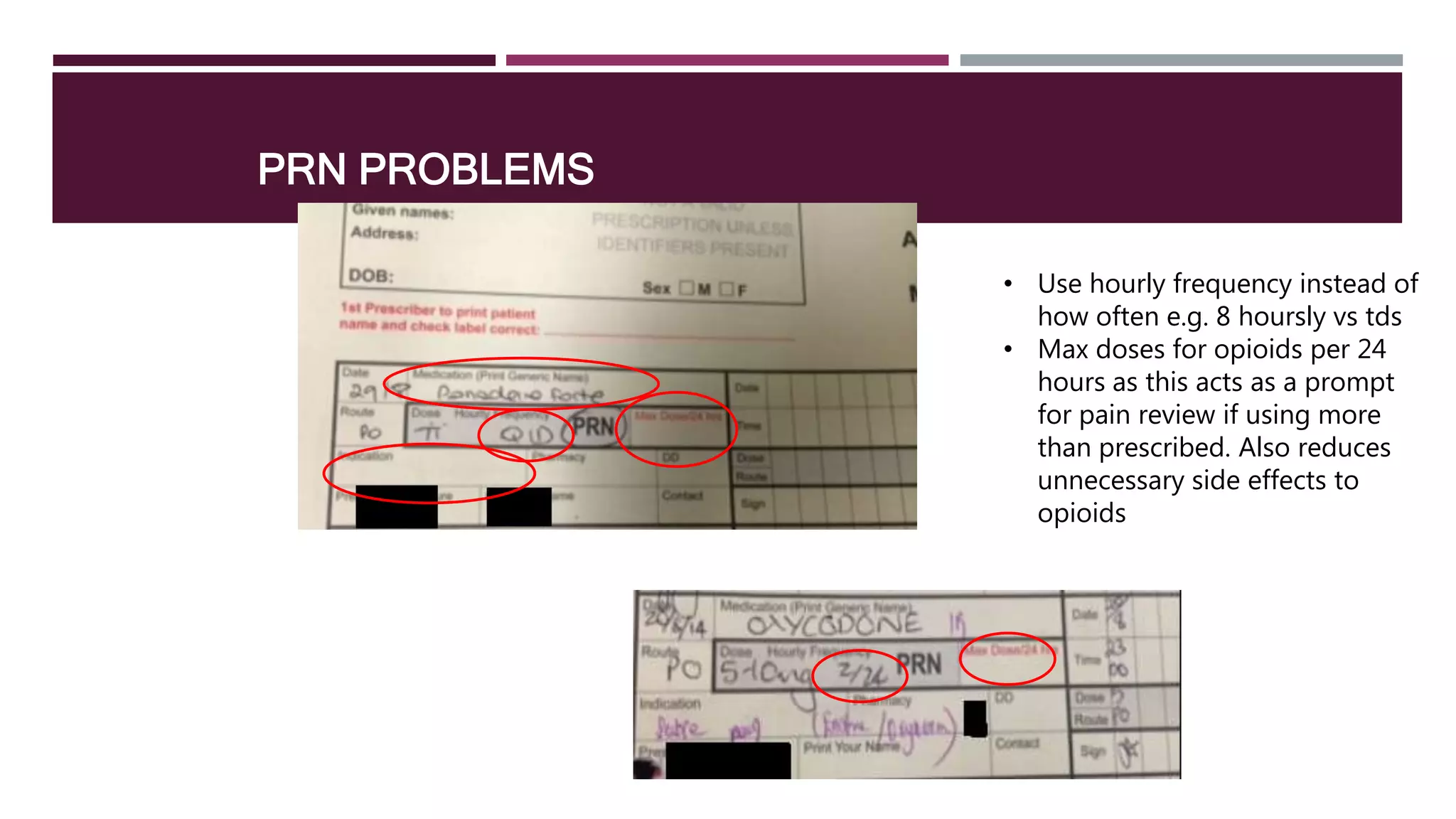
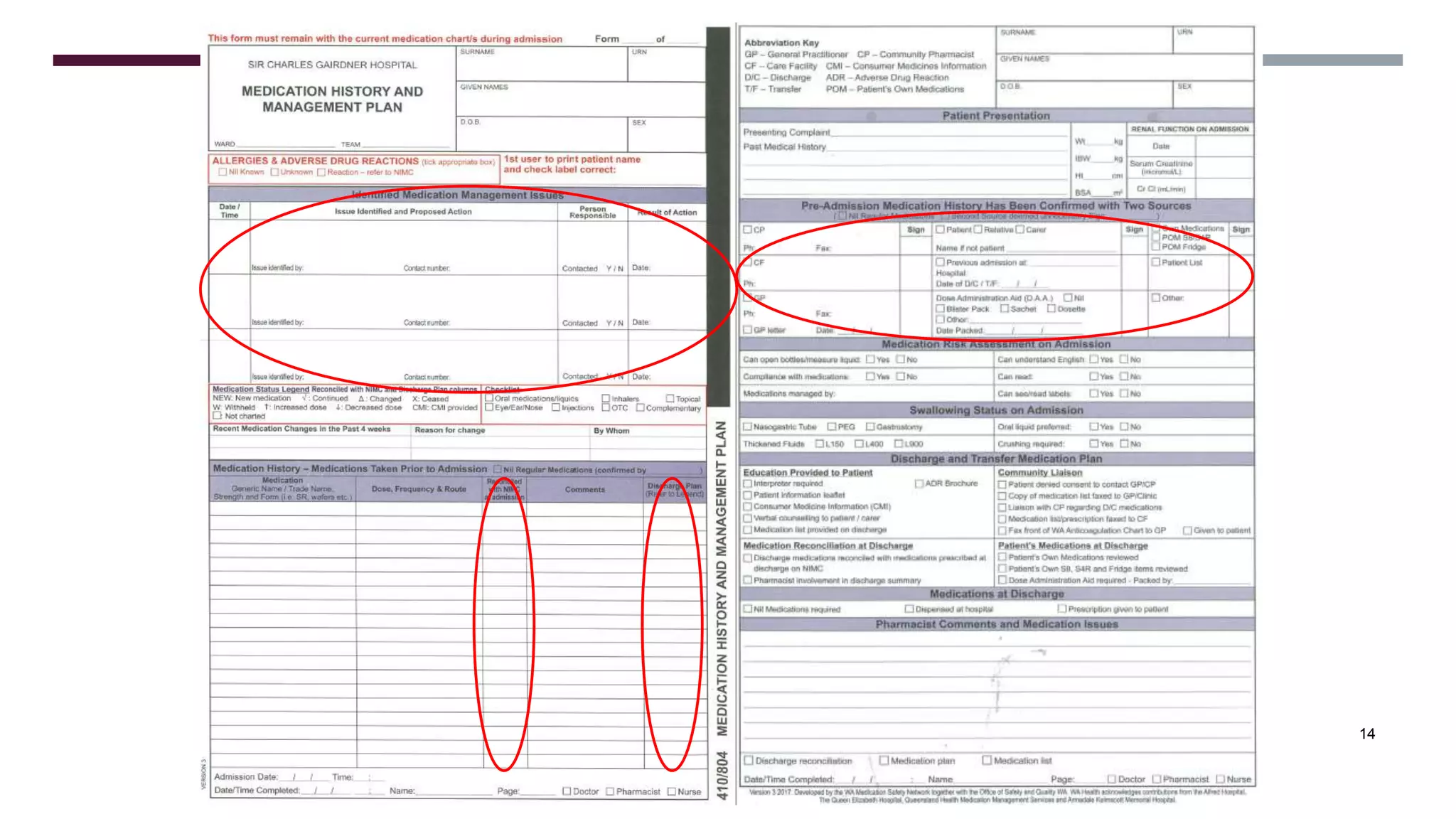
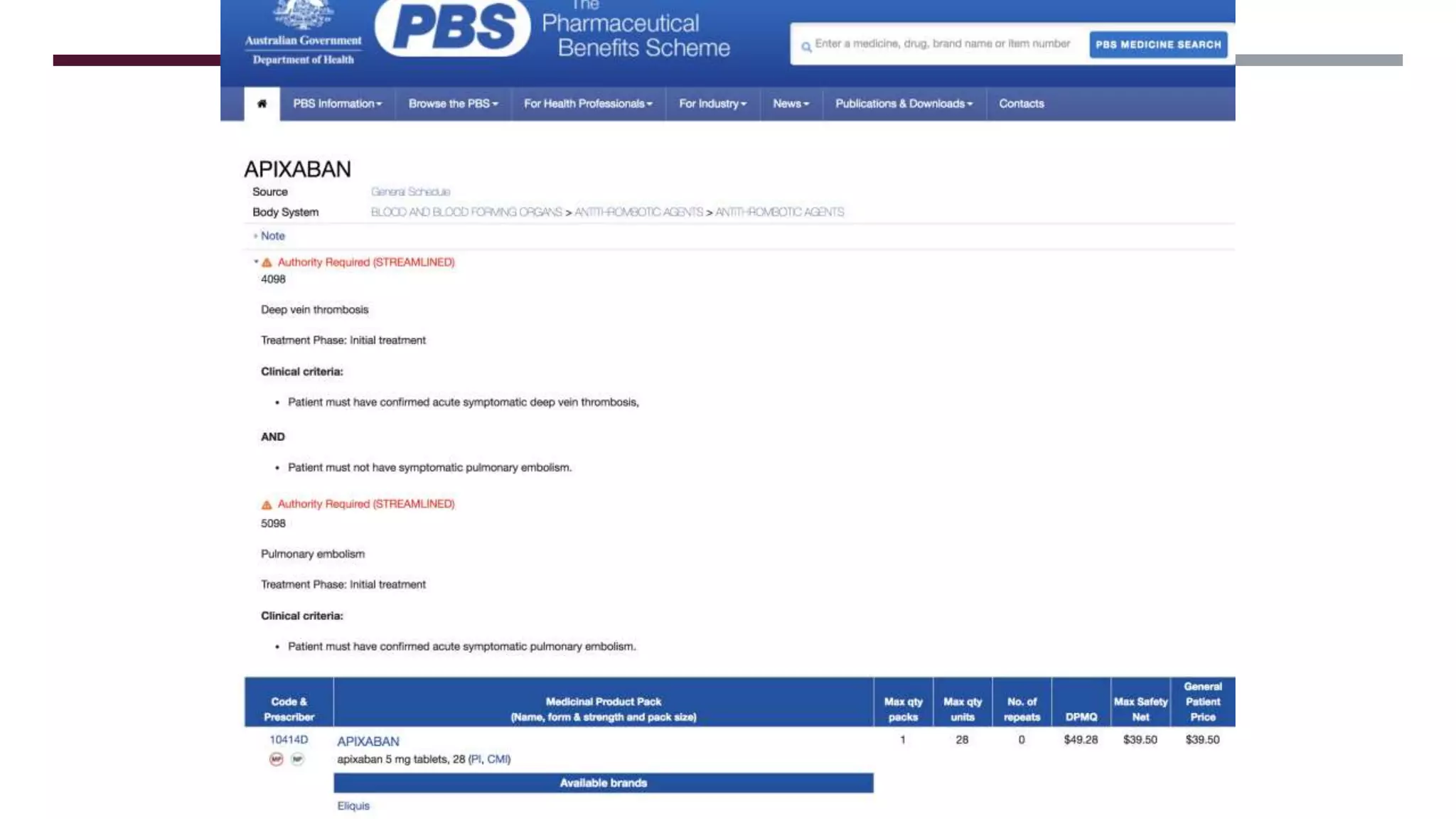
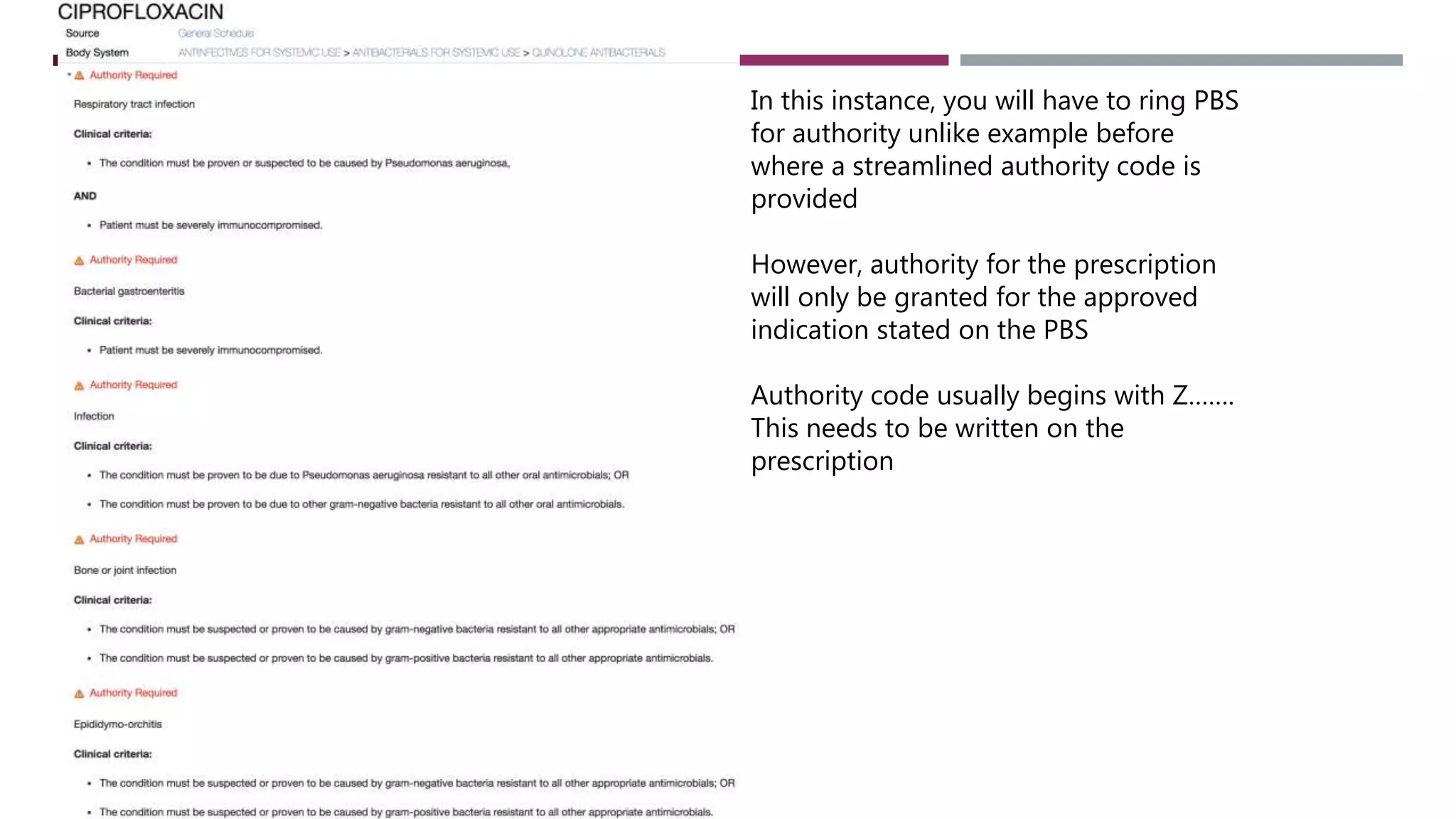
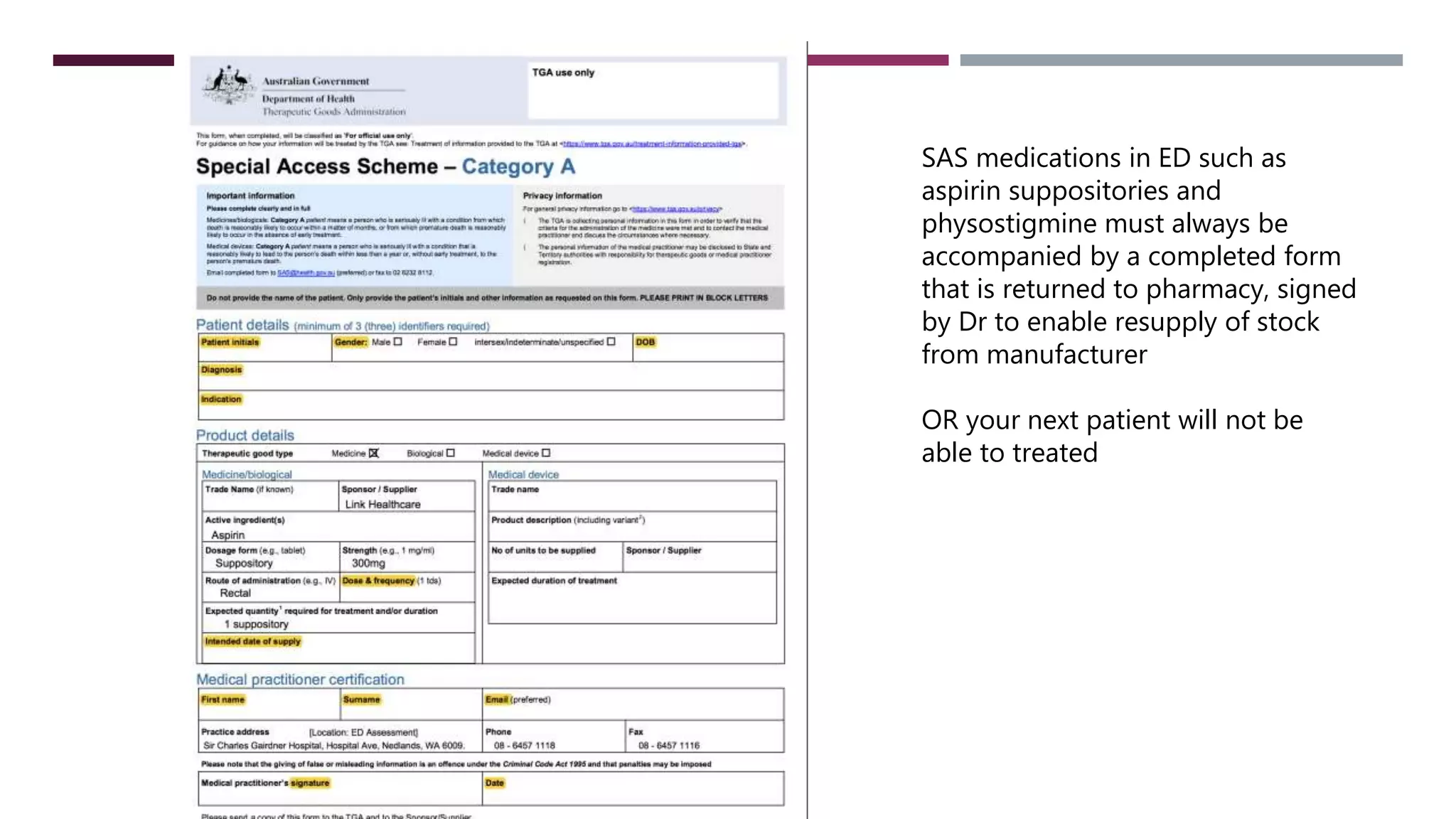
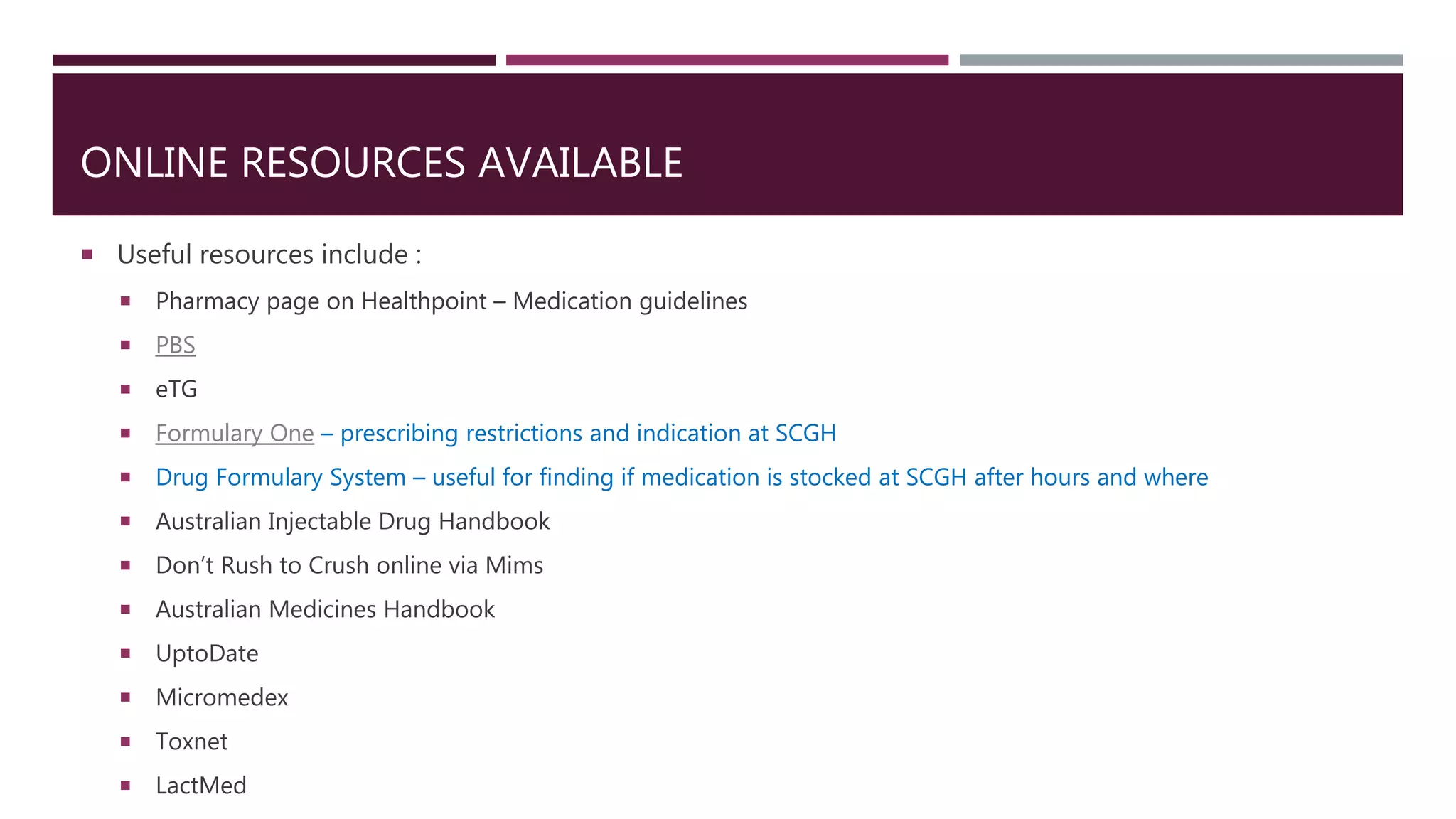
This document provides guidance on common prescribing scenarios for doctors in the emergency department at SCGH. It addresses topics such as taking an accurate medication history, discharging patients with medications, prescribing under the Pharmaceutical Benefits Scheme, and accessing online prescribing resources. Specific high-risk medications, patient populations, and clinical situations are also discussed.